Abstract
Background
Changes in the skin structure, including the collagen and elastin content, have been reported with massive weight loss (MWL) following bariatric metabolic surgery (BMS) and have been correlated to a higher risk of complications after body-contouring surgery (BCS). This study aimed at comparing the histological characteristics of the skin of patients having surgical MWL (SMWL) post-BMS to those with non-surgical massive weight loss (NSMWL).
Methods
This prospective study compared the epidermal thickness, and collagen and elastin fibers content in 80 skin biopsies obtained from BCS procedures performed to patients who experienced MWL defined more than 50% of excess weight loss (%EWL) either SMWL (40 biopsies) or NSMWL (40 biopsies). Twenty biopsies in each group were obtained from abdominoplasties and 20 from breast reductions. Epidermal thickness was measured in H&E-stained sections, collagen fibers were assessed using Masson trichrome-stained sections, and elastin fibers were assessed using Modified Verhoeff’s stained sections. Image analysis software was used to calculate the fractions of collagen and elastin fibers.
Results
This study included 77 patients, 38 SMWL patients, and 39 NSMWL patients. The SMWL group had a significantly higher age (p < 0.001), a longer time interval from intervention (p < 0.001), higher initial weight (p < 0.001), higher initial BMI (p < 0.001), lower current weight (p = 0.005), lower current BMI (p < 0.001), and significantly higher %EWL than NSMWL group (p < 0.001). No significant differences were detected between the two groups regarding complications after abdominoplasty (p = 1.000). The elastic fibers content in the dermis was significantly higher in the abdominal region of the NSMWL group than SMWL (p = 0.029). All other parameters showed non-significant differences between NSMWL and SMWL in the skin of abdomen and breast.
Conclusion
The SMWL group had a significant reduction in elastic fiber content in the skin of the abdomen compared to the NSMWL group. The collagen content was equally reduced in both groups with non-significant differences in both breast and abdomen regions in both groups.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric metabolic surgery (BMS) is currently the most effective treatment for severe obesity, offering significantly greater massive weight loss (MWL) compared to non-surgical interventions, characterized by its rapidity, progression, and sustainability [1]. However, this rapid and substantial weight reduction frequently leads to the possible development of excessive loose skin. This condition poses both psychological and physical challenges for patients, often necessitating subsequent body-contouring surgery (BCS) [2,3,4]. High incidences of BCS have been observed in patients following BMS, with reported rates varying from 6 to 21%. Among these procedures, abdominoplasty is the most performed, followed by mastopexy [4,5,6,7]. Furthermore, patients who undergo BCS following BMS are reported to have a higher risk of developing complications compared to other patients [8,9,10]. BMS leads to significant changes in skin structure, notably impacting the collagen and elastin fibers within the dermis layer. These fibers are essential for maintaining skin integrity, strength, and elasticity. Rapid and substantial MWL post-BMS often results in changes in these critical skin components. These changes compromise the skin’s ability to retract and conform to the body’s new contours, thereby elevating the risk of suboptimal early and late outcomes in BCS [3, 7]. Nevertheless, few studies have specifically addressed the changes in skin structure associated with significant MWL. To the best of our knowledge, no research to date has directly compared the collagen and elastin content in the skin dermis of patients who have undergone surgical MWL (SMWL), following BMS with those who have undergone non-surgical MWL (NSMWL) following non-surgical interventions such as diet and exercise. Consequently, this study was designed to prospectively compare the collagen and elastin content in addition to the epidermal thickness of the skin of patients who have experienced SMWL with those who have NSMWL.
Methods
This prospective cohort study enrolled patients undergoing BCS following SMWL or NSMWL between March 2021 and October 2023 in Madina Women’s Hospital and Main University Hospital, Alexandria, Egypt. The study was conducted in accordance with the principles of the Declaration of Helsinki and approved by the ethical committee board. All patients signed informed consent. The study was approved by the ethical committee under registration number 0305862. Forty skin samples, 20 from breast skin and 20 from abdominal skin, were prospectively collected from the SMWL patients upon abdominoplasty and breast reduction procedures, and similarly 40 samples from NSMWL patients.
Study Endpoints
The primary endpoint of this study is to compare the epidermal thickness, collagen, and elastin content in the skin of individuals who have undergone SMWL to those NSMWL.
Inclusion Criteria
Patients, aged between 18 and 60 years, and an initial body mass index (BMI) of ≥ 35 kg/m2 before weight loss intervention who achieved MWL defined as a percentage of excess weight loss (%EWL) of ≥ 50% [11].
