Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic led to a worldwide suspension of bariatric and metabolic surgery (BMS) services. The current study analyses data on patterns of service delivery, recovery of practices, and protective measures taken during the COVID-19 pandemic by bariatric teams.
Materials and Methods
The current study is a subset analysis of the GENEVA study which was an international cohort study between 01/05/2020 and 31/10/2020. Data were specifically analysed regarding the timing of BMS suspension, patterns of service recovery, and precautionary measures deployed.
Results
A total of 527 surgeons from 439 hospitals in 64 countries submitted data regarding their practices and handling of the pandemic. Smaller hospitals (with less than 200 beds) were able to restart BMS programmes more rapidly (time to BMS restart 60.8 ± 38.9 days) than larger institutions (over 2000 beds) (81.3 ± 30.5 days) (p = 0.032). There was a significant difference in the time interval between cessation/reduction and restart of bariatric services between government-funded practices (97.1 ± 76.2 days), combination practices (84.4 ± 47.9 days), and private practices (58.5 ± 38.3 days) (p < 0.001).
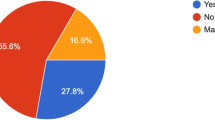
Precautionary measures adopted included patient segregation, utilisation of personal protective equipment, and preoperative testing. Following service recovery, 40% of the surgeons operated with a reduced capacity. Twenty-two percent gave priority to long waiters, 15.4% gave priority to uncontrolled diabetics, and 7.6% prioritised patients requiring organ transplantation.
Conclusion
This study provides global, real-world data regarding the recovery of BMS services following the COVID-19 pandemic.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The COVID-19 pandemic has had a devastating impact on healthcare services worldwide. During the early stages of the pandemic, the majority of elective surgical services needed to be paused [1]. There was evidence that recent infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) would significantly increase risks associated with surgery [2]. With regards to bariatric and metabolic surgery (BMS), the International Federation for the Surgery of Obesity and Metabolic Disorder recommended all non-emergency bariatric surgery be suspended during the initial phase of the COVID-19 pandemic [3]. Studies confirm that BMS services were almost entirely paused during this phase of the pandemic [4, 5].
The COVID-19 pandemic arrived on top of a worsening obesity pandemic [6]. Patients with obesity are at increased risk of developing severe COVID-19-related disease, and the COVID-19 pandemic has had a further adverse impact on obesity rates due to the repeated periods of ‘lockdown’ and disruption to both medical and surgical weight management services worldwide along with changes in lifestyle leading to less physical activity and more calorie consumption [7, 8].
With the development of vaccines and improved medical therapeutics for COVID-19, we may have put the worst of the pandemic behind us but the critical question at this stage is what lessons can be learnt from the international response to the COVID-19 pandemic and how this may influence the strategic response to recovery of BMS services, further COVID-19 waves, or other global pandemics. Concerning BMS this should have a particular focus on how it will be possible to maintain services or recover swiftly in such eventualities.
The current study has utilised hospital-level data collected as part of the GENEVA study [9,10,11] to analyse patterns of service delivery, recovery of practices, and protective measures taken during the COVID-19 pandemic. The aim was to identify the strategies deployed during the recovery of BMS services following COVID-19.
Methods
The current study is a subset analysis of the GENEVA study. The GENEVA study was a global, multicentre, observational study of BMS (elective primary, elective revisional, and emergency) performed between 1/05/2020 and 31/10/2020 in the adult (≥ 18 years). Detailed methods have been published previously [9, 10]. This study was registered as a multinational audit at the host institution [blinded] with registration number 5197. The hospital-level data collected detailed and anonymised information about surgeons, their respective bariatric surgical centres, the effect and handling of the pandemic at their centres, local perioperative COVID-19 safety protocols, and the timelines for the pandemic in their respective hospitals along with the chronology of the hospital response. Data for time points were collected to understand how different practices handled the pandemic. These time points included the first case diagnosed in the city, the first case admitted to the hospital, the peak in hospital admissions, stoppage, and subsequent restart of services. Only practices with all valid time points were considered for this part of the analysis. Data on these aspects were captured from participating surgeons through 28 questions (Appendix 1).
Statistical Analysis
Continuous data were expressed as mean with standard deviation (SD). Data distribution was tested using the Kolmogorov–Smirnov test. Categorical data were presented as a number with percentages where appropriate. Patient characteristics and outcomes were compared using a Mann–Whitney U-test for continuous variables and a chi-square test for categorical variables.
A comparison of means was performed using the Kruskal–Wallis test. For these models, only cases with a complete data set were used. All tests were two-sided, and a p-value < 0.05 was considered statistically significant. All data were analysed using a statistical software package (SPSS™ Inc., version 24, Chicago, IL, USA).
For Figs. 1, 2, and 3, data were analysed and plotted in python 3.9 with in-house written python scripts using numpy (version 1.20.2), scipy (version 1.6.2), matplotlib (version 3.4.1), cartopy (version 0.18.0), and pandas (version 1.2.4). For Figs. 2 and 3, data were accumulated for each day data was reported, on. For clarity, all data was then fed through a low-pass Butterworth filter and the maximum of the data was added to the resulting curve. The smoothed data was then plotted as connected line segments.
Results
A total of 527 surgeons from 439 hospitals in 64 countries submitted data on their practices and handling of the pandemic. Figure 1 gives an overview of the geographical distribution of hospitals included in this study. Table 1 shows the baseline data of the participating surgeons and centres.
Complete data with regards to all-time points were available for 276 unique practices. Only this data was used when analysing the effect of hospital volume or type of bariatric practice over handling the COVID-19 pandemic. All data was found to be not normally distributed.
Effect of Type of Bariatric Practice/Hospital Volume and Handling of the COVID-19 Pandemic
Figure 2 shows the timeline of the first case diagnosed in the city, the first case admitted to the primary hospital, and the peak number of hospital admissions according to the practice type. The majority of the practices reported that the first patient with COVID-19 in their city was diagnosed in the second week of March 2020, and the first patient with COVID-19 was admitted to their primary hospital in the same week. Two peaks in hospital admissions were noticed. The first peak was between 09/03/2020 and 12/05/2020 in 192 out of 276 (70%) practices. The second peak was between 12/05/2020 and 06/07/2020 in 69 out of 276 (25%) practices. Figure 3 shows the same data stratified according to the hospital volume (data for hospitals with 1000–2000 beds and more than > 2000 beds was combined due to the limited number of hospitals within these groups.
When comparing privately funded practices with government-funded or combination practices, there was relative shielding of the private practices, with only 49 out of 109 (45%) having a peak in hospital admissions at a similar time when government and combination practices had a peak (09/03/20–04/05/20; peak incidence–13/04/2020; Fig. 2). This was followed by a second peak mainly in the private practices in May/ June (11/05/2020–22/06/2020). This was seen for 50 out of 109 (46%) of the private practices.
Of 276 practices (43.1%), 119 noticed a change in their bariatric practice before the first case was diagnosed in that city. Hospitals stopped their bariatric activity at a mean of 5 days (± 27.96) before the first case of COVID-19 was diagnosed in the city. Bariatric activity in private and combination practices stopped earlier than in government-funded practices (7.11 ± 29.22 and 7.16 ± 32.01 vs 1.39 ± 17.80 days) before the first case of COVID-19 was diagnosed in the city.
Hospitals with a bed volume of < 200 beds had two distinct peaks of hospital admissions as opposed to hospitals with 200–500 beds, 500–1000 beds, or > 1000 beds. The first peak was reported between 09/03/20 and 04/05/20 with a peak incidence on 14/04/20, followed by a second peak between 11/05/20 and 22/06/20 with a peak incidence on 01/06/20 (Fig. 4). Thirty four of 72 (47%) practices with less than 200 beds reported a peak in hospital admissions during the first peak whilst 31 of 72 practices (44%) reported a peak during the second peak. Overall, the second peak in hospital admissions was less pronounced for larger hospitals. For hospitals with 200–500 beds, the second peak was noticed for 26 of 102 (25%) practices, followed by 15 of 70 (21%) for 500–1000 bedded hospitals and 10 of 32 (31%) for hospitals with > 1000 beds.
