Abstract
Background
Some 28% of the Scottish population suffer from obesity. Bariatric procedures per population carried out in England when compared to Scotland (NBSR 2018) are significantly higher. Primary care practitioners (PCP) influence equality of access to secondary care bariatrics and frequently manage post-operative bariatric patients. Examining changes in PCP knowledge and attitude could improve access to bariatric procedures in Scotland.
Methods
Following a sample pilot, all PCPs within three Scottish NHS health boards were emailed a questionnaire-based survey (2011; n = 902). A subsequent 10-year follow-up encompassed a greater scope of practice, additionally distributed to all PCPs in five further health boards (2021; n = 2049).
Results
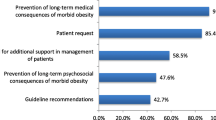
Some 452 responses were achieved (2011, 230; 2021, 222). PCPs felt bariatric surgery offered a greater impact in both weight management and that of obesity-related diseases (p < .0001). More PCPs were aware of local bariatric surgical referral criteria (2011, 43%; 2021, 57% (p = .003)), and more made referrals (2011, 60%; 2021, 72% (p = .018)) but were less familiar with national bariatric surgical guidelines (2011, 70%; 2021, 48% (p < .001)). Comfort at managing post-operative bariatric surgical patients were unchanged (2011, 24%; 2021, 27% (p = .660)). Minimal progress through dietetic-lead weight management services, plus rejection of patients thought to be good candidates, was reasons for referral hesitancy.
Conclusion
Over 10 years, PCPs were more aware of local referral criteria, making increased numbers of referrals. Knowledge deficits of national guidelines remain, and overwhelmingly PCPs do not feel comfortable looking after post-operative bariatric surgical patients. Further research into PCP educational needs, in addition to improving the primary to secondary care interface, is required.
Graphical Abstract

Similar content being viewed by others
Data Availability
Informed consent was obtained from all individuals completing the questionnaire. Data can be obtained upon request from authors.
References
Carlsson LMS, Peltonen M, Ahlin S, Anveden Å, Bouchard C, et al. Bariatric surgery and prevention of type 2 diabetes in Swedish obese subjects. N Engl J Med. 2012;367:695–704.
Perego L, Pizzocri P, Corradi D, et al. Circulating leptin correlates with left ventricular mass in morbid (grade III) obesity before and after weight loss induced by bariatric surgery: a potential role for leptin in mediating human left ventricular hypertrophy. J Clin Endocrinol Metab. 2005;90(7):4087–93. https://doi.org/10.1210/jc.2004-1963.
Yusefzadeh H, Rashidi A, Rahimi B. Economic burden of obesity: a systematic review. Soc Health Behav. 2019;2:7–12.
National Bariatric Surgery Registry. The UK National Bariatric Surgery Registry Third Registry Report. 2020. https://www.e-dendrite.com/NBSR2020. Accessed 12 Oct 2022.
The Scottish government, Scottish Health Survey 2020 Volume 1; main report. September 2020. Accessed 20/03/2022. Chapter 4: Diet, Obesity & Food Insecurity - Scottish Health Survey – telephone survey – August/September 2020: main report - gov.scot (http://www.gov.scot)
Boyers D, Retat L, Jacobsen E, et al. Cost-effectiveness of bariatric surgery and non-surgical weight management programmes for adults with severe obesity: a decision analysis model. Int J Obes. 2021;45:2179–90. https://doi.org/10.1038/s41366-021-00849-8.
Welbourn R, le Roux CW, Owen-Smith A, Wordsworth S, Blazeby JM. Why the NHS should do more bariatric surgery; how much should we do? BMJ. 2016May;11(353):i1472. https://doi.org/10.1136/bmj.i1472.
Busetto L, Dicker D, Azran C, et al. Obesity management task force of the European Association for the study of obesity released “practical recommendations for the post-bariatric surgery medical management.” Obes Surg. 2018;28:2117–21. https://doi.org/10.1007/s11695-018-3283-z.
Balduf LM, Farrell TM. Attitudes, beliefs, and referral patterns of PCPs to bariatric surgeons. J Surg Res. 2008Jan;144(1):49–58.
Sansone RA, McDonald S, Wiederman MW, Ferreira K. Gastric bypass surgery: a survey of primary care physicians. Eat Disord. 2007;15(2):145–52.
Foster GD, Wadden TA, Makris AP, Davidson D, Sanderson RS, Allison DB, Kessler A. Primary care physicians’ attitudes about obesity and its treatment. Obes Res. 2003;11(10):1168–77.
Weaver L, Beebe TJ, Rockwood T. The impact of survey mode on the response rate in a survey of the factors that influence Minnesota physicians’ disclosure practices. BMC Med Res Methodol. 2019;19:73. https://doi.org/10.1186/s12874-019-0719-7.
Hebl MR, Xu J. Weighing the care: physicians’ reactions to the size of a patient. Int J Obes Relat Metab Disord. 2001;25:1246–52.
Harvey EL, Hill AJ. Health professionals’ views of overweight people and smokers. Int J Obes Relat Metab Disord. 2001;25(8):1253–61.
Tork S, Meister KM, Uebele AL, et al. Factors influencing primary care physicians’ referral for bariatric surgery. JSLS. 2015;19(3):e2015.00046. https://doi.org/10.4293/JSLS.2015.00046.
Panteliou E, Miras AD. What is the role of bariatric surgery in the management of obesity? Climacteric. 2017;20(2):97–102. https://doi.org/10.1080/13697137.2017.1262638.
Boyers D, Retat L, Jacobsen E, et al. Cost-effectiveness of bariatric surgery and non-surgical weight management programmes for adults with severe obesity: a decision analysis model. Int J Obes. 2021;45:2179–90. https://doi.org/10.1038/s41366-021-00849-8.
Welbourn R, le Roux CW, Owen-Smith A, Wordsworth S, Blazeby JM. Why the NHS should do more bariatric surgery; how much should we do? BMJ. 2016;353:i1472. https://doi.org/10.1136/bmj.i1472. (Published 2016 May 11).
Arhi C, Karagianni C, Howse L, et al. The effect of participation in tier 3 services on the uptake of Bariatric surgery. Obes Surg. 2021;31:2529–36. https://doi.org/10.1007/s11695-021-05303-2.
O’Kane M, Parretti HM, Pinkney J, et al. British obesity and metabolic surgery society guidelines on perioperative and postoperative biochemical monitoring and micronutrient replacement for patients undergoing bariatric surgery—2020 update. Obesity Reviews. 2020;21:e13087. https://doi.org/10.1111/obr.13087
Durrer Schutz D, Busetto L, Dicker D, Farpour-Lambert N, Pryke R, Toplak H, Widmer D, Yumuk V, Schutz Y. European practical and patient-centred guidelines for adult obesity management in primary care. Obes Facts. 2019;12:40–66. https://doi.org/10.1159/000496183.
Conaty EA, Denham W, Haggerty SP, et al. Primary care physicians’ perceptions of bariatric surgery and major barriers to referral. Obes Surg. 2020;30:521–6. https://doi.org/10.1007/s11695-019-04204-9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
1. Investigating understanding of PCPs in Scotland towards bariatric surgery.
2. Overall, greater appreciation of operative weight loss surgery is achieved.
3. Demonstrable dissatisfaction of tier 3 weight loss services by PCPs.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Douglass, B., Lau, S.H., Parkin, B. et al. Changing Knowledge and Attitudes towards Bariatric Surgery in Primary Care: a 10-Year Cross-Sectional Survey. OBES SURG 34, 71–76 (2024). https://doi.org/10.1007/s11695-023-06934-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06934-3