Abstract
Purpose
Bariatric surgery is associated with a greater venous thromboembolism (VTE) risk in the weeks following surgery, but the long-term risk of VTE is incompletely characterized. We evaluated bariatric surgery in relation to long-term VTE risk.
Materials and Methods
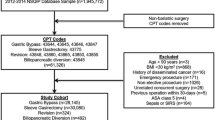
This population-based retrospective matched cohort study within three United States–based integrated health care systems included adults with body mass index (BMI) ≥ 35 kg/m2 who underwent bariatric surgery between January 2005 and September 2015 (n = 30,171), matched to nonsurgical patients on site, age, sex, BMI, diabetes, insulin use, race/ethnicity, comorbidity score, and health care utilization (n = 218,961). Follow-up for incident VTE ended September 2015 (median 9.3, max 10.7 years).
Results
Our population included 30,171 bariatric surgery patients and 218,961 controls; we identified 4068 VTE events. At 30 days post-index date, bariatric surgery was associated with a fivefold greater VTE risk (HRadj = 5.01; 95% CI = 4.14, 6.05) and a nearly fourfold greater PE risk (HRadj = 3.93; 95% CI = 2.87, 5.38) than no bariatric surgery. At 1 year post-index date, bariatric surgery was associated with a 48% lower VTE risk and a 70% lower PE risk (HRadj = 0.52; 95% CI = 0.41, 0.66 and HRadj = 0.30; 95% CI = 0.21, 0.44, respectively). At 5 years post-index date, lower VTE risks persisted, with bariatric surgery associated with a 41% lower VTE risk and a 55% lower PE risk (HRadj = 0.59; 95% CI = 0.48, 0.73 and HRadj = 0.45; 95% CI = 0.32, 0.64, respectively).
Conclusion
Although in the short-term bariatric surgery is associated with a greater VTE risk, in the long-term, it is associated with a substantially lower risk.
Graphical Abstract


Similar content being viewed by others
References
Finks JF, English WJ, Carlin AM, et al. Predicting risk for venous thromboembolism with bariatric surgery: results from the Michigan Bariatric Surgery Collaborative. Ann Surg. 2012;255(6):1100–4. https://doi.org/10.1097/SLA.0b013e31825659d4.
Froehling DA, Daniels PR, Mauck KF, et al. Incidence of venous thromboembolism after bariatric surgery: a population-based cohort study. Obes Surg. 2013;23(11):1874–9. https://doi.org/10.1007/s11695-013-1073-1.
Steele KE, Schweitzer MA, Prokopowicz G, et al. The long-term risk of venous thromboembolism following bariatric surgery. Obes Surg. 2011;21(9):1371–6. https://doi.org/10.1007/s11695-011-0445-7.
Stein PD, Matta F. Pulmonary embolism and deep venous thrombosis following bariatric surgery. Obes Surg. 2013;23(5):663–8. https://doi.org/10.1007/s11695-012-0854-2.
Winegar DA, Sherif B, Pate V, et al. Venous thromboembolism after bariatric surgery performed by Bariatric Surgery Center of Excellence Participants: analysis of the Bariatric Outcomes Longitudinal Database. Surg Obes Relat Dis. 2011;7(2):181–8. https://doi.org/10.1016/j.soard.2010.12.008.
Sweetland S, Green J, Liu B, et al. Duration and magnitude of the postoperative risk of venous thromboembolism in middle aged women: prospective cohort study. Bmj. 2009;339:b4583. https://doi.org/10.1136/bmj.b4583.
Mechanick JI, Apovian C, Brethauer S, et al. Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures - 2019 update: cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic and Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Obesity (Silver Spring). 2020;28(4):O1-o58. https://doi.org/10.1002/oby.22719.
Martin KA, Lee CR, Farrell TM, et al. Oral anticoagulant use after bariatric surgery: a literature review and clinical guidance. Am J Med. 2017;130(5):517–24. https://doi.org/10.1016/j.amjmed.2016.12.033.
Martin KA, Beyer-Westendorf J, Davidson BL, et al. Use of direct oral anticoagulants in patients with obesity for treatment and prevention of venous thromboembolism: updated communication from the ISTH SSC Subcommittee on Control of Anticoagulation. J Thromb Haemost. 2021;19(8):1874–82. https://doi.org/10.1111/jth.15358.
White RH. The epidemiology of venous thromboembolism. Circulation. 2003;107(23 Suppl 1):I4-8. https://doi.org/10.1161/01.cir.0000078468.11849.66.
Lutsey PL, Zakai NA. Epidemiology and prevention of venous thromboembolism. Nat Rev Cardiol. 2023;20(4):248–62. https://doi.org/10.1038/s41569-022-00787-6.
Stein PD, Beemath A, Olson RE. Obesity as a risk factor in venous thromboembolism. Am J Med. 2005;118(9):978–80. https://doi.org/10.1016/j.amjmed.2005.03.012.
Mahmoodi BK, Cushman M, Anne Naess I, et al. Association of traditional cardiovascular risk factors with venous thromboembolism: an individual participant data meta-analysis of prospective studies. Circulation. 2017;135(1):7–16. https://doi.org/10.1161/circulationaha.116.024507.
Moussa O, Ardissino M, Tang A, et al. Long-term impact of bariatric surgery on venous thromboembolic risk: a matched cohort study. Ann Surg. 2019. https://doi.org/10.1097/sla.0000000000003750.
Arterburn DE, Johnson E, Coleman KJ, et al. Weight outcomes of sleeve gastrectomy and gastric bypass compared to nonsurgical treatment. Ann Surg. 2021;274(6):e1269–76. https://doi.org/10.1097/sla.0000000000003826.
