Abstract
Background
Endoscopic bariatric therapies (EBT) has emerged as an effective treatment in the management of the patient with obesity. Unfortunately, most procedures involve only the restriction of gastric volume without altering the underlying metabolism. The objective of this study was to investigate the practicability and limitations of the metabolic altering procedures: “One anastomosis gastric bypass (OAGB)” with “natural orifice transluminal endoscopic surgery (NOTES)” on human cadavers.
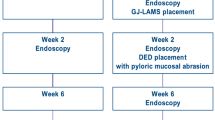
Methods
We performed OAGB with NOTES approach in 3 human cadavers. The steps of the procedure can be divided as follows: step 1, endoscopic sleeve gastroplasty (ESG); step 2, trans-gastric access to peritoneal cavity; step 3, identification of suitable loop of jejunum; step 4, introduction of the jejunal loop into the stomach; step 5, creation of the gastro-jejunostomy with lumen-apposing metal stent (LAMS); step 6, gastric pylorus occlusion with overstitch.
Results
We performed OAGB with NOTES in 3 human cadavers with bypassed bilio-pancreatic limb of 55, 75, and 105 cm from the pylorus. The average weight for the cadavers was 64.9 kg (61.2–71.7 kg). The mean procedure time was 157 min. The optimal bypassed length for the procedure was 105 cm.
Conclusions
This study has provided proof-of-principle in a pre-clinical cadaveric model that NOTES approach can be used to perform OAGB and, therefore, merits additional evaluation and consideration in surviving porcine model.
Graphical abstract









Similar content being viewed by others
References
Asian Diabetes Prevention Initiative: Facts and Figures. http://www.idf.org/diabetesatlas. Accessed 23 Mar 2022
ASMBS. Estimate of bariatric surgery numbers 2011–2017 Gainesville, FL; 2018. https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers. Accessed 29 May 2022
Swanstorm LL, Volckmann E, Hungness E, et al. Patient attitudes and expectations regarding natural orifice transluminal endoscopic surgery. Surg Endosc. 2009;23(7):1519–25.
Dayyeh BKA, Bazerbachi F, Vargas EJ, et al. Endoscopic sleeve gastreoplasty for treatment of class 1 and 2 obesity (MERIT): a prospective, multicenter, randomized trial. Lancet. 2022;400(10350):441–51.
Lim CH, Lee ZJ, Yeung B, et al. Natural orifice transluminal endoscopic one-anastomosis gastric bypass: a feasibility study using porcine model. Surg Endo. 2021. https://doi.org/10.1007/s00464-021-08547-2.
Rutledge R, Walsh TR. Continued excellent results with the mini-gastric bypass six-year study in 2,410 patients. Obes Surg. 2005;15(9):1304–8.
Lee WJ, Yu PJ, Wang W, et al. Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment of morbid obesity. Ann Surg. 2005;242(1):20–8.
Lee WJ, Chong K, Ser KH, et al. Gastric bypass vs sleeve gastrectomy for type 2 diabetes mellitus: a randomized controlled trial. Arch Surg. 2011;146(2):143–8.
Hagen ME, Wagner OJ, Swain P, et al. Hybrid natural orifice transluminal endoscopic surgery (NOTES) for Roux-en-Y gastric bypass: an experimental surgical study in human cadavers. Endoscopy. 2008;40(11):918–24.
Madan AK, Tichansky DS, Khan KA, et al. Natural orifice transluminal endoscopic gastric bypass performed in cadaver. Obes Surg. 2008;18(9):1192–9.
Chang JHE, Tan D, Chan WH, et al. Endoscopic partial reversal of complicated single anastomosis gastric bypass. Endoscopy 2019;51(5)
Lim CH, Amateur SK, McDonald NM, et al. EUS-guided endoscopic gastrointestinal anastomosis with lumen-apposing metal stent: feasibility, safety, and efficacy. Obes Surg 2018;28(5)
Lim CH, Ikramuddin S, Leslie DB, et al. Novel endoscopic management of a pancreatico-biliary limb obstruction by the creation of an entero-enterostomy following Roux-en-Y gastric bypass. Endoscopy. 2016;48(01):99–100.
Machytka E, Bužga M, Zonca P, et al. Partial jejunal diversion using an incisionless magnetic anastomosis system: 1-year interim results in patients with obesity and diabetes. Gastrointest Endosc. 2017;86(5):904–12.
GL Nava, RT Arau, R Asokkumar, et al. Prospective multicenter study of the primary obesity surgery endoluminal (POSE 2.0) procedure for treatment of obesity. Clin Gastroenterol Hepatol 2022;S1542–3565(22)00444-X. https://doi.org/10.1016/j.cgh.2022.04.019
Gonzalez JM, Ouazzani S, Monino L, et al. First fully endoscopic metabolic procedure with NOTES gastrojejunostomy, controlled bypass length and duodenal exclusion: a 9-month porcine study. Sci Rep. 2022;12:21. https://doi.org/10.1038/s41598-021-02921-9.
Pizza F, Lucido FS, D’Antonio D, et al. Biliopancreatic limb length in one anastomosis gastric bypass: which is the best? Obes Surg. 2020;30(10):3685–94.
Moreno C, Closset J, Dugardeyn S, et al. Transoral gastroplasty is safe, feasible, and induces significant weight loss in morbidly obese patients: results of the second human pilot study. Endoscopy. 2008;40(5):406–13.
Familiari P, Costamagna G, Bléro D, et al. Transoral gastroplasty for morbid obesity: a multicenter trial with a 1-year outcome. Gastrointest Endosc. 2011;74(6):1248–58.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
IRB approval and written consent is not required for cadaver study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Many patients perceive bariatric-metabolic surgery as dangerous and believe that living with severe obesity is safer than undergoing surgery.
• Endoscopic bariatric therapies (EBT) using flexible gastrointestinal endoscopy have emerged as a reliable alternative to traditional laparoscopic approach.
• We performed OAGB with NOTES in 3 human cadavers and the optimal bypassed length for the procedure was 105 cm.
• The twinning of a highly effective OAGB in weight loss and metabolic syndrome resolution, combined with “incision-less” surgery, will present a more acceptable option for this disease.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (Video 135 MB)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lim, C.H., Lee, Z.J., Lye, T. et al. Natural Orifice Transluminal Endoscopic One-Anastomosis Gastric Bypass: a Feasibility Study Using Human Cadavers. OBES SURG 32, 3787–3795 (2022). https://doi.org/10.1007/s11695-022-06273-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06273-9