Factors Affecting the Resumption of Bariatric Services
Figure 4 depicts a timeline of the changes in bariatric activity due to the COVID-19 pandemic and when hospitals resumed bariatric surgical practice. Out of 276 practices (90%), 248 reported changes in their bariatric practices between 23/02/20 and 06/04/20. Peaks in the resumption of elective bariatric surgery were seen between 20/04/20 and 27/7/2020 in 237 out of 276 practices (86%).
There was a significant difference in the time interval between the stoppage/reduction and restart of bariatric services between government-funded practices (97.1 ± 76.2 days), combination practices (84.4 ± 47.9 days), and private practices (58.5 ± 38.3 days) (p < 0.001; Kruskal–Wallis test). The time interval was significantly shorter in the private practices.
The resumption of services was again significantly in favour of smaller hospitals: 60.8 ± 38.9 days (< 200 beds) versus 76.8 ± 44.0 days (200–500 beds), 94.3 ± 80.3 days (500–1000 beds), 79.6 ± 51.8 days (1000–2000 beds), and 81.3 ± 30.5 days (> 2000 beds) (p-value = 0.032, Kruskal–Wallis test).
Precautionary Measures
With regards to the management of patient flow, 266 (50.5%) surgeons reported that they had separate wards for elective and severe acute respiratory syndrome–coronavirus 2 (SARS-CoV-2)-positive patients, and 103 (19.5%) indicated that patients who tested positive were moved to separate sites. Thus overall, almost two thirds of the surgeons maintained segregation of elective and COVID-19 patients.
Regarding preoperative testing, 359 (68.1%) surgeons confirmed that patients had at least one preoperative Reverse Transcriptase–Polymerase Chain Reaction Test (RT-PCR) for SARS-CoV-2 infection. Similarly, a preoperative chest X-ray or Computed Tomography (CT) scan was advised by 148 (28.1%) and 108 (20.5%) surgeons, respectively. Preoperative self-isolation was advised by 269 (49.1%) of the surgeons.
The most popular precautionary measure amongst healthcare staff was wearing masks and self-recording of temperature and symptoms (Table 2). Staff members, nurses, surgeons, and non-clinical staff in 434 (82.4%), 435 (82.5%), and 393 (74.6%) of the cases, respectively, were advised to wear masks. Of the nurses, surgeons, and non-clinical staff, respectively, 338 (64.1%), 323 (61.3%), and 393 (56.4%) were advised to monitor their temperature and symptoms.
Of the surgeons, 270 (51.2%) reported that Personal Protection Equipment (PPE) kits were immediately available, and 81 (15.4%) said there was a delay in availability varying between 0 and 30 days after the publication of the guidelines of the World Health Organisation (WHO).
Impact of COVID-19 Pandemic on Bariatric Practice
Four-hundred forty-eight out of 527 (85%) surgeons reported that the COVID-19 pandemic had decreased their elective bariatric surgical practice. Six (1.1%) surgeons had an increase in elective bariatric surgical practice, and 5 (0.9%) had no change. In five of the six cases where surgeons reported an increase in elective bariatric surgical practice, the increase was attributed to the patients seeking weight loss for protection from COVID-19. One of the six was due to the re-allocation of elective surgery to the so-called COVID-19-free hospital. Four-hundred (75.9%) surgeons reported that elective bariatric surgical practice ceased completely at some time point.
Around 40% of the surgeons operated with a reduced capacity, 22% gave priority to long waiters, 15.4% gave priority to uncontrolled diabetics, and 7.6% prioritised patients requiring organ transplantation (Table 3). Only a minority continued without any restrictions.
Discussion
The present study has provided real-world data regarding the process of recovery of BMS services following the COVID-19 pandemic. The study demonstrates that the majority of hospitals stopped BMS operations before the first patient was diagnosed with COVID-19 in that geographical area and that this suspension of services occurred more swiftly in privately funded units than in government institutions.
This study found that smaller hospitals (with less than 200 beds) were able to restart BMS services more rapidly (time to BMS restart 60.8 ± 38.9 days) than larger institutions (over 2000 beds) (81.3 ± 30.5 days) (p = 0.032). The reasons for this are likely to be multifactorial. These hospitals may have been less severely affected during the initial COVID-19 wave. Larger hospitals may also have had a greater burden of critically unwell patients requiring more specialist services. These patients are likely to have had more prolonged admissions during their COVID-19 treatment [12].
Another critical aspect of elective surgery recovery following COVID-19 has been the necessity to segregate patients on elective ‘green’ pathways where patients are specifically screened before admission to prevent the transmission of COVID-19. In many instances, this has been achieved through the utilisation of separate hospital sites for elective patients. This was also identified in the current study with the majority of surgeons utilising some form of patient segregation and almost 20% treating elective patients on a separate hospital site where COVID-19 patients were being managed. This development of separate hospital sites for elective surgery may also provide a further potential explanation of the finding that smaller units were able to resume BMS at earlier stages as these may have been selected as the potential green site for these services. It is to be noted that these green pathways in this study were formulated between May and October 2020, before their value became more widely reported [13].
BMS patients generally do not require a large number of intensive care or high-dependency unit beds compared to other specialities such as cancer or transplant surgery [14]. The majority of specialist equipment (such as laparoscopic equipment, appropriate operating tables, and ward-based patient care items) are potentially transferable between hospital sites. This makes BMS a very adaptable surgical specialty that can be relatively self-contained and is well suited to be transferred to an alternative hospital site as and when necessary.
A further significant finding in this dataset was that privately funded institutions were able to resume BMS services more swiftly than government institutions. Again, the reasons for this are likely to be multifactorial and may vary globally. Many private institutions were also smaller (just under half of the private hospitals had less than 200 beds) and may have been influenced by the factors described above. Furthermore, in many healthcare systems such privately funded hospitals would not have been treating large numbers of COVID-19 patients. During the recovery phase many countries saw close collaboration between private providers and government institutions. In some areas, these private units were specifically utilised as the ‘green’ sites described above to treat publicly funded patients that would otherwise have been treated in government institutions [15, 16]. This form of collaboration allowed for elective surgery to resume much more rapidly in many areas than relying upon government institutions alone.
During the recovery phase of the COVID-19 pandemic, many surgeons were required to prioritise patients to facilitate the appropriate resource utilisation. Many surgeons in the present study (40%) reported that they were operating with reduced capacity compared to the pre-pandemic level. There was some variation in priority groups with some units focussing on long-waiting patients (22.0%), whilst a smaller number prioritised those with uncontrolled diabetes (15.4%) or those awaiting organ transplant (7.6%). This is interesting and seems to be at odds with the guidance provided during the early stages of the pandemic [4, 17].
Aside from the direct effect on surgical services, the COVID-19 pandemic has seen the need for widespread lockdown restrictions which have had a profound negative effect on multiple aspects of health-related behaviours such as eating habits and physical activity, and other barriers to weight management [18]. There were also major changes concerning how the whole range of weight management services was delivered including access to services and the increased use of telemedicine for care delivery [19]. These changes were welcomed by patients and can improve efficiency for healthcare professionals, and are therefore likely to become part of the long-term care model for future weight management services [20]. Such adaptations of services are likely to be maintained even after the pandemic. However, data regarding the effectiveness of such strategies have been controversial [21], although the majority of studies have demonstrated effective results following BMS during the COVID-19 pandemic [22, 23].
Although the present study has provided an overview of the effect of the initial stages COVID-19 pandemic on BMS services the period of data collection ended in October 2020. As the COVID-19 pandemic has continued to progress it has to date been unclear how this has influenced the delivery of BMS services in 2021 and 2022. Data recently published from the National Obesity Audit in England have demonstrated that although the number of cases performed between April 2021 and April 2022 (n = 4440) has improved compared to 2020/2021 (n = 1854) this has still not reached pre-pandemic rates of BMS (2018/2019, n = 6779) [24]. Data from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Programme (MBSAQIP) in the United States has also confirmed a reduction in BMS during 2020 of approximately 22.5% [25], but data regarding the recovery of services in 2021 and beyond is awaited. In the future, it will also be necessary to establish if there has been any increase in referrals for BMS which may have been triggered due to concerns regarding the effect of severe obesity on outcomes following SARS-CoV-2 infection [26, 27].
