Abstract
Background
The SF-6D index can be used to calculate quality-adjusted life years in economic evaluations, which is required by reimbursement agencies and national advisory bodies, including the Swedish ones. However, despite that SF-36 has been largely applied among patients undergoing bariatric surgery, almost no study has accessed the short form six-dimensions (SF-6D) after bariatric surgery.
Aim
To establish normative values for the SF-6D index among patients undergoing bariatric surgery.
Materials and Methods
All patients who received bariatric surgery in Sweden between 2011–01-01 and 2019–03-31 were obtained from the Scandinavian Obesity Surgery Registry (SOReg). Information includes patients’ sociodemographic characteristics, details regarding the procedure, and postsurgical conditions. The SF-36 is applied at baseline and at follow-up years 1, 2, and 5. The multiple sequential imputation method was applied to handle missingness on SF-6D items. Based on the UK tariff, the SF-6D preference scores were calculated. The normative values for the mean (SD) SF-6D index were reported by timepoint and surgical complications for men and women, respectively. Multivariate analyses were applied to investigate how the SF-6D index is associated with timepoint, controlling for age, sex, BMI, and comorbidities in a stepwise manner.
Results
The SF-6D index increased at 1 year relative to baseline and was roughly maintained at the same level at 2 years. The normative value of the SF-6D index can be used in economic evaluations for bariatric surgery.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The prevalence of obesity has increased over time, especially in North America and Europe, with 30% of women and 24% of men affected by obesity in the USA [1]. Obesity is associated with significant mortality and reduced health-related quality of life (HRQoL). People with obesity run an increased risk of developing and worsening diabetes mellitus, cardiovascular disease, and cancer. Obesity also imposes a large economic burden on the individual and on families and the society [2] with an estimated impact of 2.8% of the global gross domestic product (GDP) [2]. Management of obesity involves lifestyle modification [3, 4], pharmacotherapy [3, 5], and bariatric surgery [3, 5]. Bariatric surgery is the most effective treatment for weight reduction, and it has also been shown to improve obesity-related complications including diabetes mellitus [6], cardiovascular disease [7], and life expectancy [8].
The most important endpoint for individuals undergoing treatment is the improvement in Health-related quality of life (HRQoL). HRQoL is an important measure as it provides a comprehensive understanding of the patient’s health status and the impact of healthcare interventions on their quality of life. It is used to monitor the effectiveness of healthcare interventions and to evaluate the cost-effectiveness of healthcare programs [9]. Quality-adjusted life years (QALYs) is a measure of disease burden that combines the quality and quantity of life, which is calculated by multiplying the duration of time spent in a health state by the HRQoL weight (i.e., utility score) associated with a certain health state [10]. The Short Form-36 (SF-36) is the most commonly used HRQoL instrument [11,12,13]; however, HRQoL weight cannot be derived directly from SF-36 scores. The Short Form 6 Dimension (SF-6D) algorithm enables the calculation of HRQoL weights based on SF-36 data, which allows the calculation of QALYS and cost-effectiveness analysis of health interventions [14]. It is used by health technology assessment agencies around the world, including in Australia, Canada, China, Ireland, Japan, Netherlands, Norway, Spain, and the USA [15].
Many studies have reported results from SF-36 in patients following bariatric surgery; however, only a few reported results from SF-6D [12]. One of the main challenges for the successful implementation of SF-6D could be related to missing data, caused by respondents not providing answers to certain items in SF-36, or being lost to follow-ups [10, 16]. Therefore, It is important to understand missingness patterns and handle missing data properly when analyzing HRQoL data, since missing data may lead to biased conclusions [17].
Normative data, data that characterize what is usual in a defined population at a specific point or period of time, are of enormous importance to primary care physicians [10, 18]. Several sets of normative values for SF-6D have been published for the general population [31,32,33,34]. Normative values for SF-6D among patients undergoing bariatric surgery can be utilized in economic evaluation and facilitate reimbursement decisions associated with treatments for patients with obesity.
The aim of this study was to establish normative values for the SF-6D index among patients undergoing bariatric surgery.
Method
Data
The Scandinavian Obesity Surgery Registry (SOReg) is a nationwide quality register of patients undergoing bariatric surgery in Sweden with a coverage exceeding 97%. It is validated regularly and is shown to have high data quality [19]. SOReg contains information on patients’ sociodemographic status, provider characteristics, details regarding procedures, and health-related outcomes, including HRQoL assessed by the SF-36 and the Obesity Problems scale (OP). HRQoL data are reported by patients at baseline and at 1, 2, and 5 years post-operatively by filling in a questionnaire. Nurses took anthropometric data and collected the completed questionnaires. Trained personnel will perform data input. For the current study, all subjects who received bariatric surgery from 2011–01-01 to 2019–03 were included (n = 36 706). The Ethics Authority in Sweden granted ethical permission for analyses of this study (reference number: 2019–03666).
