Abstract
Purpose
Beginning January 1, 2005, bariatric surgery cases were examined with the help of the quality assurance study for operative medicine. All data were registered and analyzed prospectively in cooperation with the Institute of Quality Assurance in Surgery at the Otto-von-Guericke University Magdeburg, Germany. The comparative study focuses on perioperative morbidity, complications, and remission of obesity-associated diseases after gastric bypass (RYGB) and sleeve gastrectomy (SG) at 5-year follow-up.
Materials and Methods
Data collection includes patients of full age who underwent SG or RYGB surgery between 2005 and 2017. The bougie is limited to 33–40 French for SG. The Roux-en-Y length for RYGB is set to 120–180 cm, and the biliodigestive length is set to 40–60 cm. Outcome criteria are perioperative morbidity, postoperative and intraoperative complications, and remission on comorbidities.
Results
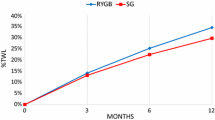
Between 2005 and 2017, 64,349 patients were enrolled in German Bariatric Surgery Registry (GBSR). Primary operations that were performed were 56.328. Out of 24,146 RYGB and 24,085 SG procedures, 922 patients had a complete 5-year follow-up. These are 342 SG patients and 580 patients with RYGB. A matching was realized for n = 285 (83.3%) patient pairs based on age, BMI, gender, ASA, and comorbidities. A significant disadvantage was identified for the SG procedure regarding reflux disease compared with RYGB (36.3% vs. 8.10%; p < 0.001). There were no significant disadvantages in terms of BMI reduction [14.92 in the RYGB and 14.50 in the SG (p = 0.437)] and %EWL [60.32 in the RYGB and 58.98 in the SG (p = 0.504)]. This also applies to the remission of NIDDM, IDDM, hypertension, and sleep apnea; no significant differences were found.
Conclusion
The results of the study show significant findings for gastroesophageal reflux. In terms of complications and obesity-associated diseases, no significant disadvantages between both treatments were found. RYGB and SG had comparable postoperative morbidity rates. The two surgical methods are legitimate bariatric procedures. However, there is a need for further evaluation to optimize patient selection in the coming years.
Graphical abstract

Similar content being viewed by others
References
Yumuk V, Tsigos C, Fried M et al. Obesity Management Task Force of the European Association for the Study of Obesity. European Guidelines for Obesity Management in Adults. Obes Facts. 2015;8(6):402-24. Erratum in: Obes Facts. 2016;9(1):64. https://doi.org/10.1159/000442721.
Rohana N. Haththotuwa, Chandrika N. Wijeyaratne, Upul Senarath. ‘Chapter 1 - worldwide epidemic of obesity’, in Obesity and Obstetrics (Second Edition), ed. Tahir A. Mahmood, Sabaratnam Arulkumaran, and Frank A. Chervenak (Elsevier), 2020; 3–8, https://doi.org/10.1016/B978-0-12-817921-5.00001-1.
Nuertey BD, Alhassan AI, Nuertey AD, et al. Prevalence of obesity and overweight and its associated factors among registered pensioners in Ghana; a Cross Sectional Studies. BMC Obes. 2017;4:26. https://doi.org/10.1186/S40608-017-0162-4.
Christou NV, Sampalis JS, Liberman M et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg. 2004; 240(3):416-23; Discussion 423-4. https://doi.org/10.1097/01.Sla.0000137343.63376.19.
Al-Goblan AS, Al-Alfi MA, Khan MZ. Mechanism linking diabetes mellitus and obesity. Diabetes Metab Syndr Obes. 2014;7:587–91. https://doi.org/10.2147/DMSO.S67400.
Coroyannakis C, Khalil A. Management of hypertension in the obese pregnant patient. Curr Hypertens Rep. 2019;21(3):24. https://doi.org/10.1007/S11906-019-0927-x.
Wang Y, Shirore RM, Ramakrishnan C, et al. Adiposity measures and pre-diabetes or diabetes in adults with hypertension in Singapore Polyclinics. J Clin Hypertens (Greenwich). 2019;21(7):953–62. https://doi.org/10.1111/Jch.13587.
