Abstract
Background
The COVID-19 pandemic was initially responsible for a global restricted access to healthcare resources including the follow-up of at-risk populations such as bariatric patients. We substituted face-to-face bariatric follow-up outpatient clinics (FTFC) with teleclinics (TC) during the lockdown.
Material and Methods
We retrospectively reviewed data collected on all patients scheduled for TC during the French lockdown period (March 15 to May 15, 2020) (N = 87). Our aims were to present the patients’ outcomes at one and 2 years post-TC implementation and describe patient/practitioner satisfaction.
Results
Seven (8%) patients required FTFC, and 80 (92%) underwent TC (study population) for preoperative bariatric assessment (N = 3) and postoperative follow-up (N = 77) after 23.6 ± 29 months following surgery. TC was performed with video and audio (N = 46; 57.5%) or audio alone when video was impossible (N = 34; 42.5%). Sixteen (20%) patients presented at least one complication identified at the first TC and were managed accordingly. There were no readmissions at 30/90 days post-TC. At 1-year after the first TC, overall follow-up rate was 94.9% (TC: 73% vs FTFC: 27%). Patients surveyed on the main advantages of TC over FTFC (N = 46) cited: saving time (97.8%) at a mean 3.9 ± 6.4 h saved per TC, work-advantages (94.3%), and comparable relevance of TC (84.8%). At 2 years post-TC implementation, follow-up rate was 93.5% and satisfaction rate was 80%, with 33% of patients preferring to return to FTFC.
Conclusions
TC is a satisfactory substitute for FTFC, enabling continued bariatric follow-up during and beyond the pandemic setting without compromising patient safety. However, the modest satisfaction outcomes at 2 years highlight a need to discuss follow-up preferences in order to achieve optimal outcomes.
Graphical Abstract

Similar content being viewed by others
Introduction
Obesity is a fast-rising global healthcare issue correlated with onset of obesity-related diseases and premature death [1,2,3]. Bariatric surgery (BS) is a safe and effective treatment for long-term weight loss [4] and longer life expectancy compared to medical management [5]. Severe obesity (BMI > 35 kg/m2) has recently been identified as an independent predictor of severe infection, hospitalization, intensive care unit admission, and death following SARS-CoV-2 infection [6, 7], including in various surgical settings [8, 9]. During the initial phase of the COVID-19 pandemic, global data showed that 81.7% of surgical procedures for benign diseases and 94% of bariatric procedures have been postponed worldwide [10, 11], along with the attending follow-up clinics. During this period, the regulations governing the use of telemedicine (TM) rapidly evolved to facilitate, secure and warranted widespread use of TM [12], and multiple consensus statements were rapidly issued to provide guidance on surgical care, including urgent implementation and utilization of TM via teleclinics (TC) to maintain unbroken follow-up whatever the pressure on national healthcare systems [13,14,15,16].
Several studies have shown that TM integrated into weight-loss programs is a feasible and efficient option whether implemented before [17] or during the pandemic [18]. In this particularly challenging pandemic period, TC was proposed as a promising short-term substitute to face-to-face follow-up clinics (FTFC) for more than half of bariatric patients [19], improving postoperative follow-up but only for non-surgical practitioners [20]. Although TC was rapidly and widely implemented to tackle urgent outpatient and inpatient issues [21], few studies have assessed the impact of TC adoption in BS practice [22] on mid-to-long-term post-pandemic outcomes. Here, to address this gap, we investigated patient-reported and practitioner-reported satisfaction rates and patient outcomes at 1 and 2 years after the first TC performed during the first COVID-19 lockdown in France.
