Abstract
Background
Obesity is a well-known risk factor for gastroesophageal reflux disease (GERD). Even though symptoms may be mitigated or resolved with the weight loss caused by sleeve gastrectomy (SG), it may be associated with higher incidences of postoperative GERD. Ligamentum teres cardiopexy (LTC) is an alternative to Roux-en-Y gastric bypass, the gold standard treatment for GERD.
Methods
This study was a retrospective single-center chart review, all patients in this cohort underwent LTC to treat refractory GERD at our institution. The option for LTC was presented after patients’ refusal to undergo RYGB conversion. We collected baseline characteristics, standard demographics, pre-operative tests and imaging, and SG information, as well as intraoperative and perioperative data regarding LTC, and postoperative complications.
Results
Our cohort included 29 patients; most were Caucasian (44.8%) females (86.2%). The mean weight and BMI before LTC were 216.5 ± 39.3 lb and 36.1 ± 5.4 kg/m2, respectively. Mean total body-weight loss (TBWL) at 12 and 24 months were 28.7% ± 9.5% and 28.4% ± 12.4%, respectively. The mean interval between the index bariatric surgery and LTC was 59.9 ± 34.9 months, mean operative time was 67 ± 18.2 min, and median length of stay (LOS) was 1 day (IQR = 1–2 days). Twelve patients (57.1%) were able to discontinue antisecretory medications, while 9 (42.9%) still required them to remain asymptomatic. Mortality and reoperation rates were 0% and the incidence of complication was 19.4% (n = 6).
Conclusions
LTC is a safe and effective surgical alternative to treat refractory GERD symptoms after SG.
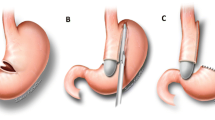
Graphical Abstract



Similar content being viewed by others
References
Fass R. Gastroesophageal reflux disease. N Engl J Med. 2022;387(13):1207–16. https://doi.org/10.1056/NEJMcp2114026.
Mahawar KK, Jennings N, Balupuri S, et al. Sleeve gastrectomy and gastro-oesophageal reflux disease: a complex relationship. Obes Surg. 2013;23(7):987–91. https://doi.org/10.1007/s11695-013-0899-x.
Melissas J, Braghetto I, Molina JC, et al. Gastroesophageal reflux disease and sleeve gastrectomy. Obes Surg. 2015;25(12):2430–5. https://doi.org/10.1007/s11695-015-1906-1.
DuPree CE, Blair K, Steele SR, et al. Laparoscopic sleeve gastrectomy in patients with preexisting gastroesophageal reflux disease: a national analysis. JAMA Surg. 2014;149(4):328–34. https://doi.org/10.1001/jamasurg.2013.4323.
Lazoura O, Zacharoulis D, Triantafyllidis G, et al. Symptoms of gastroesophageal reflux following laparoscopic sleeve gastrectomy are related to the final shape of the sleeve as depicted by radiology. Obes Surg. 2011;21(3):295–9. https://doi.org/10.1007/s11695-010-0339-0.
Popescu AL, Ioniţa-Radu F, Jinga M, et al. Laparoscopic sleeve gastrectomy and gastroesophageal reflux. Rom J Intern Med. 2018;56(4):227–32. https://doi.org/10.2478/rjim-2018-0019.
Rampal M, Perillat P, Rougaud R. Notes preliminaires sur une nouvelle tech- nique de cure chirurgicale des hernies hiatales: la cardiopexie par le ligament rond. Marseille Chir. 1964;16:488.
Bou Daher H, Sharara AI. Gastroesophageal reflux disease, obesity and laparoscopic sleeve gastrectomy: the burning questions. World J Gastroenterol. 2019;25(33):4805–13. https://doi.org/10.3748/wjg.v25.i33.4805.
Hawasli A, Foster R, Lew D, et al. Laparoscopic ligamentum teres cardiopexy to the rescue; an old procedure with a new use in managing reflux after sleeve gastrectomy. Am J Surg. 2021;221(3):602–5. https://doi.org/10.1016/j.amjsurg.2020.12.036.