Exclusion Criteria
Factors associated with skin aging such as history of smoking, diabetes mellitus, metabolic syndrome, prolonged exposure to sunlight or ultraviolet rays, rheumatological diseases, and prolonged use of steroids [11,12,13].
Data Collection
Demographic data such as age, gender, time interval from the weight loss intervention to BCS, and associated medical problems before and after MWL. Weight loss data which included method of weight loss either SMWL or NSMWL, initial weight and BMI, weight, and BMI before BCS, and %EWL were collected. Complications of BCS were recorded with the Clavien-Dindo classification [14]. Furthermore, histological examination of the skin biopsies included epidermal thickness, and percentage of collagen and elastic fibers in biopsies.
Skin Examination
Skin biopsies were obtained from the removed skin during abdominoplasty and breast reduction procedures involving the epidermis, dermis, and subcutaneous tissue. Skin biopsies from both groups were fixed in 10% buffered formalin for 24 h. The following day, sections were taken and placed in plastic cassettes. The biopsy was well oriented in the cassette to show the epidermis overlying the dermis and subcutaneous tissue. Cassettes were processed in different grades of alcohol followed by xylene until embedded in paraffin. Three serial five-micron-thick sections were cut and mounted on glass slides. The first was stained by H&E staining using standard protocols. The second slide was stained by Masson’s trichrome stain (Trichrome Staining Kit (Modified Masson’s), ScyTeh, USA). Meanwhile, the last slide was stained by elastic stain (Elastic Stain Kit (modified Verhoeff’s), USA).
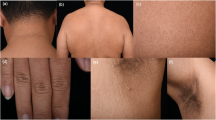
H&E-stained sections were examined by light microscope to exclude the presence of any pathology; then, multiple photos of the epidermis were taken using a camera coupled to a microscope. Photos were taken at × 200 power, and using the image analysis software, Image J (http://imagej.net), epidermal thickness was measured from the surface of the stratum corneum to the basement membrane. At least four measurements were taken on each photo; then, the mean was calculated. On Masson’s trichrome-stained sections, collagen fibers were stained blue. Multiple photos at × 200 power were taken from the dermis. Meanwhile, in modified Verhoeff’s stained sections, collagen bundles were seen deep pink in color while elastic tissue was seen black. Areas rich in elastic tissue were photographed at × 200 power. The elastic lamina of dermal vessels was stained black and considered as an internal positive control [15]. Photos in both Masson’s trichrome and modified Verhoeff’s stained slides were taken from the dermis and were assessed using Image J software. Photos were changed into gray scale 8-bit images; then, the threshold was adjusted to highlight the desired shade. The area of collagen or elastic tissue was calculated as a percentage/fraction of the total examined areas [16]. All biopsies were assessed blindly without prior knowledge of the patient’s history or clinical data. Areas of technical artifacts or large pilosebaceous structures were avoided (Figs. 1, 2, 3).
Assessment of different histopathologic skin parameters in this study at × 200 power (scale bar = 100 microns): A H&E-stained section to measure the epidermal thickness (black line). B Masson trichrome-stained section to assess collagen bundles which stained blue. The photo is changed into gray scale image (upper photo); then, segmentation of color was done to assess percentage of collagen fibers (lower photo) C Modified Verhoeff’s stained section to assess the elastic fibers. Collagen bundles are stained deep pink while elastic fibers are seen black in color. The photo was changed into gray scale 8-bit image (upper photo); then, segmentation of color was done to measure the percentage of elastic fibers (lower photo)
Histopathologic specimens of abdominal skin biopsies in studied cases: A NSMWL group and B SMWL group. H&E-stained sections (× 100, scale bar = 200 microns) shows no difference in epidermal thickness in both groups. Masson trichrome staining (× 200, inset: × 100) shows blue stained collagen bundles in the dermis. Modified Verhoeff’s stain (× 200, inset: × 100) shows deep pink collagen bundles and black-colored elastic tissues. NSMWL group shows increased elasticity in comparison to the SMWL group
Histopathologic assessment of breast skin biopsies in studied cases: A NSMWL group and B SMWL group. H&E-stained sections (× 100, scale bar = 200 microns) shows no difference in epidermal thickness in both groups. Masson trichrome staining (× 200, inset: × 100) shows blue-stained collagen bundles in the dermis. Modified Verhoeff’s stain (× 200, inset: × 100) shows deep pink collagen bundles and black-colored elastic tissues. No statistically difference in collagen and elastic tissues were detected between both groups
Statistical Analysis
Descriptive and inferential statistics were used for the analyses. All data were tested for normality using the Kolmogorov–Smirnov, Q-Q plot, and Levene’s tests. Categorical variables are expressed as numbers and percentages. Normally and non-normally distributed continuous variables are presented as means with standard deviations (SDs) and medians with interquartile ranges. When appropriate, categorical variables were tested using Pearson’s chi-square or Fisher’s exact test. Normally distributed continuous data were tested with independent samples with Student’s t-test or the Mann–Whitney U test was used for skewed (nonparametric) data. A significant level of 0.05 was used in all analyses. All analyses were conducted using R-software (version 4.2.2. Vienna, Austria).