Material and Methods
Patients and Ethics
During the first COVID-19 lockdown in France (i.e., from 15 March to 15 May, 2020), all consecutive patients scheduled for a preoperative or postoperative bariatric follow-up appointment at the department of digestive surgery, Pitié-Salpêtrière University Hospital, Sorbonne Université (France), were proposed consultation via a virtual follow-up clinic (TC) and included in the study. The postoperative assessments were scheduled in accordance with the recommendations of the French national health authority (Haute Autorité de Santé) [23]. TC were performed according to the French telehealth guidelines [12] via a dedicated free-of-charge institutional telehealth platform (Ortif, Sesan®) enabling secure voice and video exchanges and transmission of medical documents. All patients received login details prior to their TC (https://ortif.sante-idf.fr/portail/#/fr/index). If the connection was not satisfactory, the patient was phone called to complete the visit. In the event of suspicion of a clinical complication and/or when the patient was impossible to contact, a conventional face-to-face interview was scheduled. During the TC, follow-up–related data such as weight change, vitamin supplementation regimen, food tolerance, abdominal pain, adverse events, and blood test results was collected as usually performed in the course of conventional follow-up. Using our ongoing deeply phenotyped BS cohort (“BARICAN,” registered under CNIL [French data privacy agency] No. 1222666), we retrospectively retrieved each patient’s baseline clinical characteristics and perioperative data. Ethical approval was obtained from the Ile-de-France-1 institutional review board (No. 13533).
Satisfaction Questionnaire
At 1 and 2 years post-TC implementation (March–May 2021 and 2022), all patients who underwent a TC during the study period were systematically phone called. The patients and bariatricians involved in TC follow-up (surgeon, nutritionist) were asked to answer, on a voluntary basis, multiple specific questions addressing TC satisfaction, usefulness, accessibility to the tool, quality of communication, future bariatric follow-up preferences, and the limits and constraints and potential improvements. The answers were given using a 5-point Likert scale.
Statistical Analysis
Continuous demographic and outcome variables were expressed as mean ± standard deviation. Categorical variables were expressed as number and percentage. Statistical analyses were performed using JMP version 13.0.0 (SAS Institute, Cary, NC) software.
Results
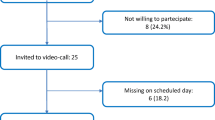
Study Population — First TC Performed
In total, 87 patients were scheduled for a virtual bariatric follow-up TC during the first lockdown period. TC was not possible in 7 post-operative patients (8%): we systematically scheduled an FTFC for all these patients, which 4 (57.1%) patients attended (Fig. 1). Eighty patients (92%) underwent TC for preoperative bariatric assessment (N = 3) or for postoperative follow-up (N = 77) after a mean delay of 23.7 ± 29 months following BS (Fig. 1). The baseline characteristics of these 80 patients are detailed in Table 1. During the first TC, a rescue phone call was performed in 34 (42.5%) patients due to limited internet connectivity (N = 22; 27.5%) or limited audio and/or video compatibility with the interface (N = 12; 15%). In 3 (3.7%) patients, a conventional face-to-face visit was organized following the TC to rule out complications (N = 2) or at the patient’s request (N = 1). At completion of the TC procedure, 72 patients (90%) agreed to schedule the next post-operative follow-up visit with the surgeon using TC. There were no unplanned admissions, resurgeries, or mortalities for BS-related complications at 30 and 90 days post-TC. All patients attending TC at the preoperative bariatric assessment were operated (N = 3) once France resumed bariatric surgery.
Post-TC Outcomes
At 1 year, two patients (2.5%) with active multidisciplinary follow-up asked to transfer follow-up to another center nearer to their home, and four patients (5.1%) were lost to follow-up (Fig. 1). Overall, 74 patients (94.9%) were in active follow-up by TC (N = 54; 73%) or conventional FTFC follow-up (N = 20; 27%) justified by either acute medical issues requiring reinforced follow-up (N = 16; 73%), patient preference (N = 3; 14%), or concomitant hospitalization unrelated to BS (N = 1; 4%). One patient (1.2%) required an unplanned readmission at the emergency department for transient abdominal pain at 1 year post-TC implementation and 2 weeks before their next scheduled TC follow-up appointment. The next follow-up visit in surgery was systematically scheduled for TC in all patients.