Lind R, Hage K, Ghanem M, et al. Long-term outcomes of sleeve gastrectomy: weight recurrence and surgical non-responders. Obes Surg. 2023;33(10):3028–34. https://doi.org/10.1007/s11695-023-06730-z.
Hayes K, Eid G. Laparoscopic sleeve gastrectomy: surgical technique and perioperative care. Surg Clin North Am. 2016;96(4):763–71. https://doi.org/10.1016/j.suc.2016.03.015.
Maroun J, Li M, Oyefule O, et al. Ten year comparative analysis of sleeve gastrectomy, Roux-en-Y gastric bypass, and biliopancreatic diversion with duodenal switch in patients with BMI ≥ 50 kg/m2. Surg Endosc. 2022;36(7):4946–55. https://doi.org/10.1007/s00464-021-08850-y.
Sharara AI, Rustom LBO, Bou Daher H, et al. Prevalence of gastroesophageal reflux and risk factors for erosive esophagitis in obese patients considered for bariatric surgery. Dig Liver Dis. 2019;51(10):1375–9. https://doi.org/10.1016/j.dld.2019.04.010.
Kermansaravi M, Parmar C, Chiappetta S, et al. Best practice approach for redo-surgeries after sleeve gastrectomy, an expert’s modified Delphi consensus, 37. Surg Endosc. 2023 Mar;(3):1617–28. https://doi.org/10.1007/s00464-023-09879-x.
Parmar CD, Mahawar KK, Boyle M, et al. Conversion of sleeve gastrectomy to roux-en-Y gastric bypass is effective for gastro-oesophageal reflux disease but not for further weight loss. Obes Surg. 2017;27:1651–8.
Qumseya BJ, Qumsiyeh Y, Ponniah SA, et al. Barrett’s esophagus after sleeve gastrectomy: a systematic review and meta-analysis. Gastrointest Endosc. 2021;93(2):343–352.e2.
Gálvez-Valdovinos R, Cruz-Vigo JL, Marín-Santillán E, et al. Cardiopexy with ligamentum teres in patients with hiatal hernia and previous sleeve gastrectomy: an alternative treatment for gastroesophageal reflux disease. Obes Surg. 2015;25(8):1539–43. https://doi.org/10.1007/s11695-015-1740-5.
Mackey EE, Dore FJ, Kelly JF, et al. Ligamentum teres cardiopexy for post vertical sleeve gastrectomy gastroesophageal reflux. Surg Endosc. 2023;37(9):7247–53. https://doi.org/10.1007/s00464-023-10239-y.
Martínez Caballero J, de la Cruz VF, Gómez Rodríguez P, et al. Ligamentum teres cardiopexy might not prevent gastro-esophageal reflux after laparoscopic sleeve gastrectomy: case series. Obes Surg. 2023;33(3):965–8. https://doi.org/10.1007/s11695-022-06413-1.
Chiu S, Birch DW, Shi X, et al. Effect of sleeve gastrectomy on gastroesophageal reflux disease: a systematic review. Surg Obes Relat Dis. 2011;7(4):510–5. https://doi.org/10.1016/j.soard.2010.09.011.
Runkel A, Scheffel O, Marjanovic G, et al. The new interest of bariatric surgeons in the old ligamentum teres hepatis. Obes Surg. 2020;30(11):4592–8. https://doi.org/10.1007/s11695-020-04918-1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
For this type of study formal consent is not required. Informed consent does not apply. The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
•GERD is a burden to a parcel of patients who underwent SG.
•A total of 72.4% of patients stated that their symptoms completely subsided.
•LTC is a safe and effective surgical alternative to treat refractory GERD.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lind, R.P., Antunes, J., Ghanem, M. et al. Reflux After Sleeve Gastrectomy: Safety and Effectiveness of Laparoscopic Ligamentum Teres Cardiopexy, a Single-Center Experience. OBES SURG 34, 1232–1237 (2024). https://doi.org/10.1007/s11695-024-07103-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-024-07103-w