Abstract
Purpose
Early postoperative bleeding is a common complication after laparoscopic Roux-en-Y gastric bypass (LRYGB) and is associated with significant morbidity. We aimed to identify predictors of early postoperative bleeding after LRYGB and characterize hemorrhagic events and 30-day postoperative outcomes.
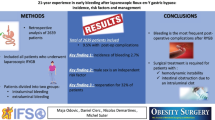
Material and Methods
We conducted a retrospective cohort study regarding all patients submitted to LRYGB in 2019 at a high-volume obesity center. Early postoperative bleeding was defined as any clinically significant evidence of hemorrhage in the early postoperative period. Demographic, preoperative, and intraoperative factors were evaluated for associations with postoperative bleeding. Postoperative outcomes were compared between patients with and without hemorrhage.
Results
Of 340 patients submitted to LRYGB, 14 (4.1%) had early postoperative bleeding. Patients with bleeding had an increased preoperative left hepatic lobe diameter (8.4 vs. 7.3 cm, p = 0.048). Prior cholecystectomy (28.6 vs. 14.5%) and previous bariatric surgery (35.7 vs. 23.9%) tended to be more prevalent among these patients. Bleeding occurred at a median time of 31.2 [IQR 19.7–38.5] h. Thirteen patients presented with intraluminal bleeding and one with extraluminal bleeding. Melena was the most common symptom. All hemorrhages were clinically diagnosed, and 92.9% were managed conservatively. Postoperative bleeding was associated with longer hospital stay (3.5 vs. 2.0 days), higher reintervention (7.1 vs. 0%), and readmission (14.3 vs. 0%), all p < 0.05.
Conclusions
Bleeding was the most frequent early complication after LRYGB. Patients with hepatomegaly and prior surgeries may have technically challenging LRYGB and should be carefully assessed. Perioperative strategies should be encouraged in high-risk patients to prevent bleeding.
Graphical abstract

Similar content being viewed by others
References
Welbourn R, Hollyman M, Kinsman R, Dixon J, Liem R, Ottosson J, et al. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the Fourth IFSO Global Registry Report 2018. Obes Surg. 2019;29(3):782–95.
Colquitt JL, Pickett K, Loveman E, Frampton GK. Surgery for weight loss in adults. Cochrane Database of Systematic Reviews. 2014(8).
Aminian A, Jamal MH, Andalib A, Batayyah E, Romero-Talamás H, Chand B, et al. Is laparoscopic bariatric surgery a safe option in extremely high-risk morbidly obese patients? J Laparoendosc Adv Surg Tech A. 2015;25(9):707–11.
Encinosa WE, Bernard DM, Du D, Steiner CA. Recent improvements in bariatric surgery outcomes. Med Care. 2009;47(5):531–5.
Dayer-Jankechova A, Fournier P, Allemann P, Suter M. Complications after laparoscopic Roux-en-Y gastric bypass in 1573 consecutive patients: are there predictors? Obes Surg. 2016;26(1):12–20.
Stenberg E, Szabo E, Agren G, Näslund E, Boman L, Bylund A, et al. Early complications after laparoscopic gastric bypass surgery: results from the Scandinavian Obesity Surgery Registry. Ann Surg. 2014;260(6):1040–7.
Rausa E, Bonavina L, Asti E, Gaeta M, Ricci C. Rate of death and complications in laparoscopic and open Roux-en-Y gastric bypass. A meta-analysis and meta-regression analysis on 69,494 patients. Obes Surg. 2016;26(8):1956–63.
Zafar SN, Miller K, Felton J, Wise ES, Kligman M. Postoperative bleeding after laparoscopic Roux en Y gastric bypass: predictors and consequences. Surg Endosc. 2019;33(1):272–80.
Brethauer SA, Kim J, el Chaar M, Papasavas P, Eisenberg D, Rogers A, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11(3):489–506.
Susmallian S, Danoch R, Raskin B, Raziel A, Barnea R, Dvora P. Assessing bleeding risk in bariatric surgeries: a retrospective analysis study. Dig Dis. 2020;38(6):449–57.