The audit at 2 years post-TC implementation showed a total of 5 patients (6.4%) lost to follow-up after a mean time of 99.3 ± 299 months post-surgery (Fig. 1). Seventy-three patients (93.5%) still had active follow-up in surgery with TC in all cases. Two patients were readmitted between year 1 and year 2 post-BS: one for acute intestinal obstruction caused by a retrograde jejuno-jejunal intussusception which required emergency surgery (N = 1) and one anemia requiring iron infusion (N = 1), without mortality. Among the 7 patients who could not attend the first TC and were offered an FTFC appointment during the lockdown, three (42.7%) were immediately lost to follow-up, and one (14.3%) was lost to follow-up 1 year later. To date, three of these 7 patients (42.8%) are in active follow-up, all via FTFC.
Patient and Practitioner Satisfaction with TC
In total, 46 (62.2%) and 30 (41.1%) patients agreed to answer the survey at 1 and 2 years post-TC implementation, respectively. The details of the audit are presented in Tables 2 and 3. Overall, at 2 years, 24 of the 30 (80%) respondent patients expressed satisfaction with post-surgery TC follow-up. Ten patients (33%) patients were not satisfied with the interface at 2 years. None of these 10 patients had experienced readmission at 90 days post-TC, and 9 of these patients (90%) had complete uneventful follow-up. The patient-stated benefits of TC over FTFC are presented in Table 4.
Discussion
The key findings of this study are as follows: (1) FTFC was successfully substituted with TC during COVID-19 lockdowns in 91.9% of BS patients scheduled for in-clinic follow-up; (2) gold-standard TC combining audio and video was fully achieved for 57.5% of patients, with phone-only TC alone in the rest of the population; (3) there was no unplanned readmissions at 90 days post-TC; (4) 2 years after TC implementation, only 6.4% of patients were lost to follow-up; (5) although 80% of patients expressed overall satisfaction with TC, 33% would prefer to return to FTFC, whereas all practitioners wished to continue with TC, suggesting that personalized follow-up with TC or alternative TC and FTFC should be organized the future as per patient preferences.
When the World Health Organization officially declared COVID-19 a pandemic in March 2020 [24], the lack of effective therapies led the medical community to implement innovative preventive follow-up strategies to maintain normal patient care while limiting potential virus transmission, especially in frail populations at risk of severe forms such as patients with obesity [7]. The need for social distancing thus acted as a powerful catalyzer for rapid regulations on TM health policies [12] and TM implementation [25] to maintain medical and surgical services [21]. A recent registry insurance study in Michigan recently showed that the proportion of TC in surgery increased rapidly after the pandemic broke out, ultimately reaching 34.6% of all visits (versus < 1% before). It seems very likely that this paradigm shift was enabled by a combination of commitment from healthcare providers [26, 27], maturing telehealth technologies and the related governing regulations [28], and patient engagement with the dedicated platforms. Thus far, several reports based on online questionnaires have shown that bariatric patients were familiar with using the Internet [29, 30] to search for bariatric-related information, with 95.1% of bariatric patients having a connection [31]. Not surprisingly, 80 of the 87 patients (91.9%) in our study population agreed to a first bariatric TC, with only 27.5% of the patients reporting limited web connectivity.
Here TC emerged as a safe alternative to FTFC in lockdown, as no patients were unexpectedly readmitted within 30 and 90 days following these first virtual appointments. Interestingly, data from a nationwide study showed that postoperative readmission was a critical event following bariatric surgery as it was associated with a fivefold increase in mortality when patients were admitted into another center [32]. This data suggests that TC is a promising tool to reinforce the bariatric patient care pathway and engagement with the multidisciplinary team and therefore a potential lever to reduce avoidable postoperative morbidity and mortality.
The French regulations governing TC [12] recommend the use of video and audio via appropriately authorized purpose-dedicated platforms or audio only if the experience with the interface fails to ensure satisfactory practitioner-patient communication. Here we performed a “rescue” phone call TC in 34 (43%) patients. To date, there has been scarce literature examining these issues in detail. Runfola et al. [19] reported data in 19 patients who attended a video bariatric clinic, but did not give any data on any rescue phone calls needed. In other bariatric teams, when telehealth platforms were unavailable, phone calls were used to conduct follow-up clinic work, and 81.7% of the patients stated they were satisfied [33].