Fock KM, Khoo J. Diet and exercise in management of obesity and overweight. J Gastroenterol Hepatol. 2013;28(Suppl 4):59–63. https://doi.org/10.1111/Jgh.12407.
Maciejewski ML, Arterburn DE, Van Scoyoc L, et al. Bariatric surgery and long-term durability of weight loss. JAMA Surg. 2016;151(11):1046–55. https://doi.org/10.1001/Jamasurg.2016.2317.
Hutter MM, Schirmer BD, Jones DB et al. First Report from the American College of Surgeons Bariatric Surgery Center Network: Laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann Surg. 2011; 254(3):410-20; Discussion 420-2. https://doi.org/10.1097/SLA.0b013e31822c9dac.
Cunha J.B. Da, Fialho MCP, deM Arruda SL, et al. Bariatric surgery as a safe and effective intervention for the control of comorbidities in older adults. Geriatrics, Gerontology and Aging. 2020;14:207–12.
Peterli R, Wölnerhanssen BK, Peters TM, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-En-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA. 2018;319(3):255–65. https://doi.org/10.1001/Jama.2017.20897.
Chung AY, Thompson R, Overby DWM, et al. Sleeve gastrectomy: surgical tips. J Laparoendosc Adv Surg Tech A. 2018;28(8):930–7. https://doi.org/10.1089/Lap.2018.0392.
Buchwald H, Williams SE. Bariatric Surgery Worldwide 2003. Obes Surg. 2004;14(9):1157–64. https://doi.org/10.1381/0960892042387057.
McGlone ER, Carey I, Veličković V, et al. Bariatric surgery for patients with type 2 diabetes mellitus requiring insulin: clinical outcome and cost-effectiveness Analyses. PLoS Med. 2020;17(12):E1003228. https://doi.org/10.1371/Journal.
Colquitt JL, Pickett K, Loveman E, et al. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014;8(8):CD003641. https://doi.org/10.1002/14651858.CD003641.
Buchwald H, Avidor Y, Braunwald E et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004; 292(14):1724–37. Erratum in: JAMA. 2005 Apr 13;293(14):1728. https://doi.org/10.1001/Jama.292.14.1724.
Gloy VL, Briel M, Bhatt DL, et al. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJ. 2013;347:F5934. https://doi.org/10.1136/Bmj.F5934.
Stone TW, McPherson M, Gail DL. Obesity and cancer: existing and new hypotheses for a causal connection. EBioMedicine. 2018;30:14–28. https://doi.org/10.1016/j.Ebiom.2018.02.022.
Kuk JL, Ardern CI. Are metabolically normal but obese individuals at lower risk for all-cause mortality? Diabetes Care. 2009;32(12):2297–9. https://doi.org/10.2337/Dc09-0574.
Flegal KM, Kit BK, Orpana H, et al. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82. https://doi.org/10.1001/Jama.2012.113905.
O'Brien P. Surgical Treatment of Obesity. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dhatariya K, Dungan K, Grossman A, Hershman JM, Hofland J, Kalra S, Kaltsas G, Koch C, Kopp P, Korbonits M, Kovacs CS, Kuohung W, Laferrère B, McGee EA, McLachlan R, Morley JE, New M, Purnell J, Sahay R, Singer F, Stratakis CA, Trence DL, Wilson DP, editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc. 2016; 2000
Stroh C, Weiner R, Wolff S, et al. Obesity Surgery Working Group and Competence Network Obesity. Are There gender-specific aspects in obesity and metabolic surgery? Data Analysis from the German Bariatric Surgery Registry. Viszeralmedizin. 2014;30(2):125–32. https://doi.org/10.1159/000360148.
Young MT, Phelan MJ, Nguyen NT. A decade analysis of trends and outcomes of male vs female patients who underwent bariatric surgery. J Am Coll Surg. 2016;222(3):226–31. https://doi.org/10.1016/j.Jamcollsurg.2015.11.033.
Tymitz K, Kerlakian G, Engel A, et al. Gender differences in early outcomes following hand-assisted laparoscopic Roux-en-Y gastric bypass surgery : gender differences in bariatric surgery. Obes Surg. 2007;17(12):1588–91. https://doi.org/10.1007/s11695-007-9296-7.