Multiple linear regression analyses were conducted to estimate the effect of age, gender, type of weight loss intervention, type of body contour surgery, %EWL, time elapsed since intervention, post-BCS complications on elastic fibers proportions, collagen fibers proportion, and epidermal thickness.
Sample Size
The sample size calculation was done using the “pwr” package version 1.3–0. A large effect size (Cohen’s D) of 0.9 was used for the difference in collagen%, elastic%, and epidermal thickness between the control and bariatric using t test and a power of 80% with a significance level of 0.05; this resulted in a minimum sample size of 20 patients in each subgroup.
Results
This study included a total of 77 patients, with 38 post-bariatric patients in the SMWL group, and 39 patients in the NSMWL group. Three patients (3.9%) had concomitant abdominoplasty and breast reduction and were excluded.
Demographic and Personal Characteristic Data
The SMWL group had a significantly higher age mean ± sd (41.4 ± 6.2 vs. 30.3 ± 4.3, p < 0.001), a longer time interval from intervention to the BCS (23.7 ± 5.6 vs. 18.7 ± 2.8 months, p < 0.001), higher initial weight (112.7 ± 5.7 vs. 98.6 ± 7.4, p < 0.001), higher initial BMI (40.3 ± 1.9 vs. 35.7 ± 1.3, p < 0.001), lower current weight (78.1 ± 5.9 vs. 82.2 ± 6.6, p = 0.005), and lower current BMI (27.9 ± 0.8 vs. 29.8 ± 0.9, p < 0.001). Moreover, the SMWL group had significantly higher %EWL compared to the NSMWL group (80.9% ± 5.6 vs. 55.5% ± 6.7, p < 0.001) (Table 1).
Weight Loss Interventions
The BMS in the SMWL group included 27 (71.1%) laparoscopic sleeve gastrectomy procedures, six one-anastomosis gastric bypass (15.8%), and five Roux-en-Y gastric bypass (31.2%) procedures. The non-surgical interventions included hypo-energetic diet with exercise in 25 patients (64.1%), hypo-energetic diet alone in eight (20.5%), and hypo-energetic diet with orlistat medications in six (15.4%).
BCS Procedures
There were no significant differences between the two groups (NSMWL vs SMWL) regarding complications after abdominoplasty (CDI 15 vs. 10%, CDIIIa 5 vs. 10%), nor breast reduction procedures (CDI 5 vs. 10%, CDIIIa 10 vs. 5%) (p = 1.000) (Table 2).
Histological Examination of Skin Biopsies
The thickness of the skin epidermis in micrometers and fractions of collagen and elastic fibers in skin biopsies from the NSMWL and SMWL groups were measured. Only elastic fiber content in the dermis was significantly higher in the abdominal region of the NSMWL group than SMWL (p = 0.029). All other parameters showed non-significant differences between NSMWL and SMWL in the skin of the abdomen and breast (Table 3).
Table 4 and Table 5 present the results of multiple linear regression analyses, exploring the impact of various factors on key skin structure-related outcomes, including elastic fibers proportion, collagen fibers proportion, and epidermal thickness. The examined factors include age, gender, type of weight loss intervention, type of BCS, %EWL, time elapsed since intervention, and post-BCS complications. Significant predictors of elastic fibers proportion were the type of weight loss intervention and time elapsed from intervention. SMWL was linked to a decrease in elastic fibers proportion compared to NSMWL (estimate = − 3.56, 95% CI − 6.41 to − 0.70, p = 0.016), whereas the time elapsed since intervention exhibited a significant positive association with elastic fibers proportion, indicating that as time passes post-intervention, elastic fibers proportion tends to increase (estimate = 0.17, 95% CI 0.03 to 0.30, p = 0.016) (Table 4). On the contrary, SMWL was associated with higher collagen fiber proportion compared to NSMWL (estimate = 5.94, 95% CI 2.78 to 11.49, p = 0.036) (Table 4). In addition, higher collagen fiber proportion was associated with higher seroma drainage after BCS compared to no complications post-BCS (estimate = 9.96, 95% CI 4.65 to 19.25, p = 0.036) (Table 4). Hematoma formation (30.32, 95% CI 13.72 to 46.93, p = 0.001) and drainage of seroma (30.50, 95% CI 4.52 to 56.47, p = 0.022) were significantly associated with increased epidermal thickness (Table 4 and 5).