Significant strengths of the present study are that it provides large-scale real-world data on the recovery of BMS services during the COVID-19 pandemic globally. Despite this, several important limitations must be considered when interpreting these results. Data were self-reported and not externally validated, therefore is reliant upon the accuracy of data input by individual collaborators. Due to the global nature of this study, there was significant variation in healthcare structure across participating centres (particularly the relationship between government and privately funded institutions). Data regarding screening and precautionary measures for COVID-19 was collected before the widespread introduction of rapid lateral flow tests for this purpose, and therefore data regarding their utilisation was not collected. The present study was also conceived and executed before the widespread utilisation of vaccination against SARS-CoV-2 for the general population so it has not been possible to assess the influence of the vaccination programme on BMS.
Conclusion
The present study has provided global, real-world data regarding the recovery of BMS services during the COVID-19 pandemic.
Data Availability
The data used to support the findings of this study can be released upon request.
References
COVIDSurg. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107(11):1440–9.
Collaborative C, Collaborative G. Timing of surgery following SARS-CoV-2 infection: an international prospective cohort study. Anaesthesia. 2021;76(6):748–58.
Yang W, Wang C, Shikora S, et al. Recommendations for metabolic and bariatric surgery during the COVID-19 pandemic from IFSO. Obes Surg. 2020;30(6):2071–3.
Singhal R, Tahrani AA, Sakran N, et al. Effect of COVID-19 pandemic on global Bariatric surgery PRActiceS — the COBRAS study. Obes Res Clin Pract. 2021;15(4):395–401.
Lazaridis II, Kraljević M, Schneider R, et al. The impact of the COVID-19 pandemic on bariatric surgery: results from a worldwide survey. Obes Surg. 2020;30(11):4428–36.
World Health Organisation. Obesity and overweight. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 24 Aug 2022
Senthilingam M. COVID-19 has made the obesity epidemic worse, but failed to ignite enough action. BMJ. 2021;372:n411.
Robinson E, Boyland E, Chisholm A, et al. Obesity, eating behavior and physical activity during COVID-19 lockdown: a study of UK adults. Appetite. 2021;156: 104853.
Singhal R, Tahrani AA, Ludwig C, et al. Global 30-day outcomes after bariatric surgery during the COVID-19 pandemic (GENEVA): an international cohort study. Lancet Diabetes Endocrinol. 2021;9(1):7–9.
Singhal R, Ludwig C, Rudge G, et al. 30-day morbidity and mortality of bariatric surgery during the COVID-19 pandemic: a multinational cohort study of 7704 patients from 42 countries. Obes Surg. 2021;31(10):4272–88.
Singhal R, Wiggins T, Super J, Alqahtani A, Nadler EP, Ludwig C, et al. 30-Day morbidity and mortality of bariatric metabolic surgery in adolescence during the COVID-19 pandemic — the GENEVA study. Pediatr Obes; 2021; 16(12); e12832.
Vekaria B, Overton C, Wiśniowski A, et al. Hospital length of stay for COVID-19 patients: data-driven methods for forward planning. BMC Infect Dis. 2021;21(1):1–15.
Glasbey JC, Nepogodiev D, Simoes JFF, et al. Elective cancer surgery in COVID-19-free surgical pathways during the SARS-CoV-2 pandemic: an international, multicenter, comparative cohort study. J Clin Oncol. 2021;39(1):66–78.
Newbold R, Craven A, Aly A. Efficacy of patient selection criteria for obesity surgery in a non-high-dependency unit/intensive care unit facility. ANZ J Surg. 2021;91(7–8):1528–33.
Bolger JC, Kelly ME, Whelan C, et al. Public-private partnership: strategies for continuing urgent elective operative care during the COVID-19 pandemic. Br J Surg. 2020;107(9):e320.
Barker T, Barker P, Sokalsky L, et al. The use of the independent sector in providing NHS services during the COVID-19 outbreak; two hospitals experience. Surgeon. 2021;19(5):e213–6.
Rubino F, Cohen RV, Mingrone G, et al. Bariatric and metabolic surgery during and after the COVID-19 pandemic: DSS recommendations for management of surgical candidates and postoperative patients and prioritisation of access to surgery. Lancet Diabetes and Endocrinol. 2020;8(7):640–8.
Holman N, Knighton P, Kar P, et al. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study. Lancet Diabetes Endocrinol. 2020;8(10):823–33.
Brown AM, Ardila-Gatas J, Yuan V, et al. The impact of telemedicine adoption on a multidisciplinary bariatric surgery practice during the COVID-19 pandemic. Ann Surg. 2020;272(6):e306-10.
Chao GF, Ehlers AP, Telem DA. Improving obesity treatment through telemedicine: increasing access to bariatric surgery. Surg Obes Relat Dis. 2021;17(1):9–11.
Vitiello A, Berardi G, Musella M. Impact of COVID-19 lockdown on short-term weight loss in a single Italian institution: 1-year updated data. Obes Surg. 2022;32(3):924–5.
El Moussaoui I, Navez J, El Moussaoui K, et al. Impact of COVID-19 lockdown on short-term results after laparoscopic sleeve gastrectomy. Obes Surg. 2021;31(6):2614–8.
Pereira X, Romero-Velez G, Skendelas JP, et al. The COVID-19 pandemic did not affect target weight loss 1 year post bariatric surgery. Obes Surg. 2021;31(11):4926–32.
NHS Digital. Bariatric surgical procedures, 2021/22 (provisional)– National Obesity Audit. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/national-obesity-audit/bariatric-surgical-procedures-2021-22-provisional/content#highlights. Accessed 24 Aug 2022.
Clapp B, Ponce J, DeMaria E, Ghanem O, Hutter M, Kothari S, et al. (2022) American Society for Metabolic and Bariatric Surgery 2020 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis.
Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–6.
Zhang X, Lewis AM, Moley JR, et al. A systematic review and meta-analysis of obesity and COVID-19 outcomes. Sci Rep. 2021;11(1):7193.