Health Outcome Measure
Short Form-36 (SF-36/RAND) and SF-6D
The SF-36 is applied in the SOReg. It measures HRQoL in eight domains, including social functioning, physical function, role-physical, bodily pain, vitality, social functioning, role-emotional, and mental health [20, 21]. The short form six-dimensions (SF-6D) was developed to derive a preference-based score from the SF-36 [14] or its 12-item version (SF-12) [22]. Briefly, 11 items from the original SF-36 were selected to form the six SF-6D domains (Supplementary material S2), including pain, mental health, physical functioning, social functioning, role limitations, and vitality, and each is described into four to six functional levels (Supplementary material S1). Each domain level is associated with a specific health weight. For problems reported on any level of any health domain, the corresponding weight will be deducted from the full health which is equivalent to 1 [14]. The details regarding how to calculate SF-6D can be requested from the ScHARR Outcomes team at the University of Sheffield [23]. The weights for calculating the SF-6D index are derived from a general population sample using a standard gamble method. The current study used the UK tariff [14] since there was no local tariff available in Sweden. Details regarding the SF-6D domains and relevant SF-36 items are given in the supplemental material (S1 and S2). The SF-6D index ranged between 0 and 1, with a higher value indicating better health.
Imputation of SF-6D Index
The overall missing data proportions (including both missing responses to items and missing forms due to loss to follow-up) of SF-6D in the 1-, 3-, and 5-year follow-ups were 40.7%, 62.9%, and 83.8%, respectively. The comprehensive information regarding missingness and missing patterns of the variables has been previously published [24]. Taking into consideration the longitudinal nature of the data collected, we adopted a sequential multiple imputation (SMI) method to impute the SF-6D index as well as other variables with missing values [24]. Briefly, the missing values of the selected eleven SF-36 items at baseline were first multiply imputed by chained equations using the baseline variables, including age, sex, BMI, pregnancy, and comorbidities. Second, for the SF-6D index of a given follow-up timepoint, missing values were imputed using the information from the baseline and previous years, including the demographic variables, SF-6D items, and comorbidities. In the current study, five imputed datasets by SMI were used to conduct descriptive and inferential analyses for the SF-6D index. The SMI method adopted in the current study might achieve an ideal imputation for the missing data even when the follow-up survey had a missing rate of 60% under the missing at random assumption [24], which could avoid significant information waste in multivariate analysis using patients with complete data only.
Sociodemographic and Clinical Characteristics
Age was categorized into age groups of 35–44 years, 45–54 years, 55–64 years, and ≥ 65 years. Educational level was self-reported and grouped into primary school with up to 9 years of education, secondary school with 9–12 years of education, and university with over 12 years. Smoking was self-reported and categorized as yes, no, occasionally, previous smoker quit before operation, and unknown. BMI was categorized into three groups including < 40, 40–44, 45–49, and 50 kg/m2 and above. Comorbidities were self-reported by the patients at baseline, including the occurrence of sleep apnea, hypertension, diabetes mellitus, dyspepsia, diarrhea, depression, and other illnesses.
Statistical Analysis
Descriptive analyses were used to examine the sample characteristics and the responses to the SF-6D domains (proportions for discrete variables, mean and standard deviation, plus median and inter-quart range for continuous variables). We applied multivariate analysis to investigate how the SF-6D index is associated with timepoint, controlling for age, sex, BMI, and comorbidities in a stepwise manner. In addition to the commonly used ordinary least squares (OLS) method, the mixed-effects Tobit regression model was used since the SF-6D index was centered at 1) [25], with random effects for patients to account for individual response clustering. The final results were combined from the five imputed datasets according to Rubin’s rule [26]. All analyses were conducted using R.4.0.2 [27] or Stata 17.0 [28].
Results
More than 76% of the patients in the study were females, and the mean age was 41 years old at baseline. Approximately 10% of the patients were current smokers (Table 1). The mean BMI was 42 kg/m2 at baseline and decreased to 29 kg/m2 at follow-ups. In general, the presence of obesity-related comorbidities including sleep apnoea, hypertension, diabetes, dyslipidemia, and depression decreased over time and was lowest at the 1-year follow-up. HRQoL improved after surgery, with the highest improvements observed at the 1-year follow-up, followed by the 2- and 5-year follow-ups (Table 2). The SF-6D index was close to a normal distribution at baseline but left-skewed at follow-ups (Supplementary material Figure S1).
