Abstract
Purpose
Secondary hyperparathyroidism (SHPT) is linked to obesity. Bariatric surgery may be associated with calcium and vitamin D deficiencies leading to SHPT. This study aimed to detect the prevalence of SHPT before and after bariatric surgery.
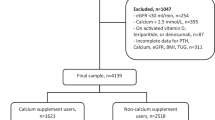
Methods
This prospective study assessed the prevalence of SHPT after sleeve gastrectomy (SG, n = 38) compared to one-anastomosis gastric bypass (OAGB, n = 86). All patients were followed up for 2 years. Bone mineral density (BMD) was assessed using dual-energy X-ray absorptiometry.
Results
Of the 124 patients, 71 (57.3%) were females, and 53 (42.7%) were males, with a mean age of 37.5 ± 8.8 years. Before surgery, 23 patients (18.5%) suffered from SHPT, and 40 (32.3%) had vitamin D deficiency. The prevalence of SHPT increased to 29.8% after 1 year and 36.3% after 2 years. SHPT was associated with lower levels of vitamin D and calcium and higher reduction of BMD in the hip but not in the spine. After 2 years, SHPT was associated with a significantly lower T-score in the hip. SHPT and vitamin D deficiency were significantly more common in patients subjected to OAGB compared to SG (p = 0.003, and p < 0.001, respectively). There is a strong negative correlation between vitamin D levels and parathormone levels before and after surgery.
Conclusion
Prevalence of SHPT is high in obese patients seeking bariatric surgery, especially with lower vitamin D levels. Bariatric surgery increases the prevalence of SHPT up to 2 years. Gastric bypass is associated with a higher risk of developing SHPT compared to SG.
Graphical abstract

Similar content being viewed by others
References
Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15:288–98
Aboulghate M, Elaghoury A, Elebrashy I, Elkafrawy N, Elshishiney G, Abul-Magd E, et al. The burden of obesity in Egypt. Front Public Health. 2021;9:1247
Bray GA, Kim KK, Wilding JPH. World obesity federation. Obesity: a chronic relapsing progressive disease process. A position statement of the world obesity federation. Obes Rev. 2017;18:715–23
Saab G, Whaley-Connell A, McFarlane SI, Li S, Chen S-C, Sowers JR, et al. Obesity is associated with increased parathyroid hormone levels independent of glomerular filtration rate in chronic kidney disease. Metabolism. 2010;59:385–9
Goldner WS, Stoner JA, Thompson J, Taylor K, Larson L, Erickson J, et al. Prevalence of vitamin D insufficiency and deficiency in morbidly obese patients: a comparison with non-obese controls. Obes Surg. 2008;18:145–50
Rodríguez-Rodríguez E, Navia B, López-Sobaler AM, Ortega RM. Vitamin D in overweight/obese women and its relationship with dietetic and anthropometric variables. Obesity. 2009;17:778–82
Guasch A, Bulló M, Rabassa A, Bonada A, Del Castillo D, Sabench F, et al. Plasma vitamin D and parathormone are associated with obesity and atherogenic dyslipidemia: a cross-sectional study. Cardiovasc Diabetol. 2012;11:149
Wiggins T, Guidozzi N, Welbourn R, Ahmed AR, Markar SR. Association of bariatric surgery with all-cause mortality and incidence of obesity-related disease at a population level: a systematic review and meta-analysis. PLoS Med. 2020;17:e1003206
O’Brien PE, Hindle A, Brennan L, Skinner S, Burton P, Smith A, et al. Long-term outcomes after bariatric surgery: a systematic review and meta-analysis of weight loss at 10 or more years for all bariatric procedures and a single-Centre review of 20-year outcomes after adjustable gastric banding. Obes Surg. 2019;29:3–14
Suthakaran R, Indigahawela I, Mori K, Lim K, Aly A. Preventing calcium and vitamin D deficiencies following weight loss and metabolic surgery. BMC Surg. 2021;21:351
Rousseau C, Jean S, Gamache P, Lebel S, Mac-Way F, Biertho L, et al. Change in fracture risk and fracture pattern after bariatric surgery: nested case-control study. BMJ. British Medical Journal Publishing Group; 2016;354:i3794.