Acknowledgements
List of Collaborators:
M. Lamota - Omni Hospital, Guayaquil, Ecuador
S. M. Raslan - Faculty of Medicine, Ain Shams University, Cairo Egypt
A. Sumer - Istinye University, School of Medicine, Medical Park Hospital, İstanbul, Turkey
S. Ugale - Kirloskar Hospital, Hyderabad, India
R. Kassir - CHU Felix Guyon, Saint Denis De La Réunion, France
A. Z. Balta - Avicenna Hospital, Istanbul, Turkey
K. Yarlagadda - Care Hospital, Hyderabad, India
M. L. Fage - Sanatorio Chivilcoy, Chivilcoy, Argentina
F. A. Espinosa - Clínica de Obesidad: Cirugía de Obesidad de los Altos, Tepatitlán De Morelos, Jalisco, Mexico
A. J. Mukherjee - Indraprastha Apollo Hospitals, New Delhi, India
P. R. Martinez Duartez - Hospital Universitario Austral, Buenos Aires, Argentina
D. Bedi - Hope Obesity Centre, Ahmedabad, India
M. M. Ozmen - Istinye University Medical School, Istanbul, Liv Hospital Ankara, Turkey
M. Kermansaravi - Hazrat-e Rasool Hospital, Tehran, Iran
E. Baldini - Ospedale “G. da Saliceto”, Piacenza, Italy
M. Narwaria - Asian Bariatrics Pvt. Ltd., Ahmedabad, India
O. M. Murshid - NJCH, Jeddeh, Saudi Arabia
A.-M. Adel - Centre Hospitalier regional d'ORLEANS, Orleans, France
C. Parikh - Devarsh Hospital, Vadodara, India
C. O. Ramirez-Serrano - Angeles Clinica Londres, Mexico City, Mexico
F. Martini - Clinique des Cedres, Cornebarrieu, France
R. Wadhawan - Manipal Hospital, Dwarka, New Delhi, India
R. P. Vargas - Hospital General San Francisco, Quito, Ecuador
F. Pizza - A Rizzoli, Napoli, Italy
S. Carandina - Clinic Saint Michel, Toulon, France
M. C. Kizilkaya - University of Health Sciences, Kanuni Sultan Süleyman Training and Research Hospital, Istanbul, Turkey
M. Ilić - Clinic for thoracic surgery, Institute for Lung Diseases, Sremska Kamenica, Novi Sad, Ap Vojvodina, Serbia
P. A. Lamoza - Hospital El Carmen, Santiago, Chile
T. Bilecik - Istinye University Faculty of Medicine, Mersin, Turkey
M. C. Torres - Hospital sírio libanês, São Paulo, Brazil
C. Guevara - Hospital Universidad Nacional, Bogota, Colombia
J. E. Garcia-Flores - Christus Muguerza, Monterrey, Mexico
N. Sakran - Holy Family Hospital, Azriali, Faculty of Medicine, Bar- Ilan University, Ramat Gan, Israel, Nazareth, Israel
S. Arana-Garza - Christus Muguerza Conchita, Monterrey, Nuevo León., Mexico
M. Khaitan - K D Hospital, Ahmedabad, India
F. Karateke - VM Medical Park Mersin Hospital, Mersin/Turkey, Turkey
V. Valenti - University Hospital of Navarra, Pamplona, Spain
N. Tartaglia - Policlinico Riuniti Foggia, Foggia, Italy
N. Dukkipati - KIMS-LIVLIFE, Hyderabad, India
S. Chiappetta - Ospedale Evangelico Betania, Naples, Italy
M. Musella - Advanced Biomedical Sciences Department – “Federico II” University, Naples, Italy
M. G. Carvalho - Hospital do Espírito Santo - Évora, Évora, Portugal
E. Pinotti - Policlinico San Pietro, Ponte San Pietro, Italy
A. Prasad - Apollo Hospitals; New Delhi, India
K. Shah - Centralsjukhuset Kristianstad, Kristianstad, Sweden
E. Baili - Laiko General Hospital, National and Kapodistrian University of Athens, Athens, Greece
S. Imran Abbas - Iranian Hospital, Dubai, United Arab Emirates (UAE)
C. Nagliati - San Giovanni di Dio Hospital, Gorizia, Italy
O. Viveiros - Hospital Lusiadas Amadora, Lisbon, Portugal
R. JS Ribeiro - Hospital Lusiadas Amadora, Amadora, Portugal
L. Angrisani - University of Naples, Naples, Italy
S. Soriano - Pennsylvania Hospital, Philadelphia, United States of America (USA)
A. C. Abbadi - Clinique De L'Yvette, Longjumeau, France
N. T. Kawahara - Hospital Sirio Libanes, São Paulo, Brazil
P. Praveen Raj - Gem Hospital & Research Centre Coimbatore, India
G. Siddiq
H. A. Balamoun - Cairo University Teaching Hospitals - Kasr Al Aini, Cairo, Egypt
C. Vaz - Hospital CUF Tejo, Lisboa, Portugal
A. Govil Bhasker - Apollo Spectra Hospital Mumbai, India
J. Himpens - CHIREC Delta, Brussels, Belgium
A. Techagumpuch, Thammasat University Hospitao, Pathumtani, Thailand
A. Shrivastava - Gokuldas and Medanta Hospitals, Indore, India
M. Valeti - Continental Hospitals, Hyderabad, India
B. Bokobza - Hospital Group of Le Havre, Le Havre, France
A. Bashir - Jordan Hospital, Amman, Jordan
S. Avallone - Clinique du Cap d'or, La Seyne Sur Mer, France
H. Sebbag - Private Hospital of Provence, Aix-En-Provence, France
M. A. Escarti Uso - HLA-Moncloa, HLA-La Vega, HLA-Vistahermosa (HLA-Hospitals Group, Spain) Valencia (Spain), 80 Cases/Year, Spain
A. E. Rodriguez - Hospital de Clínicas, Asuncion, Paraguay
D. Awruch - Sanatorio Britanico de Rosario, Rosario, Argentina
C. Ortiz Silva - Hospital El Tunal, Bogota, Colombia
A. Garcia Ruiz De Gordejuela - Vall d'Hebron University Hospital, Brarcelona, Spain
C.-K. Huang
E. Manno - Ospedale Cardarelli, Napoli, Italy
E. Ruiz-Ucar - Fuenlabrada University Hospital, Fuenlabrada, Madrid, Spain
J. M. Balibrea - Hospital Clínic de Barcelona, Barcelona, Spain
S. P. Marcoen - AZ Glorieux, Ronse, Belgium
C. Kirkil - Firat University Hospital, Elazig, Turkey
A. Maleckas - Lithuanian University of Health Sciences, Kaunas, Lithuania
T. Pham - Niagara Falls Memorial Medical Center, Niagata Falls, United States of America (USA)
J. Hazebroek - Rijnstate Hospital, Arnhem, Netherlands
W. Al-Khyatt - Royal Derby Hospital, Derby, United Kingdom (UK)
T. Poghosyan - Hôpital Européen Georges Pompidou, Université de Paris, Paris, France
J. W. Mall - Nordstadt and Siloah Hospaital, Hannover, Germany
R. Goel - Primus Hospital, Delhi, India
P. Noel - Emirates Specialty Hospital, Dubai, United Arab Emirates (UAE)
V. Bindal - Sir Ganga Ram Hospital, New Delhi, India
G. Prasad - G Madegowda Super Speciality Hospital, Mandya, India
O. M. Gomez Davila
L. Kow - Flinders Private Hospital, Adelaide, Australia
M. Focquet - AZ Sint Elisabeth, Zottegem, Belgium
T. Omerov - Azerbaijan Medical University, Baku, Azerbaijan
A. Pantelis - Evaggelismos General Hospital of Athens, Athens, Greece
H. A. D. V. Cunha - Clínica Vitali Campinas, Brazil
C. Zerrweck - Hospital ABC Santa Fe Mexico City, Mexico
V. Dejeu - MedLife Genesys, Arad, Romania
S. A. Taha - Mediclinic Airport Road Hospital, Abu Dhabi, United Arab Emirates (UAE)
Y. G. Dominguez - Hospital de Torrevieja, Alicante, Spain
C. Copaescu - Ponderas, Academic Hospital, Bucharest, Romania
A. Ribeiro Meyer Pflug
F. J. Martinez-Ubieto - Viamed Montecanal Hospital, Zaragoza, Spain
A. Usai - U. Parini Hospital Aosta, Italy
G. Kumar Juneja - Al Zahra Hospital Dubai, United Arab Emirates (UAE)
M. Moustafa Basho
N. Beglaibter - Hadassah Mount Scopus, Jerusalem, Israel
T. Pintar - UMC Ljubljana, Ljubljana, Slovenia
N. Ağbaba
M. Anselmino - Azienda Ospedaliera Universitaria Pisana, Pisa, Italy
A. Thorell - Ersta Hospital, Stockholm, Sweden
O. Şen - Nişantaşı University Faculty of Medicine, İstanbul, Turkey