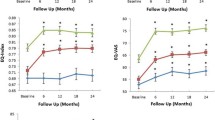
The proportion of patients without any problems on any SF-6D dimension is reported in Fig. 1. Improvements at the 1-year follow-up were reported in all dimensions, the largest being physical function (44%), followed by role limitations (34%), social function (30%), pain (30%), mental health (22%), and vitality (12%). At the 2- and 5-year follow-ups, a slight decrease in HRQoL relative to year 1 can be observed in all dimensions. However, relative to the baseline, there were still improvements in all dimensions. The proportions of patients reporting problems at all levels on each SF-6D dimension are presented in Figure S2 in Supplementary material S4.
The normative values for the mean and median SF-6D index, based on imputed data, are reported in Table 2 and (Supplementary material S3), respectively. The results were reported by timepoint and surgical complications for men and women, respectively. The SF-6D index increased at 1 year relative to baseline and was roughly maintained at the same level at 2 years. No normative values are presented at 5-year follow-up due to many missing data. In general, patients with complications had a slightly lower SF-6D index, and women had a slightly higher index value; however, such differences were not significant. No clear age gradient was observed.
The results from the regression analyses are reported in Table 3. Significant increases in the SF-6D index were observed at the 1- and 2-year follow-ups, with the largest increase at the 1-year follow-up. This effect was approximately the same, even after controlling for age, sex, and baseline BMI (models 2 to 4), and reduced after controlling for comorbidities (model 5). Being female was positively associated with the SF-6D index, and sleep apnea, dyspepsia, diarrhea, and depression were significantly negatively associated with the SF-6D index. No clear age gradient was observed.
Discussion
To the best of our knowledge, this study has established the first normative values for SF-6D among patients undergoing bariatric surgery. The results of the study can be used in economic evaluations for bariatric surgery. The results also demonstrate significant improvements in HRQoL following bariatric surgery in all health dimensions. This finding supports previous studies reporting that HRQoL improves after bariatric surgery, especially for dimensions related to physical function [12, 13, 29].
Surprisingly, almost no study has assessed the SF-6D after bariatric surgery despite that SF-36 has been extensively applied among such patients [12, 29]. Economic evaluations of patients undergoing bariatric often applied health preferences derived from other PBM, such as EQ-5D, or mapping algorithms [30]. Our study has demonstrated that the SF-6D health preferences can be derived from the SF-36 with relative ease, and we hope this work might raise awareness that large HRQoL databases on bariatric surgery such as the one generated by SOReg, which reports SF-36 data, can be better utilized. The SF-6D has a particular strength in that it can be derived from the SF-36 specifically for use in economic evaluation, which can inform decisions on reimbursement of health technology in the treatment of people with obesity. This study has the potential to improve healthcare economic data from previous studies, by converting SF-36 into SF-6D in patients undergoing bariatric surgery. Comparing our results with the SF-6D norms for the general population [31,32,33,34], the patients undergoing bariatric surgery reported lower SF-6D index at baseline, but almost the same level as the general population at 1- and 2-year follow-ups. This suggests that bariatric surgery improves HRQoL for patients with obesity to almost the level of a normal population supporting the benefits not only in terms of cardiometabolic effects but also in terms of patients-reported outcome translating into direct values to the individual. A previous systematic review found no consistency in the literature concerning long-term HRQoL after bariatric surgery. Some research indicates that HRQoL improves for up to 1 year and then plateaus and/or declines [31, 32], while other research suggested that HRQoL continues to improve after surgery [33]. In our study, we found that the greatest improvement in HRQoL was at 1 year, which declined slightly at 2 years but still significantly improved relative to the baseline. Unfortunately, we cannot draw any conclusions about HRQoL at 5 years after surgery due to the many patients lost at follow-up after 5 years.
Strength and Limitations
The main strength of our study was the use of real-world data from a large national patient register, which enables us to report HRQoL changes over time before and after bariatric surgery, as well as the influence of surgery on different health domains. Normative data may be obtained in cross-sectional studies or longitudinal study. As we do not expect potential epoch effects associated with bariatric surgery and to maximize the sample size, we pulled data from different years together. We also applied multivariate analyses to examine whether the improvement remained after adjusting for age, sex, BMI, and comorbidities. To the best of our knowledge, this is the first study that reported SF-6D normative values among bariatric patients. Such data can be utilized in economic evaluation. Nevertheless, the SF-36 scores would be still useful, especially in the clinical settings. The SMI method adopted in the current study might be an ideal strategy for handling missing data (even though the follow-up survey had a missing proportion of 60%), avoiding significant information waste in the multivariate analysis.