Discussion
To our knowledge, this is the first study that compares the histologic characteristics of skin in prospectively collected biopsies from patients undergoing body-contouring surgery (BCS) following both surgical SMWL and NSMWL. Various definitions of MWL have been reported in the literature, including the criterion used in this study, which defines MWL as a %EWL of ≥ 50% [17]. Other commonly referenced definitions include an excess body mass index loss (%EBMIL) of ≥ 30%, achieving a postoperative BMI of < 30 in patients with a preoperative BMI > 35, and a reduction of 50–100 pounds in body weight [2, 18].
MWL is commonly associated with the depletion of subcutaneous fat and contraction of the adipocutaneous envelope. This process varies among individuals: some patients exhibit better skin tone with successful tissue contraction, while others experience failure in soft tissue retraction, leading to excessive, hanging loose skin. This condition negatively impacts patients’ physical activity and psychological self-acceptance and is also associated with a higher incidence of skin lymphedema and infection [19]. Factors presumed to influence the ability of the adipocutaneous envelope to contract include the rate and amount of weight loss, as well as age, smoking habits, sun exposure, and genetic predisposition [8, 19]. Despite dramatic weight loss after BMS, patients may remain dissatisfied with their body image due to excess skin. A high proportion of patients after BMS, up to 96%, report experiencing excess skin, leading them to seek BCS [3, 4, 8, 19].
Up to 88% of patients undergoing BMS express a desire to undergo BCS, particularly for abdominal excess skin, which is reported by 60% of these individuals [8]. This desire stems from the need to alleviate the discomfort caused by excess skin and its associated psychological, physical, and social consequences. However, most of these patients do not proceed with BCS, often due to obstacles such as health insurance issues or rejection by a plastic surgeon. Additionally, the inclination to undergo BCS tends to decrease over time following BMS [4, 8].
Patients with SMWL face a higher risk of developing complications after BCS compared to those with NSMWL. A significant increased risk, ranging from 60 to 87% in SMWL, was highlighted in a meta-analysis conducted in 2014 [9]. Additionally, a 2021 meta-analysis reported an elevated risk of 37% in SMWL patients who had a body mass index (BMI) of 30 kg/m2 or more before undergoing BCS [10]. Furthermore, a notably higher incidence of post-BCS complications has been observed in SMWL patients with associated medical conditions such as dyslipidemia, diabetes mellitus, hypertension, and metabolic syndrome at the time of undergoing plastic surgery [20].
Moreover, SMWL patients are believed to exhibit specific histological changes in their skin, characterized by more pronounced epidermal weakening and a reduced dermal density of collagen and elastic fibers, compared to patients with and without obesity. However, the underlying causes of these changes are not yet fully understood [8].
This study obtained skin biopsies from abdominoplasties and breast reduction procedures, totaling 80 samples. The abdominal and breast regions were specifically chosen for histological examination, as massive weight loss most significantly affects these areas. Literature reports identify the abdomen as the region most commonly exhibiting hanging excess skin following massive weight loss, followed by the breast and chest regions, arms, thighs, and buttocks [8].
In this study, the mean epidermal thickness of the abdomen was 60.3 μm in the NSMWL group and 56.7 μm in the SMWL group. For breast biopsies, the mean epidermal thickness was 56.1 μm in the NSMWL group and 53.1 μm in the SMWL group. A recent systematic review reported a mean pooled epidermal thickness of 66.8 μm (ranging from 31.3 to 102.4 μm) in the breast region of healthy females, 79.2 μm in the abdomen of healthy females, and 100.4 μm in the abdomen of healthy men (ranging from 47.4 to 111.1 μm in females and 222.6 μm in males), with a trend of lower epidermal thickness in aged skin [21]. The epidermal thickness observed in our study was slightly lower than the reported mean in the review. Notably, the SMWL group exhibited marginally lower mean values than the NSMWL group. Though these differences were not statistically significant, they might suggest a higher degree of skin aging in the SMWL group.