T. Wiggins - Musgrove Park Hospital, Taunton, United Kingdom (UK)
N. F. Trelles - RENE DUBOS, Pontoise, France
G. Oren - Medicana Kadıköy, Istanbul, Turkey
A. G. N. Robertson - NHS Fife, Kirkcaldy, United Kingdom (UK)
E. Chousleb Mizrahi - Jackson North MEdical Center, Miami, Florida, United States of America (USA)
G. Sevá-Pereira - Hospital Vera Cruz, Campinas, Sp, Brazil
F. A. Carvalho – CEMIL, Umuarama, Brazil
A. K. Salman - King Fahd Hospital, Jeddah ,Saudi Arabia
G. Dapri - International School Reduced Scar Laparoscopy, Brussels, Belgium
Dr. P. H. Salvi - Jupiter Hospital, Thane, Mumbai, India
M. Ustun - Memorial Hospital, Istanbul, Turkey
A. H. Davarpanah Jazi – Khanevade, Isfahan, Iran
A. Zandi - Atieh, Tehran, Iran
M. I. Allouch - Nini General Hospital, Tripoli, Lebanon
C. Boza - Clínica Las Condes, Santiago, Chile
C. Esquivel - Sanatorio Allende, Córdoba, Argentina
M. A. Carbajo - Campo Grande Hospital, Valladolid, Spain
M. Ul Hassan - Shalimar Medical and Dental College, Lahore, Pakistan
Dr. A. A. Graniel Diaz - Hospital Quirurgico Graniel, Comalcalco, Mexico
M. H. Elfawal - Makassed General Hospital, Beirut, Lebanon
J. V. Ferrer - Clínica Obésitas, Madrid, Spain
D. Mazza - Hôpital Sainte Musse, Toulon, France
S. Olmi - San Marco Hospital – GSD, Zingonia - Osio Sotto, Italy
V. Soni - Max Hospital, Saket, New Delhi, India
M. Uccelli - San Marco Hospital – GSD, Zingonia - Osio Sotto, Italy
G. E. Jones - Royal Berkshire NHS Foundation Trust, Reaing, United Kingdom (UK)
L. S. Kona - Global Hospital, Hyderabad, India
D. Cottam - Bariatric Medicine Institute, Salt Lake City, United States of America (USA)
B. B. Khatsiev - Stavropol State Medical University Stavropol, Russia
M. Zuluaga Zuluaga - Hospital Universitario Del Valle, Cali, Colombia
K. Gawdat - Ain Shams, University School of Medicine Hospital, Cairo, Egypt
H. P. Povoas - Hospital de Ilheus, Ilheus, Brazil
P. Major - 2nd Department of General Surgery, Jagiellonian University Medical College, Krakow, Poland
H. Al-Momani - Danat Al Emarat Hospital, Abu Dhabi, United Arab Emirates (UAE)
M. Kurian – NYU, New York, United States of America (USA)
F. C. Campanile - San Giovanni Decollato – Andosilla, Civita Castellana, Italy
D. Hazzan - Sheba Medical Center, Tel Aviv, Israel
A. M. Alhallak - Saint Louis Hospital, Almahayni Modern Hospital, Almanar International Hospital, Damascus, Syria
G. J. Kowalski - KCM Clinic, Jelenia Gora, Poland
K. Kaseja - Independent Public Clinical Hospital No. 2 of the Pomeranian Medical University, Szczecin, Poland
M. Daskalakis - Heartlands Hospital Birmingham, United Kingdom (UK)
A. Raziel - Assuta Medical Center, Tel Aviv, Israel
K. Albanopoulos - Hippocration General Hospital, Athens Medical School, National and Kapodistrian University of Athens, Athens, Greece
A. Charalabopoulos - Interbalkan Hospital Centre, Athens,Greece
G. Jutten - AZ Klina, Brasschaat, Belgium
P. G. Patel - Zydus Hospital and Healthcare Research Center, Anand, India
A. Ahuja - Sir Ganga Ram Hospital New Delhi, India
T. Mittal - Sir Ganga Ram Hospital, New Delhi, India
A. Shabbir - National University Hospital of Singapore, Singapore, Singapore
M. Mehrotra - Apex Hospital, Moradabad, India
E. Facchiano - Santa Maria Nuova Hospital, Florence, Italy
A. Morrell - Rede DOr São Luiz, São Paulo, Brazil
A. J. Torres - Hospital Madrid Monteprincipe. Hospital Clinico San Carlos, Madrid, Spain
R. Liem - Groene Hart Hospital in Gouda, Dutch Obesity Clinic in The Hague and Gouda, The Hague and Gouda, The Netherlands
T. L. Simpson - St. Johns Regional Medical Center, Oxnard, United States of America (USA)
A. C. Ramos – Gastro Obeso Center, Sao Paulo, Brazil
M. Takieddine - CHU Charleroi & Vésale, Montigny Le Tilleul, Belgium
S. Aggarwal - All India Institute of Medical Sciences (AIIMS), New Delhi, India
P. Chowbey - Max Super-Speciality Hospital, New Delhi, India
L. Piazza - ARNAS Garibaldi, Catania, Italy
A. Pajtak - General Hospitali Varazdin, Varazdin, Croatia
M. Aznan Shuhaili - Salam Specialist Hospital, Kuala Lumpur, Malaysia
Z. Boras - Clinical Hospital Osijek, Osijek, Croatia
J. S. Azagra - Centre Hospitalier de Luxembourg, Luxembourg, Luxembourg
M. G. Qassem - Ain Shams University Hospitals, Cairo, Egypt
M. R. Elbanna - Ain Shams University Hospitals, Cairo, Egypt
A. Ali
R. Franken - Spaarne gasthuis, Hoofddorp, Netherlands
D. Pournaras - North Bristol NHS Trust, Bristol, United Kingdom (UK)
S. Mansour - Imperial College Healthcare NHS Trust, London, United Kingdom (UK)
N. Apáez Araujo - General Hospital Dr Ruben Leñero, Hospital Merlos, Mexico
A. Krikhely
C. Parmar - Whittington Hospital, London, United Kingdom (UK)
M. Lo - Hospital de Clínicas, Asunción, Paraguay
H. Ajami
R. Yarram – VPS, Abudhabi, United Arab Emirates (UAE)
H. Kais - HMC Herzlya, Israel
O. Al-Taan
M. W. Hii - St Vincent's Hospital, Melbourne, Australia
F. J. Barrera Rodriguez - Christus Muguerza Hospital Sur, Monterrey, Mexico
H. M. Elghadban - Elsafa private Hospital Damietta City, Egypt
J. Jpc Pérez Cruz
S. Ramirez - Hospital Guadalajara, Tijuana, Mexico
A. Lázaro - Centro Hospitalar e Universitário de Coimbra Coimbra, Portugal, Portugal
M. Riera - Royal Shrewsbury Hospital, Shrewsbury,United Kingdom (UK)
S. Awad - Royal Derby Hospital, Derby, United Kingdom (UK)
G. NS Neto - Memorial São Jose, Recife, Brazil
M. E. Valencia A - Clínica Universitaria Bolivariana, Medellin, Colombia
J. C. Olivares - Regional del Río Hospital, Reynosa, Tamaulipas, México, Mexico
J. A. Altuve – Maranatha, Guatemala
J. Parmar
R. V. Cohen – The center for Obesity and Diabetes, Oswaldo Cruz German Hospital, Obesity Good Bye Center, Sao Paulo, Brazil
S. Verboonen - Obesity Good Bye Center, Tijuana, Mexico
M. De Luca - Montebelluna Hospital, Treviso, Italy
H. J. Antoine - Robert Wood Johnson University Hospital, New Brunswick, United States of America (USA)
Y. Núñez Santana
J. C. Carrasco Flores - Clínica González, Lima, Peru
R. Cuellar Tamez
G. Ungson - Hospital CIMA, Hermosillo, Mexico
P. Salminen - Turku University Hospital, Turku, Finland
E. Dilektasli - Bursa Life Hospital, Bursa, Turkey
L. Antozzi - Argentina
H. Z. Adi - King Salman Armed Forces Hospital, Tabuk, Saudi Arabia
A. Leyva-Alvizo - San José-Tecsalud, Monterrey, Mexico
S. V. Andino - Sanatorio Mayo, Clinical Doctor Bariatric Surgery, Cordoba Argentine
R. J. Romero- Hospital Covadonga, Veracruz, Mexico
N. Nizami
M. Proczko-Stepaniak - Medical Univesity of Gdansk, Gdansk, Poland
M. Romeijn - Máxima Medical Center, Eindhoven-Veldhoven, Netherlands
I. W. Abreu - Meridional Hospital, Cariacica, Brazil
M. Peter - Huddersfield Royal Infirmary, Huddersfield, United Kingdom (UK)
S. M. Ward - St Vincent's Hospital Melbourne, Melbourne, Australia