There are a few limitations that need to be addressed: we based our calculation of SF-6D on the UK value set, as there was not a Swedish one. People in different countries may value health differently; however, as both are European countries, we do not expect that people will value health very differently. Some surgical centers had a low response rate HRQoL, but since most centers in Sweden have similar characteristics in patient cohorts, this is unlikely to have a significant impact on the representativeness of our study sample. Moreover, due to the high missingness at 5 years (80%), even the SMI could not handle this, so we are not able to draw a conclusion about HRQoL beyond 2 years from the baseline. Data quality for self-reported educational level is low, and therefore, socio-economic status could not be included in the analyses. To prevent and handle missing data in HRQoL studies, researchers should apply a rigorous methodology and practices. Guidance for preventing and handling missing data in observational studies is needed, and studies that use real-world data should be prioritized. For the analysis of socio-economic status, linkage with national registries is required. A previous study which is also based on SOReg (with linkage data for socio-economic status) investigated the association between weight loss and socio-economic status and has shown that the first generation immigrants and patients residing in larger towns (> 200,000 inhabitants) tend to have inferior weight loss compared to other groups; however, the remaining socioeconomic factors appear to have a weaker association with postoperative weight loss [34].
Conclusions
This study established normative values for SF-6D among patients undergoing bariatric surgery based on a large registry. The results of the study can be used in economic evaluations for bariatric surgery.
Data Availability
Data sharing is not possible according to Swedish law.
References
Branca F, Nikogosian H, Lobstein T, World Health Organization, editors. The challenge of obesity in the WHO European region and the strategies for response: summary. Copenhagen: World Health Organization, Regional Office for Europe; 2007.
Tremmel M, Gerdtham UG, Nilsson PM, Saha S. Economic burden of obesity: a systematic literature review. Int J Environ Res Public Health [Internet]. 2017 Apr [cited 2019 Sep 2];14(4). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5409636/
Jensen MD, Ryan DH, Donato KA, et al. Executive summary: guidelines (2013) for the management of overweight and obesity in adults. Obesity. 2014;22(S2):S5-39.
National Institute for Health and Care Excellence (NICE). Obesity: guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children [Internet]. [cited 2016 Jan 20]. Report No.: CG43. https://www.nice.org.uk/guidance/cg43
American Association of Clinical Endocrinologists The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient -- update: Surg Obes Relat Dis. 2013;9(2):159.
Sundbom M, Hedberg J, Marsk R, Boman L, Bylund A, Hedenbro J, et al. Substantial decrease in comorbidity 5 years after gastric bypass: a population-based study from the Scandinavian Obesity Surgery Registry. Ann Surg 2016;1.
Strazzullo P, D’Elia L, Cairella G, et al. Excess body weight and incidence of stroke: meta-analysis of prospective studies with 2 million participants. Stroke. 2010;41(5):e418–26.
Kahan S, Williams A. In adults with obesity, metabolic–bariatric surgery vs. usual care is associated with lower all-cause mortality. Ann Intern Med. 2021;174(9):JC101.
WHOQOL - Measuring quality of life| The World Health Organization [Internet]. [cited 2023 Dec 8]. https://www.who.int/tools/whoqol
Fayers PM, Machin D. Quality of life: the assessment, analysis and interpretation of patient-reported outcomes. 2nd ed. UK: John Wiley & Sons Ltd.; 2006.
Coulman KD, Abdelrahman T, Owen-Smith A, et al. Patient-reported outcomes in bariatric surgery: a systematic review of standards of reporting. Obes Rev. 2013;14(9):707–20.
Hachem A, Brennan L. Quality of life outcomes of bariatric surgery: a systematic review. Obes Surg. 2016;26(2):395–409.
Lindekilde N, Gladstone BP, Lübeck M, et al. The impact of bariatric surgery on quality of life: a systematic review and meta-analysis. Obes Rev. 2015;16(8):639–51.
Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. 2002;21(2):271–92.
The University of Sheffield. The SF-6D: an internationally adopted measure for valuing health and assessing the cost-effectiveness of health care interventions [Internet]. 2023 [cited 2023 Dec 8]. https://www.sheffield.ac.uk/economics/research/impact-and-knowledge-exchange/sf6d
Drummond MF, Sculpher M, Torrance GW, et al. Methods for the economic evaluation of health care programs. New York: Oxford University Press; 2005. p. 404.