Three patients (3.7%) in our study population switched to TC during the preoperative bariatric assessment and were operated when surgical rooms were reopened for non-emergency care, and all 3 are still in active follow-up. Mills et al. recently reported completely virtualized multidisciplinary preoperative management during the pandemic without negative impact on preoperative workup in comparison with conventional management [34]. Several observational studies [17] have shown that TM integrated into preoperative bariatric programs improved overall patient satisfaction, connection with the multidisciplinary team, and perceptions regarding their knowledge of nutrition a healthier lifestyle. Recently, a study conducted before the pandemic investigated the influence of intensive nutritional and lifestyle support by phone during the perioperative period and found greater weight loss at one and 3 years following surgery in patients included in this protocol compared to those who were not [22]. During the lockdowns, patients with overweight or obesity (N = 1550) included in a national weight-loss program who underwent remote consultation follow-up with dieticians from 2 to 6 months post-surgery showed greater weight loss compared to those who did not benefit from remote clinic support (− 4.4 kg vs − 1.4 kg; p < 0.01). The study found that number of remote clinics was positively correlated with extent of weight loss [18]. Taken together, these outcomes argue for the use of bariatric tele-care from as early as the preoperative assessment, providing that patients are comfortable with using the virtual tool.
Only one patient was lost to follow-up at 6 months, and only five (6.4%) of the eligible patients were lost to follow-up at 2 years post-TC implementation and four beyond 2 years post-BS. TC was found to be associated with stronger adherence to weight-loss programs [17], but little data is available on the impact of TC on adherence to bariatric follow-up. Even though our study population had a limited sample size for investigating the effect of TC, the rate recorded here seems low in comparison with data from the literature. Indeed, an earlier audit from our prospective cohort showed 75% and 46% follow-up rates in face-to-face clinics at 2 and 5 years post-BS [35], respectively. Similar results were reported by Paolino et al. who found 92.6% and 44.3% follow-up rates at 2 and 5 years post-surgery [36], with sleeve gastrectomy, male gender, and geographical distance identified as significant risk factors for discontinuation of follow-up [37]. Here, 96.7% of the population who answered the questionnaire found TC to save time, and 76.1% found it helped remove geographical barriers to healthcare structures. These benefits can partially explain the high follow-up rate reported in this cohort. The link between adherence to follow-up and weight loss remains a subject of debate [38], but some teams have nevertheless underlined a relationship between regular follow-up and favorable weight-loss outcomes at 5 years [36, 39]. With that in mind, a recent report by the French Ministry for Health [40] pointed out the need to improve bariatric follow-up and identified TM as a potentially valuable tool for that purpose.
During the COVID-19 lockdown, decreased physical activity, unhealthy eating behaviors, and increased stress resulted in significant weight gain in adults [41, 42] and children [43]. However, these findings were mostly based on self-reported data, which limits the reliability of these studies [44]. Here, we did not investigate weight-loss outcomes in our study population, due to these pandemic-related variables and the heterogeneity of the bariatric patient population and postoperative timeframes. Interestingly, we observed that due to inter-current health issues, TC rate decreased to 69.2% at 1 year but increased to 100% of eligible study-population patients at 2 years following implementation, which shows that patients are flexible and interested in new follow-up technologies.
Overall, all the bariatricians and 80% of the patients were satisfied with TC at 2 years after implementation and expressed their wish to maintain virtual bariatric follow-up appointments. However, thorough patient satisfaction analysis showed that 33% of patients would prefer to go back to FTFC, and 34% felt unsecure with remotely tackling any health issues that may arise. These data can be explained by the limited rate of satisfaction with the interface rather than any objective misdiagnosed complications. Our findings argue for a follow-up that alternates TC with FTFC in certain patients. TM has been shown to be feasible in various surgical settings [27] including BS [20] during and after lockdown, as confirmed here. With the pandemic now in decline, FTFC have progressively resumed [27], thus allowing the patients to reconnect in-person with their bariatricians. As suggested by Kapadia et al. [45], these contrasted satisfaction outcomes can be explained by the need to restore a patient-practitioner alliance, based on an effective relationship and verbal as well as non-verbal communication [28, 46, 47], which may be suboptimal through TM platforms and could unintentionally lead to communication breakdown and loss to follow-up. Better quality of communication and a better TM experience could help improve patient satisfaction and adherence to TM. These aspects should be investigated further to support optimal use of TM in bariatric medicine and beyond.
