Abstract
Background
The purpose of this study was to determine intern physicians’ attitudes and beliefs toward obesity and individuals with obesity and the frequency at which they encounter discriminatory language in their work environments.
Methods
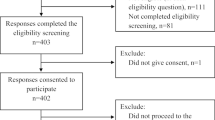
This cross-sectional study was performed with intern physicians at the Ondokuz Mayıs University Medical Faculty in Samsun, Türkiye. A questionnaire was employed for data collection (Appendix). Two hundred eighteen (82.2%) interns took part in the study. The questionnaire consisted of 53 questions in five sections, and included the attitudes toward obese persons (ATOP) and beliefs about obese persons (BAOP) scales.
Results
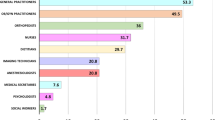
The interns most frequently cited genetic factors (98.1%) and endocrine disorder-metabolic disorders (98.1%) as non-behavioral causes of obesity, and overeating (96.2%) and physical immobility (96.2%) as behavioral causes. Lifestyle changes and exercise were most frequently recommended for treatment. The interns’ attitudes toward individuals with obesity were very slightly negative, but close to neutral. Analysis showed that 46.8% of the interns reported hearing members of academic staff, intern physicians, or health workers make negative or derogatory comments or jokes about obese patients during their education, while 22.0% reported witnessing an obese patient being subjected to discriminatory treatment in the hospital environment.
Conclusion
Medical faculties must develop curricula aimed at comprehensively addressing obesity-related bias. Such a curriculum should allow students to reflect on their biases, be aimed at reducing the effect of those biases on patient communication, and involve strategies directed toward eliminating those effects from physicians’ treatment decisions.
Graphical Abstract

Similar content being viewed by others
Data Availability
The data that support the findings of this study are available on reasonable request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Code Availability
Statistical analyses were conducted in SPSS 21.0.
References
World Health Organization. Obesity and overweight. Accessed 10 Jan 2023.
World Health Organization. The Global Health Observatory. Explore A World Of Health Data. https://www.who.int/data/gho/data/indicators/indicator-details/GHO/prevalence-of-obesity-among-adults-bmi-=-30-(crude-estimate. Accessed 10 Jan 2023.
Türkiye Nutrition and Health Survey Ministry of Health Türkiye. https://hsgm.saglik.gov.tr/depo/birimler/saglikli-beslenme-hareketli-hayat-db/Yayinlar/kitaplar/TBSA_RAPOR_KITAP_20.08.pdf. Accessed 10 Jan 2023.
Stigma GE. Noteson the management of spoiled identity. Prentice–Hall; 1963.
Cohen R, Shikora S. Fighting weight bias and obesity stigma: a call for action. Obes Surg. 2020;30(5):1623–4.
Rodhain A, Gourmelen A. Obesity: the link between stigma and perceived responsibility. J Mark Manag. 2018;34(15–16):418–1439.
Carr D, Friedman MA. Is obesity stigmatizing? Body weight, perceived discrimination, and psychological well-being in the United States. J Health Soc Behav. 2005;46(3):244–59.
Guardabassi V, Tomasetto C. Weight status or weight stigma? Obesity stereotypes-Not excess weight-Reduce working memory in school-aged children. J Exp Child Psychol. 2020;189:104706.
Lessard LM, Juvonen J. Weight stigma in the school setting: the role of inclusive weight climate—a commentary. J Sch Health. 2020;90(7):507–10.
Brewis A, Sturtz SC, Wutich A. Obesity stigma as a globalizing health challenge. Glob Health. 2018;14:1–6.
Sezgin D, Yıldırım İE, Karaaslan YS. Discrimination and stigma in obesity. In: Kapital Yayınları. İstanbul, (Turkish); 2020.
Alenazy FR, Almutairi A. The effect of obesity stigma on obese people, Saudi Arabia, 2020. World Fam Med. 2021;19(1):65–74.
Puhl R, Moss-Racusin CA, Schwartz MB, et al. Weight stigmatization and bias reduction: perspectives of overweight and obese adults. Health Educ Res. 2008;2:347–58.
Chakravorty T. Fat shaming is stopping doctors from helping overweight patients—here’s what medical students can do about it. BMJ. 2021;375. https://doi.org/10.1136/bmj.n2830.
Rubino F, Puhl RM, Cummings DE, et al. Joint international consensus statement for ending stigma of obesity. Nat Med. 2020;26:485–97.