Holick MF. Vitamin D status: measurement, interpretation and clinical application. Ann Epidemiol. 2009;19:73–8
Nissenson RA, Jüppner H. Parathyroid hormone. Primer on the metabolic bone diseases and disorders of mineral metabolism [Internet]. John Wiley & Sons, Ltd; [cited 2021 Sep 30]. p. 208–14. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/9781118453926.ch26
Cunningham J, Locatelli F, Rodriguez M. Secondary hyperparathyroidism: pathogenesis, disease progression, and therapeutic options. CJASN Am Soc Nephrol. 2011;6:913–21
Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ, Khaltaev N. A reference standard for the description of osteoporosis. Bone. 2008;42:467–75
Wei J-H, Lee W-J, Chong K, Lee Y-C, Chen S-C, Huang P-H, et al. High incidence of secondary hyperparathyroidism in bariatric patients: comparing different procedures. Obes Surg. 2018;28:798–804
Mendonça FM, Neves JS, Silva MM, Borges-Canha M, Costa C, Cabral PM, et al. Secondary hyperparathyroidism among bariatric patients: unraveling the prevalence of an overlooked foe. Obes Surg. 2021;31:3768–75
Alejo Ramos M, Cano Rodríguez IM, Urioste Fondo AM, Pintor de la Maza B, Barajas Galindo DE, Fernández Martínez P, et al. Secondary hyperparathyroidism in patients with biliopancreatic diversion after 10 years of follow-up, and relationship with vitamin D and serum calcium. Obes Surg. 2019;29:999–1006
Cheng S, Massaro JM, Fox CS, Larson MG, Keyes MJ, McCabe EL, et al. Adiposity, cardiometabolic risk, and vitamin D status: the Framingham heart study. Diabetes. 2010;59:242–8
Yetley EA. Assessing the vitamin D status of the US population. Am J Clin Nutr. 2008;88:558S–64S
Mousa A, Naderpoor N, de Courten MPJ, Scragg R, de Courten B. 25-hydroxyvitamin D is associated with adiposity and cardiometabolic risk factors in a predominantly vitamin D-deficient and overweight/obese but otherwise healthy cohort. J Steroid Biochem Mol Biol. 2017;173:258–64
Karuppusami R, Antonisami B, Vasan SK, Gowri M, Selliah HY, Arulappan G, et al. Association of serum 25-hydroxy vitamin D with total and regional adiposity and cardiometabolic traits. PLOS ONE. Public library of Science; 2020;15:e0243850.
Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000;72:690–3
Drincic AT, Armas LAG, Van Diest EE, Heaney RP. Volumetric dilution, rather than sequestration best explains the low vitamin D status of obesity. Obesity (Silver Spring). 2012;20:1444–8
Wamberg L, Christiansen T, Paulsen SK, Fisker S, Rask P, Rejnmark L, et al. Expression of vitamin D-metabolizing enzymes in human adipose tissue -- the effect of obesity and diet-induced weight loss. Int J Obes 2013;37:651–657.