Finally, as reported by Hardy et al. [33], most of the patients found TC to be on a par with FTFC in terms of saving time and costs, probably because they did not have to stop working and/or travel to attend the clinic. These outcomes highlight the potential economic benefits of implementing TC in bariatric follow-up. A study looking at the long-term management of chronic diseases such as diabetes [48] found that using TM for retinal complications, telemonitoring, and remote assistance was cost-effective, but there is still little data available on the cost-effectiveness of TM in the management of obesity and BS.
This present pilot study carries several limitations inherent to its retrospective and declarative nature. The Likert scale is a validated tool for measuring different attitudes and satisfaction levels. However, there is currently no validated tool to specifically address the effects of TC in our study population. Therefore, in line with what other teams have done [19, 33], we developed a dedicated questionnaire using the Likert method to estimate patient/practitioner experiences and satisfaction with bariatric TC. As discussed above, we did not investigate the cost-effectiveness of this TC implementation program and weight-loss outcomes. Large-scale randomized multicentric studies are now needed to determine whether TC is comparable to FTFC in the management of bariatric patients in order to gain further knowledge and endorse safe and widespread use of TM in this frail population.
Conclusion
Bariatric follow-up with TC was found to apply to more than 90% of our patients. TC emerged as a satisfactory substitute to FTFC without compromising patient safety during and beyond the pandemic. Although TC first emerged as a fantastic opportunity to maintain the link with our patients, the underwhelming patient satisfaction outcomes at 2 years point to a need to discuss follow-up preferences with the patients in order to help maintain adherence to the alliance with the multidisciplinary team and avoid lost-to-follow-up. Further research is needed to provide evidence on the long-term benefit of TM in order to facilitate resource allocation to expand TM use and uptake for high-quality follow-up in bariatric patients.
Change history
26 April 2023
A Correction to this paper has been published: https://doi.org/10.1007/s11695-023-06612-4
References
Bhaskaran K, Dos-Santos-Silva I, Leon DA, et al. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol. 2018;6:944–53.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387:1513–30.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from. to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 1975;2017(390):2627–42.
Salminen P, Grönroos S, Helmiö M, et al. Effect of laparoscopic sleeve gastrectomy vs Roux-en-Y gastric bypass on weight loss, comorbidities, and reflux at 10 years in adult patients with obesity: the SLEEVEPASS randomized clinical trial. JAMA Surg. 2022;157(8):656–666. https://doi.org/10.1001/jamasurg.2022.2229.
Syn NL, Cummings DE, Wang LZ, et al. Association of metabolic-bariatric surgery with long-term survival in adults with and without diabetes: a one-stage meta-analysis of matched cohort and prospective controlled studies with 174 772 participants. Lancet. 2021;397:1830–41.
Kwok S, Adam S, Ho JH, et al. Obesity: a critical risk factor in the COVID-19 pandemic. Clin Obes. 2020;10:e12403.
Simonnet A, Chetboun M, Poissy J, et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity (Silver Spring). 2020;28(7):1195–1199. https://doi.org/10.1002/oby.22831.
Aminian A, Safari S, Razeghian-Jahromi A, et al. COVID-19 outbreak and surgical practice: unexpected fatality in perioperative period. Ann Surg. 2020;272:e27–9.
COVIDSurg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396:27–38.
COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107:1440–9.
Singhal R, Tahrani AA, Sakran N, et al. Effect of COVID-19 pandemic on global bariatric surgery practices - the COBRAS study. Obes Res Clin Pract. 2021;15:395–401.
Réponses rapides dans le cadre du COVID-19 -Téléconsultation et télésoin [Internet]. Haute Autorité de Santé. [cited 2020 Apr 18]. Available from: https://www.has-sante.fr/jcms/p_3168867/fr/reponses-rapides-dans-le-cadre-du-covid-19-teleconsultation-et-telesoin
Executive Council of ASMBS. Safer through surgery: American Society for Metabolic and Bariatric Surgery statement regarding metabolic and bariatric surgery during the COVID-19 pandemic. Surg Obes Relat Dis. 2020;16:981–2.