R. Nassar - University Hospital Fundación Santa Fe De Bogotá, Bogotá, Colombia
H. M. A. Aboshanab - King Abdul Aziz Hospital, Alhasa, Saudi Arabia
J. F. Ortega - Bité Médica, Private Hospital, Mexico
M. K. Mirza Gari - Dammam Medical Complex, Al Dammam, Saudi Arabia
W. Yang - The First Affiliated Hospital of Jinan University, Guangzhou, China
F. Favretti - Casa di Cura Villa Berica, Vicenza, Italy
J. A. Kristinsson - Oslo University Hospital, Oslo, Norway
M. M. Bashah - Hamad General Hospital, Doha, Qatar
L. F. V. D. Mesquita - Hospital Sao Marcos, Uberaba, Brazil
F. J. Cantu - Advanced Medicine Institute, Reynosa, Mexico
H. E. Taskin - Istanbul University Cerrahpasa-Cerrahpasa Medical Faculty, Istanbul ,Turkey
J. Gonzalez - Centro Médico de Asturias, Oviedo, Spain
P. Lamb - Royal Infirmary Edinburgh, Edinburgh, United Kingdom (UK)
C. E. Boru - General Surgery & Bariatric Center of Excellence IFSO-EC, University LA Sapienza of Rome, Latina, Italy
A. Hussain - Doncaster Royal Infirmary, Doncaster, United Kingdom (UK)
B. Alkhaffaf - Salford Royal NHS Foundation Trust, Manchester, United Kingdom (UK)
P. S. Jambulingam - Luton and Dunstable University Hospital, United Kingdom (UK)
C. H. Tog - Victoria, Australia
J. D. Picardo - Sanatorio Belgrano MDP, Mar Del Plata, Argentina
A. Neimark - Almazov National Medical Research Center, Saint-Petersburg, Russia
B. J. Ammori - Burjeel Hospital, Abu Dhabi, United Arab Emirates (UAE)
Z. Dong - First affiliated hospital of Jinan University, Guangzhou, China
U. H. Garcia Trujillo - Hospital Star Medica Chihuahua, Chihuahua, Chih., Mexico
L. A. Layani - Al Sharq Hospital, Fujairah, United Arab Emirates (UAE)
V. Salsano - Clementville Clinic, Montpellier, France
A. Tank
B. Zilberstein - Beneficiencia Portuguesa de São Paulo, São Paulo, Brazil
D. Pajecki - Hospital 9 de Julho, Sâo Paulo, Brazil
A. K Saha - Huddersfield Royal Infirmary, Huddersfield, United Kingdom (UK)
T. Al Shaban - Sheikh Khalifa Medical City, Abu Dhabi, United Arab Emirates (UAE)
E. Topal - Bursa Obesity and Diabetes Clinic, Bursa, Turkey
D. Van Der Fraenen - Asz, Aalst, Belgium
M. E. Jimenez Amin - Clínica Portoazul, Barranquilla, Colombia
F. P. Galaz - Hospital Ángeles Lomas, Mexico City, Mexico
N. Z. Abdo - NMC Najran Hospital, Najran, Saudi Arabia
A. A. R. Mohamed - National Guard Hospital, Al Madinah, Saudi Arabia
L. Poggi - Clinica Anglo Amricana, Lima, Peru
H. Çiyiltepe - Health Science University, Istanbul Fatih Sultan Mehmet Training and Research Hospital, Istanbul, Turkey
C. R. Wietzycoski - Unimed Vale do Caí Hospital, Montenegro, Brazil
G. GS Scalera - Clinica Ruesch, Naples, Italy
R. Goel - Wockhardt Hospital, Mumbai, India
N. T. Santos - Rios Dor, Rio De Janeiro, Brazil
A. Inam - Pakistan Institute of Medical Sciences, Islamabad, Pakistan
E. Mans - Hospital de Mataró, Mataró, Spain
M. Altarawni - Salford Royal NHS Foundation Trust, Manchester, United Kingdom (UK)
M. Al Hadad - Healthpoint Hospital, Abu Dhabi, United Arab Emirates (UAE)
A. Mejdane - Clinique Tingis, Tangier, Morocco
A. A. S. Mhanna
S. Martin
M. Akbaba - Samsun Atasam Private Hospital, Samsun, Turkey
S. A. Shah - SIR Ganga Ram Hospital, Lahore, Pakistan
D. Birk - Roh Kliniken Ludwigsburg/Bietigheim, Germany
Md T. Adil - Luton and Dunstable University Hospital, Luton, United Kingdom (UK)
M. M. Torres - Hospital Dr Gali González, Quito, Ecuador
H. M. Elmaleh - Ain Shams University Hospitals, Cairo, Egypt
K. Miller - Diakonissen Wehrle Private Hospital, Salzburg, Austria
K. Malapan - Gleneagles Hospital Penang, Georgetown, Penang, Malaysia
H. Matar - Burjeel Hospital, Abu Dhabi, United Arab Emirates (UAE)
R. Mamidanna - Luton and Dunstable University Hospital, Luton, United Kingdom (UK)
A. A. Gudal - King Abdullah Medical Complex, Jeddah, Saudi Arabia
E. A. Aljohani - Prince Sattam bin Abdulaziz University, Riyadh, Saudi Arabia
J. L. Estrada - Hopital General Universitario, Alicante, Spain
F. E. Fiolo - Hospital Privado de Comunidad, Mar Del Plata, Argentina
M. N. Md Hashim - Hospital Universiti Sains Malaysia, Kota Bharu, Kelantan, Malaysia
M.-R. Prieto-Aldape - Jardines Hospital, Guadalajara, Mexico
M. Niazi - St. Louis Hospital, Aleppo, Syria, Syria
R. X. Cuellar Tamez - Hospital Zambrano Hellion, San Pedro Garza Garcia, Mexico
J. Dargent - Polyclinique Lyon Nord, Lyon, France
O. M. Alharbi - Farwaniyah, Farwaniyah, Kuwait
A. Katakwar - AIG Hospitals, Hyderabad, India
F. Dalati - Estuaire Private Hospital, Le Havre, France
S. Sharma - Fortis Hiranandani Hospital, Navi Mumbai, India
T. A. Samarkandy - Dameron & Lodi Adventist Health/Sutter, Stockton/Lodi, United States of America (USA)
M. A. M. F. Farina Del Rio - Hospital de Clinicas FCM/UNA, Asuncion, Paraguay
S. Dawani - Dr. Ziauddin Hospital, Clifton Campus, Karachi, Pakistan
M.-T. Van Der Merwe - Netcare Waterfall City Hospital, Midrand, South Africa
M. L. P. Vilas-Boas - Hospital Santo Amaro, Salvador, Brazil
A. A. Moustafa - Ain Shams University Hospitals, Cairo, Egypt
O. Dukhno - Soroka University Medical Center, Beer Sheva, Israel
A. Ahmed - University Hospitals of Leicester NHS Trust
F. Eghbali - Rasoul Akram Hospital, Tehran, Iran
S. K. Bandyopadhyay
A. U. H. Khan - Walsall Manor, Walsall, United Kingdom (UK)
A. G. K. Li - Salford Royal Hospital, Manchester, United Kingdom (UK)
M. Fehervari - Imperial College Healthcare NHS Trust, London, England
E. Silva - Country Clinic, Bogota, Colombia
M. Kostalas
T. Salih - St Richards Hospital, Chichester, United Kingdom (UK)
H. Hamed - Truelife Bariatric and Digestive Surgery Center, Mansoura, Dakahleyya, Egypt
R. Bolckmans
B. Amr - Royal Cornwall Hospital, Truro, United Kingdom (UK)
R. Welbourn - Musgrove Park Hospital, Taunton, United Kingdom (UK)
J. A. M. Cervantes - Hospital Satelite, Naucalpan, Mexico
V. Menon - University Hospitals Coventry & Warwickshire NHS Trust, Coventry, United Kingdom (UK)
B. Marzano - Humanitas Gavazzeni Bergamo, Bergamo, Italy
M. Garcia Garza - Swiss Hospital, Monterrey, Mexico
S. Talwar - Manipal Hospital, HAL, Bangalore, Bangalore, India
J. A. Jimenez - Arboledas Hospital, Guadalajara, Mexico
J. R. Ramos-Kelly - Hospital Ángeles, Tijuana, Mexico
R. Lutfi - Advocate Illinois Masonic Medical Center, Chicago, United States of America (USA)
F. A. Husain - Oregon Health & Science University, Portland, United States of America (USA)
H. M. Heneghan - St Vincent's University Hospital, Dublin, Ireland
K. Patel - Northern General Hospital, Sheffield, United Kingdom (UK)
M. R. Junior - Santa Marta Hospital, Brasília, Brazil
F. Viegas - Copa Dor, Rio De Janeiro, Brazil
M. Avalos-Avalos - Puerta de Hierro Sur, Guadalajara, Mexico