Peterson LA. Bariatric surgery and vitamin D: key messages for surgeons and clinicians before and after bariatric surgery. Minerva Chir. 2016;71:322–36
Chakhtoura M, Nakhoul N, Shawwa K, Mantzoros C, El Hajj FG. Hypovitaminosis D in bariatric surgery: a systematic review of observational studies. Metabolism. 2016;65:574–85
Dogan K, Homan J, Aarts EO, de Boer H, van Laarhoven CJHM, Berends FJ. Long-term nutritional status in patients following roux-en-Y gastric bypass surgery. Clin Nutr. 2018;37:612–7
Arias PM, Domeniconi EA, García M, Esquivel CM, Martínez Lascano F, Foscarini JM. Micronutrient deficiencies after roux-en-Y gastric bypass: long-term results. Obes Surg. 2020;30:169–73
Schafer AL, Weaver CM, Black DM, Wheeler AL, Chang H, Szefc GV, et al. Intestinal calcium absorption decreases dramatically after gastric bypass surgery despite optimization of vitamin D status. J Bone Miner Res. 2015;30:1377–85
Carrasco F, Basfi-fer K, Rojas P, Csendes A, Papapietro K, Codoceo J, et al. Calcium absorption may be affected after either sleeve gastrectomy or roux-en-Y gastric bypass in premenopausal women: a 2-y prospective study. Am J Clin Nutr. 2018;108:24–32
Braghetto I, Davanzo C, Korn O, Csendes A, Valladares H, Herrera E, et al. Scintigraphic evaluation of gastric emptying in obese patients submitted to sleeve gastrectomy compared to normal subjects. Obes Surg. 2009;19:1515–21
Schafer AL. Vitamin D and intestinal calcium transport after bariatric surgery. J Steroid Biochem Mol Biol. 2017;173:202–10
Fleet JC, Schoch RD. Molecular mechanisms for regulation of intestinal calcium absorption by vitamin D and other factors. Crit Rev Clin Lab Sci. 2010;47:181–95
Altawil E, Alkofide H, Alamri H, Alhassan N, Alsubaie H, Alqahtani A, et al. Secondary hyperparathyroidism in obese patients post sleeve gastrectomy. DMSO Dove Press. 2021;14:4059–66
Jalali SM, Azadbakht M, Azadbakht S, Daniali S, Farokhi E. Prevalence of secondary hyperparathyroidism following bariatric surgery. International Journal of Surgery Open. 2020;27:214–9
Jaruvongvanich V, Vantanasiri K, Upala S, Ungprasert P. Changes in bone mineral density and bone metabolism after sleeve gastrectomy: a systematic review and meta-analysis. Surg Obes Relat Dis. 2019;15:1252–60
Liu C, Wu D, Zhang J-F, Xu D, Xu W-F, Chen Y, et al. Changes in bone metabolism in morbidly obese patients after bariatric surgery: a meta-analysis. Obes Surg. 2016;26:91–7
de Holanda NCP, Baad VMA, Bezerra LR, de Lima SKM, Filho JM, de Holanda Limeira CC, et al. Secondary hyperparathyroidism, bone density, and bone turnover after bariatric surgery: differences between roux-en-Y gastric bypass and sleeve gastrectomy. Obes Surg. 2021;
Maghrabi AH, Wolski K, Abood B, Licata A, Pothier C, Bhatt DL, et al. Two-year outcomes on bone density and fracture incidence in patients with T2DM randomized to bariatric surgery versus intensive medical therapy. Obesity (Silver Spring). 2015;23:2344–8
Blom-Høgestøl IK, Hewitt S, Chahal-Kummen M, Brunborg C, Gulseth HL, Kristinsson JA, et al. Bone metabolism, bone mineral density and low-energy fractures 10 years after roux-en-Y gastric bypass. Bone. 2019;127:436–45
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All performed procedures were in accordance with the ethical standards of the institutional research committee and with the Helsinki declaration.
Informed Consent
Informed consent was obtained from all patients included in this study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Prevalence of SHPT is high in obese patients seeking bariatric surgery.
• Bariatric surgery increases the prevalence of SHPT up to 2 years.
• Gastric bypass is associated with a higher risk of developing SHPT compared to SG.
Rights and permissions
About this article
Cite this article
Salman, M.A., Salman, A., Elewa, A. et al. Secondary Hyperparathyroidism Before and After Bariatric Surgery: a Prospective Study with 2-Year Follow-Up. OBES SURG 32, 1141–1148 (2022). https://doi.org/10.1007/s11695-022-05902-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-05902-7