Courcoulas AP, Johnson E, Arterburn DE, et al. Reduction in long-term mortality after sleeve gastrectomy and gastric bypass compared to nonsurgical patients with severe obesity. Ann Surg. 2023;277(3):442–8. https://doi.org/10.1097/sla.0000000000005155.
Center for Disease Control and Prevention. Defining adult overweight & obesity 2023 [cited 2023 October 29]. Available from: https://www.cdc.gov/obesity/basics/adult-defining.html#:~:text=Obesity%20is%20frequently%20subdivided%20into,BMI%20of%2040%20or%20higher
Fisher DP, Johnson E, Haneuse S, et al. Association between bariatric surgery and macrovascular disease outcomes in patients with type 2 diabetes and severe obesity. JAMA. 2018;320(15):1570–82. https://doi.org/10.1001/jama.2018.14619.
O’Brien R, Johnson E, Haneuse S, et al. Microvascular outcomes in patients with diabetes after bariatric surgery versus usual care: a matched cohort study. Ann Intern Med. 2018;169(5):300–10. https://doi.org/10.7326/m17-2383.
Li RA, Liu L, Arterburn D, et al. Five-year longitudinal cohort study of reinterventions after sleeve gastrectomy and Roux-en-Y gastric bypass. Ann Surg. 2021;273(4):758–65. https://doi.org/10.1097/sla.0000000000003401.
Gagne JJ, Glynn RJ, Avorn J, et al. A combined comorbidity score predicted mortality in elderly patients better than existing scores. J Clin Epidemiol. 2011;64(7):749–59. https://doi.org/10.1016/j.jclinepi.2010.10.004.
Mahalanobis PC. On the generalized distance in statistics. Proc Natl Acad Sci India. 1936;2:49–55.
VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268–74. https://doi.org/10.7326/m16-2607.
Haneuse S, VanderWeele TJ, Arterburn D. Using the E-value to assess the potential effect of unmeasured confounding in observational studies. JAMA. 2019;321(6):602–3. https://doi.org/10.1001/jama.2018.21554.
Folsom AR, Cushman M. Exploring opportunities for primary prevention of unprovoked venous thromboembolism: ready for prime time? J Am Heart Assoc. 2020;9(23):e019395. https://doi.org/10.1161/jaha.120.019395.
Schauer DP, Feigelson HS, Koebnick C, et al. Bariatric surgery and the risk of cancer in a large multisite cohort. Ann Surg. 2019;269(1):95–101. https://doi.org/10.1097/sla.0000000000002525.
Pahlkotter MK, Mohidul S, Moen MR, et al. BMI and VTE risk in emergency general surgery, does size matter? : An ACS-NSQIP database analysis. Am Surg. 2020;86(12):1660–5. https://doi.org/10.1177/0003134820940272.
Zhang ZH, Shen B, Yang J, et al. Risk factors for venous thromboembolism of total hip arthroplasty and total knee arthroplasty: a systematic review of evidences in ten years. BMC Musculoskelet Disord. 2015;16:24. https://doi.org/10.1186/s12891-015-0470-0.
Courcoulas A, Coley RY, Clark JM, et al. Interventions and operations 5 years after bariatric surgery in a cohort from the US National Patient-Centered Clinical Research Network Bariatric Study. JAMA Surg. 2020;155(3):194–204. https://doi.org/10.1001/jamasurg.2019.5470.
Funding
The study was funded by NIH/NIDDK R01DK105960-01. Dr. Harrington was funded by a grant from the NHLBI (K01HL139997). Sponsors did not play a role in the collection, management, analysis or interpretation of data, the preparation, review, or approval of the manuscript, or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
For this type of study formal consent is not required.
Consent to Participate
Informed consent does not apply.
Conflict of Interest
Anita P. Courcoulas had a research grant from Allurion Inc. David E. Arterburn has grants from NIH and PCORI; a contract from Sharecare, Inc.; and received reimbursements for travel expenses from the American Society of Metabolic and Bariatric Surgery. Karen J. Coleman has funding for research from NIDDK, NHLBI, NIMH, and FDA and is paid a stipend for reviewing grants for NIH (outside of the submitted work). No authors have spouses, partners, or children that have financial relationships that may be relevant to the submitted work. Laura B. Harrington, Luke Benz, Sebastien Haneuse, Eric Johnson, Robert A. Li, Mary Kay Theis, Julie Cooper, Philip L. Chin, Gary G. Grinberg, Christopher R. Daigle, Julietta H. Chang, Scott S. Um, Panduranga R. Yenumula, and Jorge Zelada Getty have nothing to declare.
Data Access, Responsibility, and Analysis
Luke Benz, Sebastien Haneuse, and David Arterburn had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Data Sharing
Study participants did not give written consent for their data to be shared publicly, and the data contain protected health information governed by the US Health Insurance Portability and Accountability Act (HIPAA). Because of this, we do not plan to publicly share data; however, authors will respond to reasonable requests, with permission of all health systems involved and a fully executed data use agreement. In the interest of reproducibility, code used for all analyses is available on GitHub at https://github.com/lbenz730/arterburn_vte/.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Long-term VTE risk post-bariatric surgery is incompletely characterized.
• Our large population-based matched cohort included adults with severe obesity.
• Bariatric surgery was associated with a significantly lower risk of VTE long-term.
• This supports balanced consideration of short-term risks and long-term benefits.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Harrington, L.B., Benz, L., Haneuse, S. et al. Bariatric Surgery and the Long-Term Risk of Venous Thromboembolism: A Population-Based Cohort Study. OBES SURG 34, 2017–2025 (2024). https://doi.org/10.1007/s11695-024-07236-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-024-07236-y