Pouwels S, Omar I, Aggarwal S, et al. The first modified Delphi consensus statement for resuming bariatric and metabolic surgery in the COVID-19 Times. Obes Surg. 2021;31:451–6.
COVIDSurg Collaborative. Global guidance for surgical care during the COVID-19 pandemic. Br J Surg. 2020;107:1097–103.
Kassir R, Rebibo L, Genser L, et al. SOFFCO-MM guidelines for the resumption of bariatric and metabolic surgery during and after the Covid-19 pandemic. J Visc Surg. 2020;157:317–27.
Coldebella B, Armfield NR, Bambling M, et al. The use of telemedicine for delivering healthcare to bariatric surgery patients: a literature review. J Telemed Telecare. 2018;24:651–60.
Bailly S, Fabre O, Legrand R, et al. The impact of the COVID-19 lockdown on weight loss and body composition in subjects with overweight and obesity participating in a nationwide weight-loss program: impact of a remote consultation follow-up-the CO-RNPC study. Nutrients. 2021;13:2152.
Runfola M, Fantola G, Pintus S, et al. Telemedicine Implementation on a bariatric outpatient clinic during COVID-19 pandemic in Italy: an unexpected hill-start. Obes Surg. 2020;30:5145–9.
Brown AM, Ardila-Gatas J, Yuan V, et al. The impact of telemedicine adoption on a multidisciplinary bariatric surgery practice during the COVID-19 pandemic. Ann Surg. 2020;272:e306–10.
Hincapié MA, Gallego JC, Gempeler A, et al. Implementation and usefulness of telemedicine during the COVID-19 pandemic: a scoping review. J Prim Care Community Health. 2020;11:2150132720980612.
Koffman L, Levis AW, Haneuse S, et al. Evaluation of intensive telephonic nutritional and lifestyle counseling to enhance outcomes of bariatric surgery. Obes Surg. 2022;32:133–41.
Haute Autorité de Santé - Obésité : prise en charge chirurgicale chez l’adulte [Internet]. [cited 2015 Jul 17]. Available from: http://www.has-sante.fr/portail/jcms/c_765529/fr/obesite-prise-en-charge-chirurgicale-chez-l-adulte
Coronavirus disease (COVID-19) – World Health Organization [Internet]. [cited 2022 Jun 23]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019
Dorsey ER, Topol EJ. Telemedicine 2020 and the next decade. Lancet. 2020;395:859.
Moazzami B, Razavi-Khorasani N, Dooghaie Moghadam A, et al. COVID-19 and telemedicine: immediate action required for maintaining healthcare providers well-being. J Clin Virol. 2020;126:104345.
Chao GF, Li KY, Zhu Z, et al. Use of telehealth by surgical specialties during the COVID-19 pandemic. JAMA Surg. 2021;156:620–6.
Télémédecine – La téléconsultation et la téléexpertise en pratique [Internet]. Haute Autorité de Santé. [cited 2021 Feb 27]. Available from: https://www.has-sante.fr/jcms/p_3069228/fr/telemedecine-la-teleconsultation-et-la-teleexpertise-en-pratique
Alamri AA, Alsadiqi AI, Dahlawi A, et al. Are patients aware of potential risks of weight reduction surgery? An internet based survey. Saudi J Gastroenterol. 2019;25:97–100.
Meleo-Erwin ZC, Basch CH, Fera J, et al. Discussion of weight loss surgery in Instagram posts: successive sampling study. JMIR Perioper Med. 2021;4:e29390.
Paolino L, Genser L, Fritsch S, et al. The web-surfing bariatric patient: the role of the internet in the decision-making process. Obes Surg. 2015;25:738–43.
Lazzati A, Chatellier G, Paolino L, et al. Postoperative care fragmentation in bariatric surgery and risk of mortality: a nationwide study. Surg Obes Relat Dis. 2021;17:1327–33.
Hardy K, Anistratov A, He W, et al. Bariatric patient experience with virtual care during the COVID-19 pandemic. Obes Surg. 2022;32:940–3.