Farrow CV, Tarrant M. Weight-based discrimination, body dissatisfaction and emotional eating: the role of perceived social consensus. Psychol Health. 2009;24(9):1021–34.
Berdah C. Obésité ettroubles psychopathologiques. Ann Méd-Psychol Rev Psychiatr. 2010;168(3):184–90.
World Health Organization. WHO acceleration plan to stop. Obesity. https://iris.who.int/bitstream/handle/10665/370281/9789240075634-eng.pdf?sequence=1. Accessed 30 Sep 2023.
Flint S. Obesity stigma: Prevalence and impact in healthcare. Br J Obes. 2015;1(1):14–8.
Allison DB, Basile VC, Yuker HE. The measurement of attitudes toward and beliefs about obese persons. Int J Eat Disord. 1991;10(5):599–607.
Dedeli O, Bursalioglu SA, Deveci A. Validity and reliability of the Turkish version of the attitudes toward obese persons scale and the beliefs about obese persons scale. Clin Nurs Stud. 2014;2(4):105.
Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health. 2010;100(6):1019–28.
Epstein L, Ogden J. A qualitative study of GPs’ views of treating obesity. Br J Gen Pract. 2005;55:750–4.
Campbell K, Engel H, Timperio A, et al. Obesity management: Australian general practitioners’ attitudes and practices. Obes Res. 2000;8:459–66.
Thuan JF, Avignon A. Obesity management: attitudes and practices of French general practitioners in a region of France. Int J Obes. 2005;29:1100–6.
Harvey EL, Hill AJ. Health professionals‘ views of overweight people and smokers. Int J Obes. 2001;25:1253–61.
Hebl MR, Xu J. Weighing the care: Physicians reactions to the size of a patient. Int J Obes Relat Metab Dis. 2001;25:1246–52.
Foster GD, Wadden TA, Makris AP, et al. Primary care physicians’ attitudes about obesity and its treatment. Obes Res. 2003;11:1168–77.
Bocquier A, Verger P, Basdevant A, et al. Overweight and obesity: knowledge, attitudes, and practice of general practitioners in France. Obes Res. 2005;13:787–95.
Harvey E, Summerbell CD, Kirk SF, et al. Dieticians’ views of overweight and obese people and reported management practices. J Hum Nutr Diet. 2002;15:331–327.
Brandsma L. Physician and patient attitudes toward obesity, eating disorders. Eat Disord. 2005;3(2):201–11.
O’Donoghue G, McMahon S, Holt A, et al. Obesity bias and stigma, attitudes and beliefs among entry-level physiotherapy students in the Republic of Ireland: a cross sectional study. Physiotherapy. 2021;112:55–63.
Tanas R, Bernasconi S, Marsella M, et al. What’s the name? Weight stigma and the battle against obesity. Ital J Pediatr. 2020;46(1):1–3.
Hartlev M. Stigmatisation as a public health tool against obesity—a health and human rights perspective. Eur J Health Law. 2014;21:365–86.
Ip EH, Marshall MS, Vitolins M, et al. Measuring medical student attitudes and beliefs regarding obese patient. Acad Med: J Assoc Am Med Coll Acad Med. 2013;88(2):282–9.
Soto L. Beliefs, attitudes and phobias among Mexican medical and psychology students towards people with obesity. Nutr Hosp. 2014;30(1):37–41.
Poustch Y, Saks NS, Piasecki AK, et al. Brief intervention effective in reducing weight bias in medical students. Fam Med. 2013;45(5):345–8.
Akman M, Kıvrakoğlu E, Çifçili S, et al. Weight bias among primary care health professionals: personal attitude matters. Obes Metab Milan. 2010;6(2–3):63–8.
Parıldar H, Tuncer OU, Şahin MK, et al. Are patients with obesity “scapegoats”? The obesity prejudice levels of health care workers in Turkey. Rev Assoc Med Bras. 2021;67:1785–92.
Tomiyama AJ, Finch LE, Belsky ACI. Weight bias in 2001 versus 2013: contradictory attitudes among obesity researchers and health professionals. Obesity. 2015;23(1):46–53.
Sabin A, Marini M, Nosek BA. Implicit and explicit anti-fat bias among a large sample of medical doctors by BMI, race/ethnicity and gender Janice. PLoS One. 2012;7(11):e48448.
Schwartz MB, Chambliss HO, Brownell KD, et al. Weight bias among health professionals specializing in obesity. Obes Res. 2003;11:1033–9.
Miller DP, Spangler JG, Vitolins MZ, et al. Are medical students aware of their anti-obesity bias? Acad Med: J Assoc Am Med Coll. 2013;88(7):978.
