Abstract
Open inguinal lymph node dissection (O-ILND) is the gold standard in the management of lymph nodes in carcinoma penis; however, video endoscopic inguinal lymphadenectomy (VEIL) is performed in some centers. Our primary objective is to compare perioperative and survival outcomes in patients undergoing VEIL with O-ILND, as very few studies have reported long-term survival outcomes till date. We analyzed patients who underwent O-ILND and VEIL (laparoscopic or robot-assisted) from January 2009 to January 2020 in our institute for carcinoma of the penis. Patient details, perioperative complications, and survival outcomes were analyzed. Perioperative outcomes were analyzed by logistic regression and survival outcomes by log-rank and Cox regression methods. We analyzed 79 patients (32 O-ILND, 47 VEIL) with a median follow-up of 51 (IQR 25.5–75.5) and 42 months (IQR 21–62). Wound complications were common in O-ILND group (65.6%) compared to VEIL group (27.7%) (p = 0.001), predominantly skin flap necrosis in 14 groins (23.73%) after O-ILND and none after VEIL. Median overall survival was 80 and 88 months (p = 0.840) with five-year survival of 65% and 66.8% (p = 0.636) and five-year DSS of 76.6% and 73.9% (p = 0.96) in O-ILND and VEIL, respectively. Multivariate analysis showed that grade and pathological node status were significant (HR-2.650, p = 0.040; HR-3.218, p = 0.024) factors for survival. The retrospective nature of the study design is the limitation. Management of inguinal lymph nodes in carcinoma penis by VEIL is safe, associated with lesser wound-related complications, and equivalent survival outcomes compared to O-ILND. It should be considered as an alternative option for inguinal lymph node dissection.

Similar content being viewed by others
Data availability
Yes (with the corresponding author).
References
Wang S, Du P, Tang X et al (2017) Comparison of efficiency of video endoscopy and open inguinal lymph node dissection. Anticancer Res 37:4623–4628
Syed S, Eng TY, Thomas CR et al (2003) Current issues in the management of advanced squamous cell carcinoma of the penis. Urol Oncol 21:431–438. https://doi.org/10.1016/s1078-1439(03)00058-9
Sánchez-Ortiz RF, Pettaway CA (2004) The role of lymphadenectomy in penile cancer. Urol Oncol. https://doi.org/10.1016/j.urolonc.2004.04.031
Niyogi D, Noronha J, Pal M et al (2020) Management of clinically node-negative groin in patients with penile cancer. Indian J Urol 36:8–15. https://doi.org/10.4103/iju.IJU_221_19
Bevan-Thomas R, Slaton JW, Pettaway CA (2002) Contemporary morbidity from lymphadenectomy for penile squamous cell carcinoma: the M.D. Anderson Cancer Center Experience J Urol 167:1638–1642
Protzel C, Alcaraz A, Horenblas S et al (2009) Lymphadenectomy in the surgical management of penile cancer. Eur Urol 55:1075–1088. https://doi.org/10.1016/j.eururo.2009.02.021
Hinten F, van den Einden LCG, Hendriks JCM et al (2011) Risk factors for short- and long-term complications after groin surgery in vulvar cancer. Br J Cancer 105:1279–1287. https://doi.org/10.1038/bjc.2011.407
Spiess PE, Hernandez MS, Pettaway CA (2009) Contemporary inguinal lymph node dissection: minimizing complications. World J Urol 27:205–212. https://doi.org/10.1007/s00345-008-0324-6
Leijte JAP, Kirrander P, Antonini N et al (2008) Recurrence patterns of squamous cell carcinoma of the penis: recommendations for follow-up based on a two-centre analysis of 700 patients. Eur Urol 54:161–168. https://doi.org/10.1016/j.eururo.2008.04.016
Koifman L, Hampl D, Koifman N et al (2013) Radical open inguinal lymphadenectomy for penile carcinoma: surgical technique, early complications and late outcomes. J Urol 190:2086–2092. https://doi.org/10.1016/j.juro.2013.06.016
Daseler EH, Anson BJ, Reimann AF (1948) Radical excision of the inguinal and iliac lymph glands; a study based upon 450 anatomical dissections and upon supportive clinical observations. Surg Gynecol Obstet 87:679–694
Stuiver MM, Djajadiningrat RS, Graafland NM et al (2013) Early wound complications after inguinal lymphadenectomy in penile cancer: a historical cohort study and risk-factor analysis. Eur Urol 64:486–492. https://doi.org/10.1016/j.eururo.2013.02.037
Tobias-Machado M, Tavares A, Silva MNR et al (2008) Can video endoscopic inguinal lymphadenectomy achieve a lower morbidity than open lymph node dissection in penile cancer patients? J Endourol 22:1687–1691. https://doi.org/10.1089/end.2007.0386