Mills J, Liebert C, Pratt J, et al. Complete telehealth for multidisciplinary preoperative workup does not delay time to metabolic and bariatric surgery: a pilot study. OBES SURG [Internet]. 2022 [cited 2022 Sep 18]; Available from:https://doi.org/10.1007/s11695-022-06233-3.
Vignot M, Oppert J-M, Basdevant A, et al. Adhésion au suivi après chirurgie bariatrique : identification des facteurs de non observance dans une cohorte de 207 patients obèses sévères opérés. Évaluation de l’adhésion du patient obèse sévère au suivi post chirurgie bariatrique. Recherche en soins infirmiers. 2018;N° 134:70–7.
Luca P, Nicolas C, Marina V, et al. Where are my patients? Lost and Found in Bariatric Surgery. Obes Surg. 2021;31(5):1979–1985. https://doi.org/10.1007/s11695-020-05186-9.
Spaniolas K, Kasten KR, Celio A, et al. Postoperative follow-up after bariatric surgery: effect on weight loss. Obes Surg. 2016;26:900–3.
Is adherence to follow-up after bariatric surgery necessary? A systematic review and meta-analysis - PubMed [Internet]. [cited 2022 Aug 24]. Available from: https://pubmed.ncbi.nlm.nih.gov/35020125/
Lujan J, Tuero C, Landecho MF, et al. Impact of routine and long-term follow-up on weight loss after bariatric surgery. Obes Surg. 2020;30:4293–9.
Situation de la chirurgie de l’obésité - IGAS - Inspection générale des affaires sociales [Internet]. [cited 2018 Nov 26]. Available from: http://www.igas.gouv.fr/spip.php?article704
Bellicha A, Lassen PB, Poitou C, et al. Effect of COVID-19 lockdowns on physical activity, eating behavior, body weight and psychological outcomes in a post-bariatric cohort. Obes Surg. 2022;32(7):1–9. https://doi.org/10.1007/s11695-022-06069-x.
Zeigler Z. COVID-19 self-quarantine and weight gain risk factors in adults. Curr Obes Rep. 2021;10:423–33.
Jebeile H, Kelly AS, O’Malley G, et al. Obesity in children and adolescents: epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. 2022;10:351–65.
Pearl RL, Schulte EM. Weight bias during the COVID-19 pandemic. Curr Obes Rep. 2021;10:181–90.
Kapadia MR, Kratzke IM, Sugg SL. The rise and fall of surgical telehealth—can lack of patient connection be blamed? JAMA Surg. 2021;156:627.
Télémédecine [Internet]. [cited 2020 Jan 19]. Available from: https://esante.gouv.fr/projets-nationaux/telemedecine
Sabesan S, Allen D, Caldwell P, et al. Practical aspects of telehealth: doctor-patient relationship and communication. Intern Med J. 2014;44:101–3.
Lee JY, Lee SWH. Telemedicine cost-effectiveness for diabetes management: a systematic review. Diabetes Technol Ther. 2018;20:492–500.
Acknowledgements
We thank Nathalie Nunes, Linda Helbert, and Virginie Bourgain for their help in data Collection and in telemedicine implementation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ahmed Daouadji-Ghazouani and Judith Aron-Wisnewsky are co-first authors.
Key Points
• TC was applicable to 92% of this cohort.
• There were no readmissions at 30 and 90 days after TC.
• At 2 years post-implementation, follow-up rate was 93.5% (TC: 100%), and satisfaction rate was 80%.
• Thirty-three percent of patients would prefer to go back to FTFC.
• Underwhelming satisfaction outcomes at 2 years highlight the need to talk over follow-up preferences in order to achieve optimal outcomes.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Daouadji-Ghazouani, A., Aron-Wisnewsky, J., Torcivia, A. et al. Follow-Up, Safety, and Satisfaction with Tele-bariatric Follow-Up Implemented During the COVID-19 French Lockdown: a 2-Year Follow-Up Study. OBES SURG 33, 1083–1091 (2023). https://doi.org/10.1007/s11695-023-06485-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06485-7