Abstract
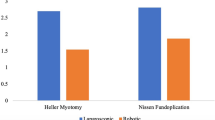
Minimally invasive surgery (MIS) has improved surgical access to the foregut. While the benefits of MIS versus open surgery are well accepted, the relative benefits of laparoscopic versus robotic approaches continue to be debated. Procedure-specific comparisons are difficult to obtain for Heller myotomy, due to the relative rarity of the procedure in most practices. A retrospective review of prospectively collected perioperative data of a single surgical practice from 2001 to 2019 was conducted for the rate of perforation during Heller myotomy laparoscopically compared to robotically. From 2001 through February 2012, a laparoscopic approach was employed and from October 2008 to 2019, a robotic approach was employed. All perforations were recorded, as well as secondary outcomes of perforation location (gastric or esophageal), postoperative imaging for evidence of leak, length of stay, and complications. Chi-square and simple t test were employed for data analysis. During the 11 years of laparoscopic Heller myotomy, 14 cases resulted in 7 instances of perforation (50%). During the 11 years of robotic Heller myotomy, 45 cases resulted in 11 instances of perforation (24%) (p value = 0.06). All perforations in both groups were tiny, recognized, and repaired immediately. The length of stay (LOS) was longer in the laparoscopic perforation group (3.4 days) compared to the laparoscopic non-perforation group (1.2 days) (p value = 0.06). LOS for robotic was not significantly longer in the perforation group (2.8 days) compared to the robotic non-perforation group (1.5 days) (p value = 0.18). First time Heller myotomies showed a higher rate of perforation with laparoscopic (50%) vs robotic (14%) (p value = 0.009) approach. In subgroup analysis of revisional procedures, all ten were performed robotically (p value < 0.001) with a 60% perforation rate (p value = 0.001) and one associated, radiographically confirmed leak. Primary laparoscopic Heller myotomy related to more than four times the frequency of perforation than did primary robotic myotomy. We propose that the robotic platform provided the surgeon with superior ability to avoid perforation. Interestingly, the robotic group in this study dealt with more complex redo cases. In fact, reoperation in the area of the hiatus was a separate risk factor for perforation during robotic Heller myotomy. We recommend further prospective trials be done to better evaluate the benefits of robotic platform in regard to revisional foregut surgery.
Similar content being viewed by others
References
Markar SR, Karthikesalingam AP, Hagen ME, Talamini M, Horgan S, Wagner OJ (2010) Robotic vs. laparoscopic Nissen fundoplication for gastro-oesophageal reflux disease: systematic review and meta-analysis. Int J Med Robot Comput Assist Surg 6(2):125–131. https://doi.org/10.1002/rcs.309
Toro JP, Lin E, Patel AD (2014) Review of robotics in foregut and bariatric surgery. Surg Endosc. https://doi.org/10.1007/s00464-014-3646-z
Wilson EB (2009) The evolution of robotic general surgery. Scand J Surg 98(2):125–129. https://doi.org/10.1177/145749690909800208
Soliman BG, Nguyen DT, Chan EY et al (2020) Robot-assisted hiatal hernia repair demonstrates favorable short-term outcomes compared to laparoscopic hiatal hernia repair. Surg Endosc 34(6):2495–2502. https://doi.org/10.1007/s00464-019-07055-8
Melvin WS, Needleman BJ, Krause KR et al (2002) Computer-enhanced robotic telesurgery: initial experience in foregut surgery. Surg Endosc Other Interv Tech 16(12):1790–1792. https://doi.org/10.1007/s00464-001-8192-9
Ito F, Gould JC (2006) Robotic foregut surgery. Int J Med Robot Comput Assist Surg 2(4):287–292. https://doi.org/10.1002/rcs.108
Arora Z, Thota PN, Sanaka MR (2017) Achalasia: current therapeutic options. Ther Adv Chronic Dis 8(6–7):101–108. https://doi.org/10.1177/2040622317710010
Jeon HH, Kim JH, Youn YH, Park H, Conklin JL (2017) Clinical characteristics of patients with untreated achalasia. J Neurogastroenterol Motil 23(3):378–384. https://doi.org/10.5056/jnm16177
Burmeister S (2013) Review of current diagnosis and management of diffuse esophageal spasm, nutcracker esophagus/spastic nutcracker and hypertensive lower esophageal sphincter. Curr Opin Otolaryngol Head Neck Surg 21(6):543–547. https://doi.org/10.1097/MOO.0000000000000002
Almansa C, Hinder RA, Smith CD, Achem SR (2008) A comprehensive appraisal of the surgical treatment of diffuse esophageal spasm. J Gastrointest Surg 12(6):1133–1145. https://doi.org/10.1007/s11605-007-0439-x
Roman S, Huot L, Zerbib F et al (2016) High-resolution manometry improves the diagnosis of esophageal motility disorders in patients with dysphagia: a randomized multicenter study. Am J Gastroenterol 111(3):372–380. https://doi.org/10.1038/ajg.2016.1
Oude Nijhuis RAB, Zaninotto G, Roman S et al (2020) European Guideline on Achalasia—UEG and ESNM recommendations. United Eur Gastroenterol J 8(1):13–34. https://doi.org/10.1177/2050640620903213