Dick A, Byrne TK, Baker M, Budak A, Morgan K. Gastrointestinal bleeding after gastric bypass surgery: nuisance or catastrophe? Surg Obes Relat Dis. 2010;6(6):643–7.
Bellorin O, Abdemur A, Sucandy I, Szomstein S, Rosenthal RJ. Understanding the significance, reasons and patterns of abnormal vital signs after gastric bypass for morbid obesity. Obes Surg. 2011;21(6):707–13.
Surgeons ACo. User guide for the 2019 ACS NSQIP participant use data file (PUF). 2020.
Surgeons ACo. User guide for the 2019 participant use data file (PUF). 2020.
Rabl C, Peeva S, Prado K, James AW, Rogers SJ, Posselt A, et al. Early and late abdominal bleeding after Roux-en-Y gastric bypass: sources and tailored therapeutic strategies. Obes Surg. 2011;21(4):413–20.
Perugini RA, Mason R, Czerniach DR, Novitsky YW, Baker S, Litwin DE, et al. Predictors of complication and suboptimal weight loss after laparoscopic Roux-en-Y gastric bypass: a series of 188 patients. Arch Surg. 2003;138(5):541–5 (discussion 5–6).
Gribsholt SB, Svensson E, Thomsen RW, Richelsen B, Sørensen HT. Preoperative glucocorticoid use and risk of postoperative bleeding and infection after gastric bypass surgery for the treatment of obesity. Surg Obes Relat Dis. 2015;11(6):1212–7.
Fecso AB, Samuel T, Elnahas A, Sockalingam S, Jackson T, Quereshy F, et al. Clinical indicators of postoperative bleeding in bariatric surgery. Surg Laparosc Endosc Percutan Tech. 2018;28(1):52–5.
Cohen JB, Tewksbury CM, Torres Landa S, Williams NN, Dumon KR. National postoperative bariatric surgery outcomes in patients with chronic kidney disease and end-stage kidney disease. Obes Surg. 2019;29(3):975–82.
Jalal DI, Chonchol M, Targher G. Disorders of hemostasis associated with chronic kidney disease. Semin Thromb Hemost. 2010;36(1):34–40.
Midya S, Ramus J, Hakim A, Jones G, Sampson M. Comparison of two types of liver retractors in laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg. 2020;30(1):233–7.
Heneghan HM, Meron-Eldar S, Yenumula P, Rogula T, Brethauer SA, Schauer PR. Incidence and management of bleeding complications after gastric bypass surgery in the morbidly obese. Surg Obes Relat Dis. 2012;8(6):729–35.
García-García ML, Martín-Lorenzo JG, Torralba-Martínez JA, Lirón-Ruiz R, Miguel Perelló J, Flores Pastor B, et al. Emergency endoscopy for gastrointestinal bleeding after bariatric surgery. Therapeutic algorithm Cir Esp. 2015;93(2):97–104.
Nguyen NT, Longoria M, Welbourne S, Sabio A, Wilson SE. Glycolide copolymer staple-line reinforcement reduces staple site bleeding during laparoscopic gastric bypass: a prospective randomized trial. Arch Surg. 2005;140(8):773–8.
Acknowledgements
The authors would like to acknowledge all members of the Obesity Integrated Responsibility Unit (CRI-O) group.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
This study was approved by the Health Ethics Committee of our hospital (deliberation no. 46/2021).
Informed Consent
Informed consent does not apply.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Bleeding was the most frequent complication after LRYGB, with an incidence of 4.1%.
• Patients with bleeding had an increased preoperative left hepatic lobe diameter.
• Bleeding was conservatively managed in 92.9% of the patients.
• Bleeding resulted in longer hospital stay, higher reintervention, and readmission.
Rights and permissions
About this article
Cite this article
Pereira, A., Santos, R.F., Costa-Pinho, A. et al. Early Postoperative Bleeding After Laparoscopic Roux-En-Y Gastric Bypass: a Single Center Analysis. OBES SURG 32, 1902–1908 (2022). https://doi.org/10.1007/s11695-022-05973-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-05973-6