Bishoff JT, Lackland AFB, Basler JW, Teichman JM and ThompsonIM: Endoscopic subcutaneous modified inguinal lymph node dissection (ESMIL) for squamous cell carcinoma of the penis. J Urol, suppl., 2003; 169: 78, abstract 301
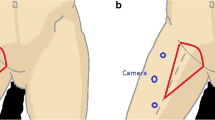
Tobias-Machado M, Tavares A, Ornellas AA et al (2007) Video endoscopic inguinal lymphadenectomy: a new minimally invasive procedure for radical management of inguinal nodes in patients with penile squamous cell carcinoma. J Urol. https://doi.org/10.1016/j.juro.2006.10.075
Josephson DY, Jacobsohn KM, Link BA, Wilson TG (2009) Robotic-assisted Endoscopic Inguinal Lymphadenectomy. Urology 73:167–170. https://doi.org/10.1016/j.urology.2008.05.060
Amitabh S, Jiten J, Amit G et al (2018) Comparing outcomes of robotic and open inguinal lymph node dissection in patients with carcinoma of the penis. J Urol 199:1518–1525. https://doi.org/10.1016/j.juro.2017.12.061
Hu J, Li H, Cui Y et al (2019) Comparison of clinical feasibility and oncological outcomes between video endoscopic and open inguinal lymphadenectomy for penile cancer. Medicine. https://doi.org/10.1097/MD.0000000000015862
Schwentner C, Todenhöfer T, Seibold J et al (2013) Endoscopic inguinofemoral lymphadenectomy–extended follow-up. J Endourol 27:497–503. https://doi.org/10.1089/end.2012.0489
d’Ancona CAL, de Lucena RG, de Querne FA et al (2004) Long-term followup of penile carcinoma treated with penectomy and bilateral modified inguinal lymphadenectomy. J Urol. https://doi.org/10.1097/01.ju.0000132239.28989.e1
Kumar V, Sethia KK (2017) Prospective study comparing video-endoscopic radical inguinal lymph node dissection (VEILND) with open radical ILND (OILND) for penile cancer over an 8-year period. BJU Int 119:530–534. https://doi.org/10.1111/bju.13660
Thyavihally Y, Tongaonkar H (2008) VID.03: video endoscopic inguinal lymphadenectomy (VEIL): our initial experience. Urology 72:S106–S107. https://doi.org/10.1016/j.urology.2008.08.310
Yadav SS, Tomar V, Bhattar R et al (2018) Video endoscopic inguinal lymphadenectomy vs open inguinal lymphadenectomy for carcinoma penis: expanding role and comparison of outcomes. Urology 113:79–84. https://doi.org/10.1016/j.urology.2017.11.007
Ye Y-L, Guo S-J, Li Z-S et al (2018) Radical videoscopic inguinal lymphadenectomies: a matched pair analysis. J Endourol 32:955–960. https://doi.org/10.1089/end.2018.0356
Novara G, Galfano A, De Marco V et al (2007) Prognostic factors in squamous cell carcinoma of the penis. Nature Clin Prac Urol 4:140–146. https://doi.org/10.1038/ncpuro0751
Pandey D, Mahajan V, Kannan RR (2006) Prognostic factors in node-positive carcinoma of the penis. J Surg Oncol 93:133–138. https://doi.org/10.1002/jso.20414
Soria JC, Fizazi K, Piron D et al (1997) Squamous cell carcinoma of the penis: multivariate analysis of prognostic factors and natural history in monocentric study with a conservative policy. Ann Oncol 8:1089–1098. https://doi.org/10.1023/a:1008248319036
Shah AA, Shah HA, Panjwani GN et al (2016) Prognostic factors and 5-year survival of patients with carcinoma penis: tertiary health center study. Indian J Cancer 53:309–312. https://doi.org/10.4103/0019-509X.197729
Funding
No funding.
Author information
Authors and Affiliations
Contributions
All authors critically revised the paper for important intellectual content. All authors have contributed to the work and agreed on the final version. This manuscript is not being considered by any other journal.
Corresponding author
Ethics declarations
Conflict of interest
Yuvaraja B Thyavihally, Preetham Dev, Santosh S Waigankar, Abhinav Pednekar, Bijal Kulkarni, Anshu Sharma, Sharad Maheshwari, Diptiman Roy, Varun Agarwal, Archan A Khandekar, Naresh D Badlani, Ashish N Asari, and Neha Sanwalka declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving humans were in accordance with the ethical standards of the institutional research committee and the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed written consent for the surgery was obtained, but consent for inclusion in the study is not taken as it is a retrospective study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Thyavihally, Y.B., Dev, P., Waigankar, S.S. et al. Comparative study of perioperative and survival outcomes after video endoscopic inguinal lymphadenectomy (VEIL) and open inguinal lymph node dissection (O-ILND) in the management of inguinal lymph nodes in carcinoma of the penis. J Robotic Surg 15, 905–914 (2021). https://doi.org/10.1007/s11701-020-01189-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-020-01189-x