Abstract
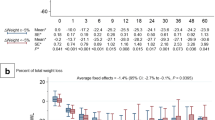
Previous studies investigated low-calorie diets (LCD), very-low-calorie diets (VLCD), and very-low-calorie ketogenic diets (VLCKD) in relation to weight loss and outcomes for bariatric surgery patients. However, the overall effects of these diets on various outcomes remain unclear. This study aimed to assess the impact of preoperative restricted calorie diets on weight, body mass index (BMI), operation time (OT), and hospital stay (HS) in bariatric surgery patients. Seventeen articles were analyzed, revealing the highest weight loss (-8.62) and BMI reduction (-5.75) with VLCKD. Due to insufficient data, the impact of these diets on OT and HS could not be determined. Further interventional studies are required to determine the ideal preoperative diet that achieves optimal weight loss, patient compliance, tolerance, acceptance, and surgical outcomes.









Similar content being viewed by others
References
Dhurandhar NV. What is obesity? Obesity Musings. Int J Obes. 2022;46:1081–2.
Organization WH. World obesity day 2022-accelerating action to stop obesity. Geneva, Switzerland: World Health Organization; 2022.
Murray CJ, Abbafati C, Abbas KM, et al. Five insights from the global burden of disease study 2019. The Lancet. 2020;396:1135–59.
Després J-P, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444:881–7.
Prabhakaran D, Jeemon P, Sharma M, et al. The changing patterns of cardiovascular diseases and their risk factors in the states of India: the Global Burden of Disease Study 1990–2016. Lancet Glob Health. 2018;6:e1339–51.
Pearson-Stuttard J, Zhou B, Kontis V et al. Worldwide burden of cancer attributable to diabetes and high body-mass index: a comparative risk assessment. Elsevier 2018
Furer A, Afek A, Sommer A, et al. Adolescent obesity and midlife cancer risk: a population-based cohort study of 2· 3 million adolescents in Israel. Lancet Diabetes Endocrinol. 2020;8:216–25.
Meijnikman AS, De Block CE, Verrijken A, et al. Predicting type 2 diabetes mellitus: a comparison between the FINDRISC score and the metabolic syndrome. Diabetol Metab Syndr. 2018;10:1–6.
Gadde KM, Allison DB. Combination therapy for obesity and metabolic disease. Curr Opin Endocrinol Diabetes Obes. 2009;16:353–8.
Pontiroli AE, Zakaria AS, Mantegazza E, et al. Long-term mortality and incidence of cardiovascular diseases and type 2 diabetes in diabetic and nondiabetic obese patients undergoing gastric banding: a controlled study. Cardiovasc Diabetol. 2016;15:1–9.
Courcoulas AP, Gallagher JW, Neiberg RH, et al. Bariatric surgery vs lifestyle intervention for diabetes treatment: 5-year outcomes from a randomized trial. J Clin Endocrinol Metab. 2020;105:866–76.
Seventh I. Global Registry Report. 2022. IFSO Registry| International Federation for the Surgery of Obesity and Metabolic Disorders Available online: https://www ifso com/ifso-registry php (accessed on 28 February 2023)
Craig BM, Tseng DS. Cost-effectiveness of gastric bypass for severe obesity. Am J Med. 2002;113:491–8.
Buchwald H, Ikramuddin S, Dorman RB, et al. Management of the metabolic/bariatric surgery patient. Am J Med. 2011;124:1099–105.
Sjöström L, Peltonen M, Jacobson P, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307:56–65.
Van Nieuwenhove Y, Dambrauskas Z, Campillo-Soto A, et al. Preoperative very low-calorie diet and operative outcome after laparoscopic gastric bypass: a randomized multicenter study. Arch Surg. 2011;146:1300–5.
Cassie S, Menezes C, Birch DW, et al. Effect of preoperative weight loss in bariatric surgical patients: a systematic review. Surg Obes Relat Dis. 2011;7:760–7.
Stefura T, Droś J, Kacprzyk A, et al. Influence of preoperative weight loss on outcomes of bariatric surgery for patients under the enhanced recovery after surgery protocol. Obes Surg. 2019;29:1134–41.
Schwingshackl L, Chaimani A, Schwedhelm C, et al. Comparative effects of different dietary approaches on blood pressure in hypertensive and pre-hypertensive patients: a systematic review and network meta-analysis. Crit Rev Food Sci Nutr. 2019;59:2674–87.
Leslie W, Taylor R, Harris L, et al. Weight losses with low-energy formula diets in obese patients with and without type 2 diabetes: systematic review and meta-analysis. Int J Obes. 2017;41:96–101.
Klonoff DC. The beneficial effects of a Paleolithic diet on type 2 diabetes and other risk factors for cardiovascular disease. SAGE Publications 2009; 1229–32
Thackrey E, Chen J, Martino C-R, et al. The effects of diet on weight and metabolic outcomes in patients with double diabetes: A systematic review. Nutrition. 2022;94:111536.
