Abstract
Background
Malnutrition and liver impairment after duodenal switch (DS) are possible and undesired complications, often conservatively treated. However, in specific cases, surgical revision may be necessary. This study aims to describe outcomes achieved by two bariatric surgery centers and address effectiveness and safety of revisional surgical procedures to resolve these complications.
Methods
A retrospective chart review was performed in two bariatric surgery centers from 2008 to 2022. Patients who required revisional surgery to treat malnutrition and/or liver impairment refractory to nutritional and total parenteral nutrition intervention (TPN) after duodenal switch were included. No comparisons were performed due to the descriptive nature of this study.
Results
Thirteen patients underwent revisional surgery, the mean age was 44.7, the 53.8% were females, and the mean preoperative BMI was 54.7 kg/m2; the mean time between DS and revisional procedure was 26.5 months, and 69.1% of patients were placed on TPN. One patient developed hepatic encephalopathy; one patient presented with ascites, pleural effusion, and renal insufficiency, undergoing reoperation after revisional procedure due to a perforated ileal loop. Mortality rate was 0%; all patients regained weight after the revisional procedure, and the mean total protein and albumin blood levels 12 months after surgery were 6.3 and 3.6 g/dl, respectively.
Conclusions
While refractory malnutrition and/or liver failure are rare among patients post-DS, if underdiagnosed and untreated, this can lead to irreversible outcomes and death. All revisional procedures included in this study resulted in improvement of the nutritional status and reversal of liver impairment, with low complication rates.
Graphical Abstract






Similar content being viewed by others
Data Availability
The data that support the findings of this study are on a repository; they are not publicly available because it contains information that could compromise the privacy of research participants.
References
Gloy VL, Briel M, Bhatt DL, et al. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJ. 2013;347:f5934.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Maroun J, Li M, Oyefule O, et al. Ten year comparative analysis of sleeve gastrectomy, Roux-en-Y gastric bypass, and biliopancreatic diversion with duodenal switch in patients with BMI ≥ 50 kg/m(2). Surg Endosc. 2022;36(7):4946–55.
Conner J, Nottingham JM. Biliopancreatic diversion with duodenal switch. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC.; 2022.
Onem S, Cengiz O, Dolu S, et al. Acute liver failure after bariatric surgery. Hepatol Forum. 2020;1(3):119–20.
Sagredo S, Brahm J, Uribe M, et al. Acute liver failure after bariatric surgery. A case report and literature review. Gastroenterol Hepatol. 2013;36(2):76–80.
Baltasar A, Bou R, Bengochea M. Fatal perforations in laparoscopic bowel lengthening operations for malnutrition. Surg Obes Relat Dis. 2010;6(5):572–4.
Vahibe A, Aizpuru MJ, Sarr MG, et al. Safety and efficacy of revisional surgery as a treatment for malnutrition after bariatric surgery. J Am Coll Surg. 2023;236(1):156–66.
Brethauer SA, Kothari S, Sudan R, et al. Systematic review on reoperative bariatric surgery: American Society for Metabolic and Bariatric Surgery Revision Task Force. Surg Obes Relat Dis. 2014;10(5):952–72.
Topart PA, Becouarn G. Revision and reversal after biliopancreatic diversion for excessive side effects or ineffective weight loss: a review of the current literature on indications and procedures. Surg Obes Relat Dis. 2015;11(4):965–72.
Süsstrunk J, Schneider R, Peterli R, et al. Long-term outcome after biliopancreatic diversion with duodenal switch: a single-center experience with up to 20 years follow-up. Surg Obes Relat Dis. 2023;19(2):83–90.
Hess DS, Hess DW, Oakley RS. The biliopancreatic diversion with the duodenal switch: results beyond 10 years. Obes Surg. 2005;15(3):408–16.
Hamoui N, Chock B, Anthone GJ, et al. Revision of the duodenal switch: indications, technique, and outcomes. J Am Coll Surg. 2007;204(4):603–8.
Mantziari S, Abboretti F, Favre L, et al. Protein malnutrition after Roux-en-Y gastric bypass: a challenging case and scoping review of the literature. Surg Obes Relat Dis. 2022;28:S1550–7289(22)00828–0. https://doi.org/10.1016/j.soard.2022.12.032
Nakanishi H, Matar RH, Vahibe A, et al. Single versus double anastomosis duodenal switch in the management of obesity: a meta-analysis and systematic review. Surg Laparosc Endosc Percutan Tech. 2022;32(5):595–605.
Lind RP, Ghanem M, Teixeira AF, et al. Single- versus double-anastomosis duodenal switch: outcomes stratified by preoperative BMI. Obes Surg. 2022;32(12):3869–78.
Handzlik-Orlik G, Holecki M, Orlik B, et al. Nutrition management of the post-bariatric surgery patient. Nutr Clin Pract. 2015;30(3):383–92.
Baltasar A, Serra C, Pérez N, et al. Clinical hepatic impairment after the duodenal switch. Obes Surg. 2004;14(1):77–83.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Consent to Participate
An informed consent waiver was obtained for this study.
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Malnutrition and liver impairment after DS rarely require surgical intervention.
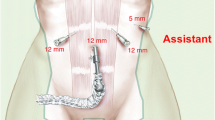
• Lengthening of the common channel, conversion to RYGB, and “kissing X” procedure were performed.
• All procedures were effective at reversing complications, with 0% mortality.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lind, R.P., Salame, M., Kendrick, M. et al. Management of Malnutrition and Hepatic Impairment After Duodenal Switch. OBES SURG 34, 602–609 (2024). https://doi.org/10.1007/s11695-023-07032-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-07032-0