Z. Nor Hanipah - Department of Surgery, Faculty of Medicine and Health Sciences, University Putra Malaysia, Kuala Lumpur, Malaysia
R. Snoekx - Bravis, Bergen-Op-Zoom, Netherlands
C. A. Diaz Rincon - Clinica VIP, Bogota, Colombia
R. Aceves - Christus Muguerza Hospital Reynosa, Reynosa, Tamaulipas, Mexico
M. Fadhel - Medical City, Baghdad, Iraq
S. A. Cahalan - Iowa Methodist Medical Center, Des Moines, United States of America (USA)
Dr. D. M. Jasim
M. S. Al-Hamadani - Basra Teaching Hospital, Basrsh, Iraq
M. K. Albermani
H. S. Ali - Baghdad Teaching Hospital, Medical City Complex, Baghdad, Iraq
W. J. Altaee
H. D. Almussawi - Baghdad Teaching hospital, Baghdad, Iraq
A. S. B. Silva - Ordem de S. Francisco, Porto, Portugal
A. A. Atra - Baghdad Teaching Hospital, Baghdad, Iraq
A. A. Majeed
A. N. Al-Turfi - Baghdad hospital, Baghdad, Iraq
O. S. Alomar - Al Araby Private Hospital, Baghdad, Iraq
G. Kalogeropoulos - Eastern Health, Melbourne, Australia
I. G. Tzvetkov - 1, Sofia, Bulgaria
R. M. Rajneesh
H. Khwaja - Chelsea and Westminster Hospital, London, United Kingdom (UK)
D. Foschi - Saint Joseph Hospital, IRCCS Multimedica, Milan, Italy
G. N. Al Hajj
A. Assalia - Rambam Health Care Campus, Haifa, Israel
F. Khaleal - Holroyd Private Hospital, Sydney, Australia
M. Solovyeva - American Medical Clinic and Hospital, Saint-Petersburg, Russia
A. A. A. Salem - Al Rahma Hospital, Cairo, Egypt
H. Takla - Winchester, MA, United States of America (USA)
H. A. Alshurafa
N. Alrifai - Zulekha Hospital Sharja, Sharja and Dubai, United Arab Emirates (UAE)
A. Muñoz-Mora - Clinica del Country, Bogotá, Colombia
G. Martinez De Aragon - Hospital Universitario de Alava, Vitoria-Gasteiz, Spain
V. V. Diaconu - Provita Hospital, Bucharest, Romania
N. A. Alenazi - Saudi Germany Hospital, Riyadh, Saudi Arabia
M. Kaplan - NCR International Hospital, Gaziantep, Turkey
P. C. Grippa - Hospital Beneficente Unimar, Marília, Brazil
P. D. Nottle - The Avenue Hospital, Melbourne, Australia
L. A. C. Fonseca - University Hospital Lauro Wanderley UFPB, João Pessoa, Brazil
R. C. Luciani - Groupepe Hospitalier Les Portes du Sud, Venissieux, France
M. L. Talbot - St George Private Hospital, Sydney, Australia
Y. C. Park - Seoul Slim Surgery, Seoul, South Korea
E. Nacur Silva - Santa Casa de Belo Horizonte, Belo Horizonte, Brazil
G. Merola - San Giovanni di Dio Hospital, Frattamaggiore, Italy
V. Sharma - Meenakshi Hospital, Ghaziabad, India
A. M. Elghandour - Ain Shams University Hospital, Cairo Egypt
E. J. Behrens - New Life Center, Guatemala, Guatemala
A. Sharples - University Hospitals of North Midlands, Stoke on Trent, United Kingdom (UK)
J. M. Pestana - Clinica Sanatrix, Caracas, Venezuela
J. Monterrubio - Christus Muguerza Sur, Monterrey, Mexico
E. L. De Souza Bastos - Santa Casa de Marilia, Marilia, Brazil
N. S. Alalwani
D. A. Mohammed
H. L. Kathrein - A.o. Krankenhaus St. Vinzenz, Zams, Austria
F. N. Schutte - Sunward Park Hospital, Johannesburg, South Africa
A. Sava - Helsingborg's Hospital, Helsingborg, Sweden
M. D. L. A. Mayo-Ossorio - Hospital Universitario Puerta del Mar, Cadiz, Spain
D. A. Manrique
S. Shahabi - Rasool-e Akram Hospital, Tehran, Iran
C. EMIR Guldogan - Liv Hospital Ankara, Ankara, Turkey
D. Gärtner - Municipal Hostpital Karlsruhe, Karlsruhe, Germany
R. KSAN Ksantini - Ernest Conseil la Rabta, Tunis, Tunisia
E. Boutry - University hospital Nîmes, Nîmes, France
G. S. Mazzini - Hospital Moinhos de Vento, Porto Alegre, Brazil
K. P. Rheinwalt - St. Franziskus Hospital Cologne, Cologne, Germany
A. Pagan
O. Ospanov - GreenClinic, Nur-Sultan, Kazakhstan
S. S. Saggu - CK Birla Hospital, New Delhi, New Delhi, India
S. A. E. S. Alsubaie - Sidra Hospital, Jahra Governerate, Kuwait
M. Walędziak - Military Institute of Medicine, Warsaw, Poland
B. Fallatah - Sumuo mefical, Khobar, Saudi Arabia
A. Edenberg - Sørlandet sykehus, Arendal, Norway
M. Abdullah - Alsaaha Specialized Hospital, Khartoum, Sudan
N. R. Floch - Norwalk Hospital, Norwalk Connecticut, United States of America (USA)
Dr. J. Stewart - HSC Winnipeg, Winnipeg, Canada
D. V. Timofte - Sf. Spiridon Emergency Hospital, Iasi, Romania
A. E. Jawed - Hackensack Meridien Health JFK Medical Center, Florham Park, NJ, United States of America (USA)
A. Bhambri
M. Hany - Medical Research Institute, Alexandria, Egypt
S. A. Jain
I. Terzis - King Salman specialist hospital, Hail, Saudi Arabia
L. Level - Clinica Santa Sofia, Caracas, Venezuela
M. A. Al Sayyad - Hammoud University Medical Center, Saida, Lebanon
H. Ahmed - Department of Surgical Oncology, Shuakat Khanum Memorial Cancer Hospital and Research Centre, Lahore and Karachi, Pakistan
M. Devadas - Nepean Hospital, Sydney, Australia
A. C. J. Coelho - Hospital Rios Dor, Rio De Janeiro, Brazil
S. S. Shah - Laparo Obeso Centre, LOC Healthcare LLP, Pune, India
R. J. Anacona C. - Hospital Regional de Talca, Talca, Chile
A. B. Palacios - Hospital Básico Ambato, Ambato, Ecuador
D. N. Ismael - Royal Private Hospital, Sulaimanyah, Iraq
U. Iqbal - Karachi, South City Hospital, Pakistan
H. R. Herrera - National Hospital of Itaugua, Itaugua, Paraguay
D. Goitein - Sheba Medical Center, Ramat Gan, Israel
R. M. Quinino - Hospital Unimed de Natal, Natal, Brazil
G. Spiliopoulos - Breteché Clinic ELSAN Group, Nantes, France
P. Pjz Zambrana - Modelo, Tucuman, Argentina
R. Villagran - Bupa Clinica, Antofagasta, Chile
A. Ghazal
F. Frattini - ASST Settaghi, Tradate- Varese, Italy
M. Battistoni - Aoui Verona, Verona, Italy
K. Stamou - Mitera Hospital, Athens, Greece
Z. Bodnar - Letterkenny University Hospital, Letterkenny, Ireland
H. Sinan - Kadikoy Florence Nightingale Hospital, Istanbul, Turkey
V. L Nirujogi - Marshfield Medical Center, Marshfield, United States of America (USA)
O. Taha - Osama Taha Group, Cairo, Egypt
S. Hu - the first affiliated hospital of Jinan University, Guangzhou, China
M. E. M. Mahfouz - AlJazeera Medical Hospital, Riyadh, Saudi Arabia
L. U. Biter - Franciscus Gasthuis, Rotterdam, Netherlands
H. Ibrahim - Aleppo Private Hospital, Aleppo, Syria
L. Jordan
J. Hill - Coliseum Medical Centers, Macon, United States of America (USA)
M. M. H. Mohammed - Zagazig University Hospital, Zagazig, Egypt
L. X. Armijos - Hospital Naval De Guayaquil, Tena, Ecuador
R. Vilallonga - Universitary Hospital Vall Hebron, Universitat Autònoma De Barcelona, Barcelona, Spain; Hospital De Barcelona, Barcelona, Spain; Fellow of The European Board of Surgery - MIS, Barcelona, Andorra
L. A. Zavala Salazar - Christus Muguerza Sur, Monterrey México
J. F. Schrapps - Christus St Elizabeth, Beaumont, United States of America (USA)
K. Al Amri - Nizwa Hosptial, Nizwa, Oman
G. J. Muzio - Sanatorio Del Oeste, Ituzaingó, Argentina
A. Y. Abualsel - King Hamed University Hospital, Muhrraq, Bahrain
M. Kurian