In terms of collagen fiber density in this study, the fractions of collagen in the dermis were 49.5% in the abdomen and 49.6% in the breast for the NSMWL group. In contrast, the SMWL group showed 49.2% in the abdomen and 49.3% in the breast, indicating no significant differences between the groups. However, a notable distinction was observed in the density of elastic fibers. In the abdominal skin biopsies, the SMWL group demonstrated a significantly lower fraction of elastic fibers compared to the NSMWL group (5% vs 6.8%, respectively, p = 0.029). In contrast, the breast skin biopsies showed fractions of elastic fibers of 6.3% in the SMWL group and 6.7% in the NSMWL group, with no significant differences noted between the two.
Orpheu et al. [3] conducted a comparison of the collagen and elastic fiber content in the abdominal skin of post-BMS patients with massive weight loss to that of patients that never had obesity. Their findings revealed significantly lower fractions of collagen fibers in biopsies from both the upper and lower abdomen of post-BMS patients compared to patients that never had obesity (46.4–47.6% vs 58.6–52.4%, respectively, p = 0.001–0.007). Conversely, they observed significantly higher fractions of elastic fibers in biopsies from the upper abdomen of post-BMS patients (9.5% vs 7.7%, respectively, p = 0.004). However, the difference in elastic fiber fractions in the lower abdomen biopsies between post-BMS and patients that never had obesity was not significant (7.2% vs 7.6%, respectively, p = 0.187).
The collagen fractions observed in both groups of this study closely align with the collagen fractions reported in post-bariatric patients by Orpheu et al. [3]. This similarity suggests a relative lack of collagen fibers in comparison to healthy patients who have not experienced massive weight loss. Such a trend is akin to the aging process of the skin, which is characterized by a depletion of collagen and a reduction in its tensile strength [11].
Another study by Rocha et al. compared the content of collagen and elastic fibers in abdominal skin samples from SMWL patients to those from patients with obesity. They utilized Picrosirius staining with polarized light for studying collagen and Weigert’s resorcin-fuchsin method for elastic fibers. Their findings showed nearly equal total fractions of collagen in both groups (77% in post-bariatric patient’s vs 75% in patients with obesity). However, they observed significant structural changes in the dermis, notably a reduction in thick, well-structured collagen fibers and an increase in loosely arranged, thin collagen fibers in SMWL patients. Additionally, there was an increase in elastic fibers in SMWL patients compared to patients with obesity (1.3% vs 0.8%, respectively) [7].
Our study observed a lower likelihood of seroma occurrence in the surgical group, as indicated by the surgical estimated OR of − 0.13 and the negative association with seroma at − 4.53. However, when seroma was present, it correlated with higher requirements for drainage (30.50) and an increased incidence of hematoma (30.32). These results highlight the complex interplay between surgical outcomes and post-BCS complications. While no significant direct correlation was found between skin epidermal thickness and these complications, the nuanced roles of physiological and anatomical factors, including skin properties, warrant further investigation. This underscores the necessity of a multifaceted approach to understanding and managing postoperative complications in BCS, considering the intricate connections between surgical techniques, patient characteristics, and skin healing and physiology.
The literature provides limited data on skin structural changes associated with MWL. Nevertheless, both the available literature and our findings indicate that MWL generally leads to a depletion of collagen content or a reduction in the structured collagen fibers compared to normal skin. The behavior of elastic fiber content, however, appears to vary; it may either decrease or increase, and these changes can differ across various body regions. Additionally, the diverse methodologies employed for identifying the fractions of collagen and elastic fibers in different studies might contribute to the variability and lack of uniformity in the data.
Limitations
This study represents the first to compare and analyze skin structural changes following MWL, contrasting outcomes from bariatric surgery with those resulting from non-surgical weight loss methods. Key areas of focus included epidermal thickness, dermal collagen content, and dermal elastic fiber content. These insights may aid in predicting and understanding the skin changes associated with massive weight loss. However, the study is not without limitations. These include the absence of longitudinal follow-up to observe changes in the skin over time, a relatively small sample size—a challenge due to the difficulty in assembling a large cohort of individuals with non-surgical massive weight loss—and the lack of a control group comprising normal skin from patients without obesity. Additionally, a notable limitation is the unknown type of dietary regimen followed by the participants in the NSMWL group, which could influence the skin’s response to weight loss and thus affect the study’s outcomes.