Flint SW, Hudson J, Lavallee D. UK adults‘ implicit and explicit attitudes towards obesity: a cross-sectional study. BMC Obesity. 2015;2:31.
Cotugna N, Malick A. Following a calorie-restricted diet may help in reducing healthcare students’ fat-phobia. J Community Health. 2010;35:321–4.
Latner JD, Stunkard AJ, Wilson GT. Stigmatized students: age, sex, and ethnicity effects in the stigmatization of obesity. Obes Res. 2005;13:1226–2123.
Phelan MS, Dovidio JF, Puhl RM, et al. Implicit and explicit weight bias in a national sample of 4732 medical students: the medical student CHANGES study. Obesity (Silver Spring. 2014;22(4):1201–8.
Davis NJ, Shishodia H, Taqui B, et al. Resident physician attitudes and competence about obesity treatment: need for improved education. Med Educ Online. 2008;13:5.
Khandalavala B, Rojanala A, Geske JA, et al. Obesity bias in primary care providers. Fam Med. 2014;46(7):532–5.
Tomiyama AJ, Finch LE, Belsky AC, et al. Weight bias in 2001 versus 2013: Contradictory attitudes among obesity researchers and health professionals. Obesity. 2015;23:46–53.
Oberrieder H, Walker R, Monroe D, et al. Attitudes of dietetics students and registered dietitians towards obesity. J Am Diet Assoc. 1995;95:914–9.
Wadden TA, Anderson DA, Foster GD, et al. Obese women’s perceptions of their physicians’ weight management attitude and practices. Arch Fam Med. 2000;9:854–60.
Meadows A, Barreto M, Dovidio JF, et al. Signaling hostility: the relationship between witnessing weight-based discrimination in medical school and medical student well-being. J Appl Soc Psychol. 2021. https://doi.org/10.1111/jasp.12847.
Wear D, Aultman JM, Varley JD, et al. Making fun of patients: medical students’ perceptions and use of derogatory and cynical humor in clinical settings. Acad Med. 2006;81(5):454–62.
Wear D, Aultman JM, Zarconi J, et al. Derogatory and cynical humour directed towards patients: views of residents and attending doctors. Med Educ. 2009;43(1):34–41.
Geier AB, Foster GD, Womble LG. The relationship between relative weight and school attendance among elementary school children. Obesity. 2007;15–8:2157–61.
Puhl RM, Luedicke J, Grilo CM. Obesity bias in training: attitudes, beliefs, and observations among advanced trainees in professional health disciplines. Obesity (Silver Spring). 2014;22:1008–15.
Berman MI, Hegel MT. Weight bias education for medical school faculty: workshop and assessment. J Nutr Educ Behav. 2017;49(7):605–6.
Lewis S, Thomas SL, Blood RW. How do obese individuals perceive and respond to the different types of obesity stigma that they encounter in their daily lives? A qualitative study. Soc Sci Med. 2011;73:1349–56.
Mastrocola MR, Roque SS, Benning LV, et al. Obesity education in medical schools, residencies, and fellowships throughout the world: a systematic review. Int J Obes. 2020;44(2):269–79.
Katz NJ, Neary E, Tang N, et al. Undergraduate medical education interventions aimed at managing patients with obesity: a systematic review of educational effectiveness. Obes Rev. 2021;22(10):e13329.
Crowley J, Ball L, Hiddink GJ. Nutrition in medical education: a systematic review. Lancet Planet Health. 2019;3:e379–89.
Acknowledgements
We would like to thank all the participating students.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
Ethical approval was granted by the Ondokuz Mayıs University Clinical Research Ethical Committee before the study commenced (IRB no. OMUKAEK 2022/101).
Consent to Participate
Participants gave their consent to partake in this study. Participation was voluntary, and consent was collected as deemed appropriate by the ethics committee.
Consent for Publication
When providing consent to take part in the study, participants acknowledged that de-identifed data from the study would be published.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Intern physicians exhibit negative attitudes toward individuals with obesity.
• Intern physicians mostly highlighted non-behavioral factors as causes of obesity.
• Intern physicians stated that they had heard healthcare professionals making derogatory comments or jokes about individuals with obesity.
Appendix. Questionnaire.
Appendix. Questionnaire.



Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aker, S., Şahin, M.K. Obesity Bias and Stigma, Attitudes, and Beliefs Among Intern Doctors: a Cross-sectional Study from Türkiye. OBES SURG 34, 86–97 (2024). https://doi.org/10.1007/s11695-023-06919-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06919-2