L. Szczerbinski - Medical University of Bialystok Clinical Hospital, Bialystok, Poland
C. M. Trindade - Centro Hospitalar De Setúbal EPE, Setúbal, Portugal
A. Forieg
F. Schwoch
L. Genser - Sorbonne Université, Assistance Publique-Hôpitaux De Paris (AP-HP), Department of Hepato-Biliary and Pancreatic Surgery, Pitié-Salpêtrière University Hospital, Paris, France
A. Osman - Ain Shams University Hospitals, Cairo, Egypt
M. D. A. Menezes - Santa Casa, Londrina, Brazil
H. Özgüç - Private Medicabil Hospital, Bursa, Turkey
H. A. V. Cunha - Vera Cruz Campinas, Campinas, Brazil
M. S. Sbaï Idrissi - Clinique Claude Bernard 95120 Ermont, Ermont, France
B. Gülcü - Medicana Bursa Hospital, Bursa, Turkey
A. Contine - Città Di Castello Hospital, Città Di Castello, Italy
L. F. Rossi - Hospital Leforte, São Paulo, Brazil
A. Isik - Erzincan University, Erzincan, Turkey
O. A. Khan – St. Georges Hospital, Erzincan, Turkey
L. G. De Oliveira E. Silva - Ipanema Federal Hospital, Rio De Janeiro, Brazil
M. K. Bartın - Van Training and Education Hospital, University Of Health Sciences, Leicester, United Kingdom (UK)
S. Yardımcı
E. Yardimci
P. E. Pinto Jr - Hospital Das Clínicas of São Paulo, São Paulo, Brazil
I. A. Hassan
C. L. Yeap - Gleneagles Kuala Lumpur, Kuala Lumpur, Malaysia
R. Arias - Centro Medico Imbanaco, Cali, Colombia
A. H. Hamouda - Nuffield Hospital, Kent, United Kingdom (UK)
E. A. Dorado – Oeclinic, Cali, Colombia
C. Simoneti - Hospital Miguel Soeiro Sorocaba, Sorocaba, Brazil
P. Vasas - Doncaster Royal Infirmary, Doncaster, United Kingdom (UK)
L. Paolino - Centre Hospitalier Intercommunal De Créteil, Créteil, France
R. C. De Ajuria - Clincob@hotmail.com
V. Borrelli - San Donato Group, Bergamo, Italy
A. A. Shamim - Mercy Clinic, Fort Smith, United States of America (USA)
M. F. Herrera - ABC Medical Center, Mexico City, Mexico
J. Galindo Alvarez - University Hospital Ramón Y Cajal, Madrid, Spain
W. J. Wong - University Of Malaya Medical Centre, Kuala Lumpur, Malaysia
S. R. Prasad - Royal Adelaide Hospital, Adelaide, Australia
S. Aly - Herzogin Elisabeth Hospital, Braunschweig, Germany
F. C. Karaca - Istanbul Cerrahi Hospital, Istanbul, Turkey
S. Weiner - Nordwest Krankenhaus, Frankfurt, Germany
M. A. Kazak - VM Medicalpark Mersin Hospital, Mersin, Turkey
M. Motwani - Aastha Bariatrics, Mumbai, India
Ç. Büyükkasap - Gazi University Faculty of Medicine, Ankara, Turkey
A. Rizzi - Galmarini Hospital Tradate, Italy
S. K. Niazi - Southcity Hospital, Karachi, Pakistan
Dr. M. H. Alatrakhiam
N. Pararas - Hygeia Hospital, Athens, Greece
A. F. Ibrahim - Sarawak General Hospital, Kuching, Malaysia
D. Youssef - Clínica Tarapaca, Iquique, Chile
J. C. Marchesini - Marcelino Champagnat Hospital, Curitiba, Brazil
J.-M. V. Correia-Neves - Hospital CUF Descobertas, Lisbon, Portugal
A. Shreekumar - Laparo Obeso Centre, Pune, India
I. Elwardany
S. Demirli Atici - University of Health Sciences Tepecik Training and Research Hospital, Izmir, Turkey
J. Lorenzo Pérez - University Hospital La Ribera, Valencia
K. C. Ng - St. Vincent's University Hospital, Dublin, Ireland
C. Stier - Obesity Center Northrhine Westphalia, Huerth, Germany
M. Hany Ashour - Madina Women's Hospital, Alexandria, Egypt
H. M. Elmaleh - Ain Shams University Hospitals, Cairo, Egypt
C. A. S. Madalosso - Hospital Sao Vicente De Paulo, Passo Fundo, Brazil
P. Vasas - Doncaster Royal Infirmary, Doncaster, United Kingdom (UK)
S. Raslan - Armed Forces Hospitals Taif Region, Taif, Saudi Arabia
Funding
The study was funded by the Bariatric Unit’s Research Funds at University Hospitals Birmingham NHS Foundation Trust (Birmingham, UK). There was no sponsor, and the study was designed and conducted by the study group and the authors on behalf of GENEVA collaborators.
Author information
Authors and Affiliations
Consortia
Contributions
R. S., T. W., and S. P.: contributed equally to this work and shared the first authorship. R. S.: conceptualisation, methodology, investigation, formal analysis. T. W.: formal analysis, discussion of the results, writing — review and editing. S. P.: formal analysis, writing — original draft preparation. Y. R. and W. H.: discussion of the results, review and editing. B. M.: investigation, data curation. A. A. T.: conception, writing. Y. G.: manuscript writing, investigation, data curation. C. L.: investigation, data curation. K. M.: conceptualisation, methodology, writing — review and editing, supervision. All authors have seen the final manuscript and approved it.
Corresponding author
Ethics declarations
Ethics Approval
This project was registered as a multinational audit. Each site project lead was responsible for obtaining local governance approvals and data sharing agreements before entering data into the registry.
Statement of Human and Animal Rights
Not applicable.
Informed Consent
No informed consent was needed for an audit of this nature.
Conflict of Interest
A. A. T. reports grants from Novo Nordisk, personal fees from Novo Nordisk, non-financial support from Novo Nordisk, personal fees from Eli Lilly, non-financial support from Eli Lilly, personal fees from Janssen, personal fees from AZ, non-financial support from AZ, non-financial support from Impeto medical, non-financial support from Resmed, non-financial support from Aptiva, personal fees from BI, non-financial support from BI, personal fees from BMS, non-financial support from BMS, personal fees from NAPP, non-financial support from NAPP, personal fees from MSD, non-financial support from MSD, personal fees from Nestle, personal fees from Gilead, grants from Sanofi, and personal fees from Sanofi outside the submitted work. A. A. T. is currently an employee of Novo Nordisk. Novo Nordisk had no role in this project.
K. M. has been paid honoraria by various NHS trusts and Ethicon®, Medtronic®, Gore Inc®, and Olympus® for educational activities related to bariatric surgery.
Other authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
1) Smaller hospitals (< 200 beds) were able to restart their BMS sooner than larger ones (60.8 ± 38.9 days vs 81.3 ± 30.5 days).
2) Private practices were able to resume BMS sooner than government-funded practices (58.5 ± 38.3 days vs 97.1 ± 76.2 days).
3) Precautionary measures adopted included patient segregation, utilisation of personal protective equipment, and preoperative patients’ testing.
Supplementary Information
ESM 1
(PDF 63.9 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Singhal, R., Wiggins, T., Pouwels, S. et al. Handling of the Covid-19 Pandemic and Its Effects on Bariatric Surgical Practice: Analysis of GENEVA Study Database. OBES SURG 32, 3908–3921 (2022). https://doi.org/10.1007/s11695-022-06267-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06267-7