Li T, Hutfless S, Scharfstein DO, et al. Standards should be applied in the prevention and handling of missing data for patient-centered outcomes research: a systematic review and expert consensus. J Clin Epidemiol. 2014;67(1):15–32.
O’Connor PJ. Normative data: their definition, interpretation, and importance for primary care physicians. Fam Med. 1990;22(4):307–11.
Sundbom M, Näslund I, Näslund E, et al. High acquisition rate and internal validity in the Scandinavian Obesity Surgery Registry. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2021;17(3):606–14.
Ware JE Jr, Gandek B. Overview of the SF-36 health survey and the international quality of life assessment (IQOLA) project. J Clin Epidemiol. 1998;51(11):903–12.
Monica 1776 Main Street Santa, California 90401–3208. 36-item short form survey from the RAND medical outcomes study [Internet]. [cited 2018 Mar 29]. https://www.rand.org/health/surveys_tools/mos/36-item-short-form.html
Brazier JE, Roberts J. The estimation of a preference-based measure of health from the SF-12. Med Care. 2004;42(9):851–9.
ScHARR Outcomes team the University of Sheffield. SF-6D & SF-6Dv2 - Calculating QALYs from the SF-36, SF-12 and the standalone SF-6Dv2 [Internet]. [cited 2023 Dec 8]. https://licensing.sheffield.ac.uk/product/SF-6D/print
Sun S, Luo N, Stenberg E, et al. Sequential multiple imputation for real-world health-related quality of life missing data after bariatric surgery. Int J Environ Res Public Health. 2022;19(17):10827.
Kleiber C, Zeileis A. AER: applied econometrics with R [Internet]. 2020 [cited 2021 Apr 15]. https://CRAN.R-project.org/package=AER
Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley; 1987.
R Core Team. R: a language and environment for statistical computing. [Internet]. Vienna, Austria: R Foundation for Statistical Computing; 2019. https://www.R-project.org/.
StataCorp. Stata statistical software: release 17. College station. StataCorp LLC; 2021.
Kolotkin RL, Andersen JR. A systematic review of reviews: exploring the relationship between obesity, weight loss and health-related quality of life: Quality of life systematic review of reviews. Clin Obes. 2017;7(5):273–89.
Picot J, Jones J, Colquitt J, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess [Internet]. 2009 Sep [cited 2019 Oct 11];13(41). https://www.journalslibrary.nihr.ac.uk/hta/hta13410/
Colquitt JL, Pickett K, Loveman E, et al. Surgery for weight loss in adults [Internet]. 2014 Aug [cited 2017 Feb 6]. (Cochrane Database of Systematic Reviews). Report No.: No.: CD003641. http://onlinelibrary.wiley.com.proxy.kib.ki.se/doi/10.1002/14651858.CD003641.pub4/abstract
Colquitt JL, Picot J, Loveman E, et al. Surgery for obesity. In: The Cochrane Collaboration, editor. Cochrane Database of Systematic Reviews [Internet]. Chichester, UK: John Wiley & Sons, Ltd; 2009 [cited 2016 Jan 19]. http://doi.wiley.com/10.1002/14651858.CD003641.pub3
Lee WJ, Huang MT, Yu PJ, et al. Laparoscopic vertical banded gastroplasty and laparoscopic gastric bypass: a comparison. Obes Surg. 2004;14(5):626–34.
Stenberg E, Näslund I, Persson C, et al. The association between socioeconomic factors and weight loss 5 years after gastric bypass surgery. Int J Obes 2005. 2020;44(11):2279–90.
Funding
Open access funding provided by Umea University. This study was funded and supported by the Swedish Research Council for Health, Working Life and Welfare (project number: 2018–00896).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Consent to Participate
Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Human and Animal Rights/Ethics Approval
The Ethics Authority in Sweden granted ethical permission for analyses of this study (reference number: 2019–03666).
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• The normative value of the SF-6D index is provided for patients with bariatric surgery.
• SF-6D index increased at year 1 post-surgery and maintained at year 2.
• Post-surgery SF-6D index was at the same level as the general population.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sun, S., Stenberg, E., Luo, N. et al. SF-6D Normative Values Among Patients Undergoing Bariatric Surgery: Results Based on Real-World Evidence from the Scandinavian Obesity Surgery Registry (SOReg). OBES SURG 34, 558–567 (2024). https://doi.org/10.1007/s11695-023-07024-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-07024-0