Fontana L, Weiss EP, Villareal DT, et al. Long-term effects of calorie or protein restriction on serum IGF-1 and IGFBP-3 concentration in humans. Aging Cell. 2008;7:681–7.
Alami RS, Morton JM, Schuster R, et al. Is there a benefit to preoperative weight loss in gastric bypass patients? A prospective randomized trial. Surg Obes Relat Dis. 2007;3:141–5.
Colles SL, Dixon JB, Marks P, et al. Preoperative weight loss with a very-low-energy diet: quantitation of changes in liver and abdominal fat by serial imaging–. Am J Clin Nutr. 2006;84:304–11.
Merra G, Gratteri S, De Lorenzo A, et al. Effects of very-low-calorie diet on body composition, metabolic state, and genes expression: a randomized double-blind placebo-controlled trial. Eur Rev Med Pharmacol Sci. 2017;21:329–45.
Castellana M, Conte E, Cignarelli A, et al. Efficacy and safety of very low calorie ketogenic diet (VLCKD) in patients with overweight and obesity: A systematic review and meta-analysis. Rev Endocr Metab Disord. 2020;21:5–16.
Leonetti F, Campanile FC, Coccia F, et al. Very low-carbohydrate ketogenic diet before bariatric surgery: prospective evaluation of a sequential diet. Obes Surg. 2015;25:64–71.
Pilone V, Tramontano S, Renzulli M, et al. Metabolic effects, safety, and acceptability of very low-calorie ketogenic dietetic scheme on candidates for bariatric surgery. Surg Obes Relat Dis. 2018;14:1013–9.
Albanese A, Prevedello L, Markovich M, et al. Pre-operative very low calorie ketogenic diet (VLCKD) vs. very low calorie diet (VLCD): surgical impact. Obes Surg. 2019;29:292–6.
Wolf RM, Oshima K, Canner JK, et al. Impact of a preoperative low-calorie diet on liver histology in patients with fatty liver disease undergoing bariatric surgery. Surg Obes Relat Dis. 2019;15:1766–72.
Hutcheon DA, Hale AL, Ewing JA, et al. Short-term preoperative weight loss and postoperative outcomes in bariatric surgery. J Am Coll Surg. 2018;226:514–24.
Yolsuriyanwong K, Thanavachirasin K, Sasso K, et al. Effectiveness, compliance, and acceptability of preoperative weight loss with a liquid very low-calorie diet before bariatric surgery in real practice. Obes Surg. 2019;29:54–60.
Katsogiannos P, Kamble PG, Boersma GJ, et al. Early changes in adipose tissue morphology, gene expression, and metabolism after RYGB in patients with obesity and T2D. J Clin Endocrinol Metab. 2019;104:2601–13.
Şen O, Türkçapar AG. Effect of pre-operative weight loss on patients’ outcomes undergoing laparoscopic sleeve gastrectomy. Journal of minimal access surgery. 2022;18:260.
Ekici U, Ferhatoglu MF. Perioperative and postoperative effects of preoperative low-calorie restrictive diets on patients undergoing laparoscopic sleeve gastrectomy. J Gastrointest Surg. 2020;24:313–9.
Gils Contreras A, Bonada Sanjaume A, Montero Jaime M, et al. Effects of two preoperatory weight loss diets on hepatic volume, metabolic parameters, and surgical complications in morbid obese bariatric surgery candidates: a randomized clinical trial. Obes Surg. 2018;28:3756–68.
Chakravartty S, Vivian G, Mullholland N, et al. Preoperative liver shrinking diet for bariatric surgery may impact wound healing: a randomized controlled trial. Surg Obes Relat Dis. 2019;15:117–25.
Serafim MP, Santo MA, Gadducci AV et al. Very low-calorie diet in candidates for bariatric surgery: change in body composition during rapid weight loss. Clinics. 2019;74
Sivakumar J, Chong L, Ward S, et al. Body composition changes following a very-low-calorie pre-operative diet in patients undergoing bariatric surgery. Obes Surg. 2020;30:119–26.
Bakker N, van den Helder RS, Geenen RW, et al. Four weeks of preoperative omega-3 fatty acids reduce liver volume: a randomised controlled trial. Obes Surg. 2019;29:2037–44.
Salman MA, Qassem MG, Aboul-Enein MS, et al. Effect of preoperative diet regimen on liver size before laparoscopic sleeve gastrectomy in morbidly obese patients. Surg Endosc. 2022;36:2981–6.
González-Pérez J, Sánchez-Leenheer S, Delgado AR, et al. Clinical impact of a 6-week preoperative very low calorie diet on body weight and liver size in morbidly obese patients. Obes Surg. 2013;23:1624–31.
O’Kane M, Parretti HM, Pinkney J, et al. British Obesity and Metabolic Surgery Society Guidelines on perioperative and postoperative biochemical monitoring and micronutrient replacement for patients undergoing bariatric surgery—2020 update. Obes Rev. 2020;21:e13087.