Chrystoja CC, Darling GE, Diamant NE et al (2016) Achalasia-specific quality of life after pneumatic dilation or laparoscopic heller myotomy with partial fundoplication: a multicenter, randomized clinical trial. Am J Gastroenterol 111(11):1536–1545. https://doi.org/10.1038/ajg.2016.402
Persson J, Johnsson E, Kostic S, Lundell L, Smedh U (2015) Treatment of achalasia with laparoscopic myotomy or pneumatic dilatation: long-term results of a prospective, randomized study. World J Surg 39(3):713–720. https://doi.org/10.1007/s00268-014-2869-4
Zaninotto G, Annese V, Costantini M et al (2004) Randomized controlled trial of botulinum toxin versus laparoscopic heller myotomy for esophageal Achalasia. Ann Surg 239(3):364–370. https://doi.org/10.1097/01.sla.0000114217.52941.c5
Bello B, Herbella FA, Allaix ME, Patti MG (2012) Impact of minimally invasive surgery on the treatment of benign esophageal disorders. World J Gastroenterol 18(46):6764–6770. https://doi.org/10.3748/wjg.v18.i46.6764
Schuchert MJ, Luketich JD, Landreneau RJ et al (2008) Minimally-invasive esophagomyotomy in 200 consecutive patients: factors influencing postoperative outcomes. Ann Thorac Surg 85(5):1729–1734. https://doi.org/10.1016/j.athoracsur.2007.11.017
Melvin WS, Needleman BJ, Krause KR, Wolf RK, Michler RE, Ellison EC (2001) Computer-assisted robotic Heller myotomy: initial case report. J Laparoendosc Adv Surg Tech Part A 11(4):251–253. https://doi.org/10.1089/109264201750539790
Maeso S, Reza M, Mayol JA et al (2010) Efficacy of the da vinci surgical system in abdominal surgery compared with that of laparoscopy: a systematic review and meta-analysis. Ann Surg 252(2):254–262. https://doi.org/10.1097/SLA.0b013e3181e6239e
Perry KA, Kanji A, Drosdeck JM et al (2014) Efficacy and durability of robotic heller myotomy for achalasia: patient symptoms and satisfaction at long-term follow-up. Surg Endosc 28(11):3162–3167. https://doi.org/10.1007/s00464-014-3576-9
Shaligram A, Unnirevi J, Simorov A, Kothari VM, Oleynikov D (2012) How does the robot affect outcomes? A retrospective review of open, laparoscopic, and robotic Heller myotomy for achalasia. Surg Endosc 26(4):1047–1050. https://doi.org/10.1007/s00464-011-1994-5
Horgan S, Galvani C, Gorodner MV et al (2005) Robotic-assisted Heller myotomy versus laparoscopic Heller myotomy for the treatment of esophageal achalasia: multicenter study. J Gastrointest Surg 9(8):1020–1030. https://doi.org/10.1016/j.gassur.2005.06.026
Galvani C, Gorodner MV, Moser F, Baptista M, Donahue P, Horgan S (2006) Laparoscopic Heller myotomy for achalasia facilitated by robotic assistance. Surg Endosc Other Interv Tech 20(7):1105–1112. https://doi.org/10.1007/s00464-005-0272-9
Heller E (1913) Extramucöse cardioplastie beim chronischen cardiospasmus mit dilatation des oesophagus. Mitt Grengeb Med Chir 2:141–149
Falkenback D, Lehane CW, Lord RVN (2015) Robot-assisted oesophageal and gastric surgery for benign disease: antireflux operations and Heller’s myotomy. ANZ J Surg 85(3):113–120. https://doi.org/10.1111/ans.12731
Huffmanm LC, Pandalai PK, Boulton BJ et al (2007) Robotic Heller myotomy: a safe operation with higher postoperative quality-of-life indices. Surgery 142(4):613–620. https://doi.org/10.1016/j.surg.2007.08.003
Rossetti G, del Genio G, Maffettone V et al (2009) Laparoscopic reoperation with total fundoplication for failed Heller myotomy: is it a possible option? Personal experience and review of literature. Int Surg 94(4):330–334
Rakita S, Bloomston M, Villadolid D, Thometz D, Zervos E, Rosemurgy A (2005) Esophagotomy during laparoscopic Heller myotomy cannot be predicted by preoperative therapies and does not influence long-term outcome. J Gastrointest Surg 9:159–164. https://doi.org/10.1016/j.gassur.2004.10.015
Horgan S, Hudda K, Eubanks T, McAllister J, Pellegrini CA (1999) Does botulinum toxin injection make esophagomyotomy a more difficult operation? Surg Endosc 13(6):576–579. https://doi.org/10.1007/s004649901044
Patti MG, Feo CV, Arcerito M et al (1999) Effects of previous treatment on results of laparoscopic Heller myotomy for achalasia. Dig Dis Sci 44(11):2270–2276. https://doi.org/10.1023/A:1026660921776
Sharp KW, Khaitan L, Scholz S, Holzman MD, Richards WO (2002) 100 Consecutive minimally invasive heller myotomies: lessons learned. Ann Surg 235(5):631–639. https://doi.org/10.1097/00000658-200205000-00004
Ponce J, Juan M, Garrigues V, Pascual S, Berenguer J (1999) Efficacy and safety of cardiomyotomy in patients with achalasia after failure of pneumatic dilatation. Dig Dis Sci 44(11):2277–2282. https://doi.org/10.1023/A:1026613005846
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Abigail Engwall-Gill and Dr. Tahereh Soliemani have no conflicts of interest or financial ties to disclose. Dr. Sandra Engwall has been a robotic proctor for Intuitive.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Engwall-Gill, A.J., Soleimani, T. & Engwall, S.S. Heller myotomy perforation: robotic visualization decreases perforation rate and revisional surgery is a perforation risk. J Robotic Surg 16, 867–873 (2022). https://doi.org/10.1007/s11701-021-01307-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-021-01307-3