Conclusion
The SMWL group demonstrated a significant reduction in the content of elastic fibers in the skin of the abdomen compared to the NSMWL group. However, in the breast skin, the differences in elastic fiber content between the two groups were not significant. While the collagen content did not show significant differences in either the breast or abdomen regions between the two groups, it is noteworthy that the collagen content in both groups was reduced compared to the normal skin data available in the literature.
Data Availability
Data is available with the corresponding author.
References
Arterburn DE, Johnson E, Coleman KJ, et al. Weight outcomes of sleeve gastrectomy and gastric bypass compared to nonsurgical treatment. Ann Surg. 2021;274:e1269–76.
ElAbd R, AlMojel M, AlSabah S, et al. Complications post abdominoplasty after surgical versus non-surgical massive weight loss: a comparative study. Obes Surg. 2022;32:3847–53.
Orpheu SC, Coltro PS, Scopel G, et al. Collagen and elastic content of abdominal skin after surgical weight loss. Obes Surg. 2010;20:480–6.
De Vries C, Kalff M, van Praag E, et al. The influence of body contouring surgery on weight control and comorbidities in patients after bariatric surgery. Obes Surg. 2020;30:924–30.
Altieri MS, Yang J, Park J, et al. Utilization of body contouring procedures following weight loss surgery: a study of 37,806 patients. Obes Surg. 2017;27:2981–7.
Kitzinger HB, Abayev S, Pittermann A, et al. The prevalence of body contouring surgery after gastric bypass surgery. Obes Surg. 2012;22:8–12.
Rocha RI, Junior WC, Modolin ML, et al. Skin changes due to massive weight loss: histological changes and the causes of the limited results of contouring surgeries. Obes Surg. 2021;31:1505–13.
Ellison JM, Steffen KJ, Sarwer DB. Body contouring after bariatric surgery. Eur Eat Disord Rev. 2015;23:479–87.
Hasanbegovic E, Sørensen JA. Complications following body contouring surgery after massive weight loss: a meta-analysis. J Plast Reconstr Aesthet Surg. 2014;67:295–301.
Marouf A, Mortada H. Complications of body contouring surgery in postbariatric patients: a systematic review and meta-analysis. Aesthetic Plast Surg. 2021;45:2810–20.
Farage MA, Miller KW, Elsner P, et al. Structural characteristics of the aging skin: a review. Cutan Ocul Toxicol. 2007;26:343–57.
Quondamatteo F. Skin and diabetes mellitus: what do we know? Cell Tissue Res. 2014;355:1–21.
Reilly DM, Lozano J. Skin collagen through the lifestages: importance for skin health and beauty. Plast Aesthetic Res. 2021;8:2. https://doi.org/10.20517/2347-9264.2020.153
Clavien PA, Barkun J, De Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–96.
Fachinelli A, Trindade M, Fachinelli F. Elastic fibers in the anterior abdominal wall. Hernia. 2011;15:409–15.
Kumar N, Kumar P, Nayak Badagabettu S, Prasad K, Kudva R, Raghuveer CV. Quantitative fraction evaluation of dermal collagen and elastic fibres in the skin samples obtained in two orientations from the trunk region. Dermatol Res Pract. 2014;2014:251254. https://doi.org/10.1155/2014/251254
Shermak MA, Chang D, Magnuson TH, et al. An outcomes analysis of patients undergoing body contouring surgery after massive weight loss. Plast Reconstr Surg. 2006;118:1026–31.
De Kerviler S, Hüsler R, Banic A, et al. Body contouring surgery following bariatric surgery and dietetically induced massive weight reduction: a risk analysis. Obes Surg. 2009;19:553–9.
Abela C, Stevens T, Reddy M, et al. A multidisciplinary approach to post-bariatric plastic surgery. Int J Surg. 2011;9:29–35.
Rosa SC, de Macedo JLS, Canedo LR, et al. What is the impact of comorbidities on the risk for postoperative body-contouring surgery complications in postbariatric patients? Obes Surg. 2019;29:552–9.
Lintzeri D, Karimian N, Blume-Peytavi U et al. Epidermal thickness in healthy humans: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2022;36:1191–200.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and the guidelines of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hany, M., Zidan, A., Ghozlan, N.A. et al. Comparison of Histological Skin Changes After Massive Weight Loss in Post-bariatric and Non-bariatric Patients. OBES SURG 34, 855–865 (2024). https://doi.org/10.1007/s11695-024-07066-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-024-07066-y