Stegenga H, Haines A, Jones K, et al. Identification, assessment, and management of overweight and obesity: summary of updated NICE guidance. BMJ. 2014;349:g6608.
Raynor HA, Champagne CM. Position of the Academy of Nutrition and Dietetics: Interventions for the Treatment of Overweight and Obesity in Adults. J Acad Nutr Diet. 2016;116:129–47.
Roitman JL, Herridge M. ACSM’s resource manual for guidelines for exercise testing and prescription. Lippincott Williams & Wilkins; 2012.
Schiavo L, Scalera G, Sergio R, et al. Clinical impact of Mediterranean-enriched-protein diet on liver size, visceral fat, fat mass, and fat-free mass in patients undergoing sleeve gastrectomy. Surg Obes Relat Dis. 2015;11:1164–70.
Alvarado R, Alami R, Hsu G, et al. The impact of preoperative weight loss in patients undergoing laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2005;15:1282–6.
Hollis G, Franz R, Bauer J, et al. Implementation of a very low calorie diet program into the pre-operative model of care for obese general elective surgery patients: outcomes of a feasibility randomised control trial. Nutr Diet. 2020;77:490–8.
Faria SL, Faria OP, de Almeida CM, et al. Effects of a very low calorie diet in the preoperative stage of bariatric surgery: a randomized trial. Surg Obes Relat Dis. 2015;11:230–7.
Colangeli L, Gentileschi P, Sbraccia P, et al. Ketogenic Diet for Preoperative Weight Reduction in Bariatric Surgery: A Narrative Review. Nutrients. 2022;14:3610.
Cicero AF, Benelli M, Brancaleoni M, et al. Middle and long-term impact of a very low-carbohydrate ketogenic diet on cardiometabolic factors: a multi-center, cross-sectional, clinical study. High Blood Press Cardiovasc Prev. 2015;22:389–94.
Ricci A, Idzikowski MA, Soares CN, et al. Exploring the mechanisms of action of the antidepressant effect of the ketogenic diet. Rev Neurosci. 2020;31:637–48.
Kossoff EH, Zupec-Kania BA, Auvin S, et al. Optimal clinical management of children receiving dietary therapies for epilepsy: Updated recommendations of the International Ketogenic Diet Study Group. Epilepsia Open. 2018;3:175–92.
McKechnie T, Lee Y, Dionne J, et al. Very low energy diets prior to bariatric surgery may reduce postoperative morbidity: a systematic review and meta-analysis of randomized controlled trials. Front Nutr. 2023;10:1211575.
Bueno NB, de Melo ISV, de Oliveira SL, et al. Very-low-carbohydrate ketogenic diet v. low-fat diet for long-term weight loss: a meta-analysis of randomised controlled trials. Br J Nutr. 2013;110:1178–87.
Stenberg E, dos Reis Falcao LF, O’Kane M, et al. Guidelines for perioperative care in bariatric surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations: a 2021 update. World J Surg. 2022;46:729–51.
Pondel N, Liśkiewicz D, Liśkiewicz A. Dieta ketogeniczna-mechanizm działania i perspektywy zastosowania w terapii: dane z badań klinicznych. Postępy Biochemii 2020;66:270â 86-â 86
Cenci L, Paoli A, Omar HR, et al. Internist, anesthesiologist and surgeon use of ketogenic diet. Minerva Gastroenterol Dietol. 2018;64:84–93.
w Polsce KLR. Polskie Towarzystwo Medycyny Rodzinnej. Polskie Towarzystwo Badań nad Otyłością: https://107sw mil pl/udary/pacjent/wp-content/uploads/2019/11/1211. 2019
Kim JJ, Rogers AM, Ballem N, et al. ASMBS updated position statement on insurance mandated preoperative weight loss requirements. Surg Obes Relat Dis. 2016;12:955–9.
Mechanick JI, Apovian C, Brethauer S, et al. Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures–2019 update: cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Surg Obes Relat Dis. 2020;16:175–247.
Acknowledgements
The authors would like to thank the Research Development Center Of Sina Hospital for their technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Statement
For this type of study formal consent is not required.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
1. VLCKD was more effective on weight loss and BMI, and the effectiveness of the diets on the OT and HS could not be investigated.
2. Despite the growing interest in preoperative restricted calorie diets, there is a limited number of studies that definitively establish their effectiveness in patients preparing for bariatric surgery.
3. Further research is required to better understand the optimal diet type, duration, and compliance factors to achieve the best outcomes for patients undergoing bariatric surgery.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khalooeifard, R., Rahmani, J., Ghoreishy, S.M. et al. Evaluate the Effects of Different Types of Preoperative Restricted Calorie Diets on Weight, Body Mass Index, Operation Time and Hospital Stay in Patients Undergoing Bariatric Surgery: a Systematic Review and Meta Analysis Study. OBES SURG 34, 236–249 (2024). https://doi.org/10.1007/s11695-023-06973-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06973-w