Varela JE, Wilson SE, Nguyen NT. Outcomes of bariatric surgery in the elderly. Am Surg. 2006;72(10):865–9. https://doi.org/10.1177/000313480607201005.
Thaher O, Wolf S, Hukauf M et al. Propensity Score-matching sleeve gastrectomy (SG) vs. gastric bypass (RYGB) in patients ≥ 60 years. Obes Surg. 2021. https://doi.org/10.1007/S11695-021-05320-1.
Dorman RB, Abraham AA, Al-Refaie WB et al. Bariatric Surgery outcomes in the elderly: an ACS NSQIP study. J Gastrointest Surg. 2012; 16(1):35-44; Discussion 44. https://doi.org/10.1007/S11605-011-1749-6.
Giordano S, Victorzon M. Bariatric surgery in elderly patients: a systematic review. Clin Interv Aging. 2015;10:1627–35. https://doi.org/10.2147/CIA.S70313.
Cunha J.B. Da, Fialho M.C.P., de Arruda S.L.M et al. Bariatric surgery as a safe and effective intervention for the control of comorbidities in older adults. Geriatrics, Gerontology and Aging. 2020; 14, 207–212.’
Sjöström L, Peltonen M, Jacobson P, et al. Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascular and macrovascular complications. JAMA. 2014;311(22):2297–304. https://doi.org/10.1001/Jama.2014.5988.
Melissas J, Stavroulakis K, Tzikoulis V, et al. Sleeve gastrectomy vs Roux-En-Y gastric bypass. Data from IFSO-European Chapter Center of Excellence Program. Obesity Surgery. 2017;27(4):847–55.
Lager CJ, Esfandiari NH, Luo Y, et al. Oral EA: metabolic parameters, weight loss, and comorbidities 4 years after Roux-En-Y Gastric bypass and sleeve gastrectomy. Obes Surg. 2018;28(11):3415–23.
Jiménez A, Ibarzabal A, Moizé V, et al. Ten-year outcomes after Roux-En-Y gastric bypass and sleeve gastrectomy: an observational nonrandomized cohort study. Surg Obes Relat Dis. 2019;15(3):382–8. https://doi.org/10.1016/j.Soard.2019.01.020.
Ma IT, Madura JA 2nd. Gastrointestinal complications after bariatric surgery. Gastroenterol Hepatol (N Y). 2015;11(8):526–35.
Monkhouse SJ, Morgan JD, Norton SA. Complications of bariatric surgery: presentation and emergency management–a review. Ann R Coll Surg Engl. 2009;91(4):280–6. https://doi.org/10.1308/003588409X392072.
Herron DM, Bloomberg R. Complications of bariatric surgery. Minerva Chir. 2006;61(2):125–39.
Caceres BA, Moskowitz D, O’Connell T. A review of the safety and efficacy of bariatric surgery in adults over the age of 60: 2002–2013. J Am Assoc Nurse Pract. 2015;27(7):403–10. https://doi.org/10.1002/2327-6924.12235.
Husain F, Jeong IH, Spight D, et al. Risk Factors for early postoperative complications after bariatric surgery. Ann Surg Treat Res. 2018;95(2):100–10.
Weiner S, Heidsieck T, Chiappetta S, et al. Anastomosis and suture insufficiency after interventions for bariatric and metabolic surgery. Chirurg. 2015;86(9):824–32.
Casella G, Soricelli E, Giannotti D, et al. Learning curve for laparoscopic sleeve gastrectomy: role of training in a high-volume bariatric center. Surg Endosc. 2016;30(9):3741–8.
Ricci C, Gaeta M, Rausa E, et al. Long-term effects of bariatric surgery on type II diabetes, hypertension and hyperlipidemia: a meta-analysis and meta-regression study with 5-year follow-up. Obes Surg. 2015;25(3):397–405.
Mizera M, Wysocki M, Bartosiak K, et al. Type 2 diabetes remission 5 years after laparoscopic sleeve gastrectomy: multicenter cohort study. Obes Surg. 2021;31:980–6. https://doi.org/10.1007/S11695-020-05088-w.
Seki Y, Kasama K, Haruta H, et al. Five-year-results of laparoscopic sleeve gastrectomy with duodenojejunal bypass for weight loss and type 2 diabetes mellitus. Obes Surg. 2017;27(3):795–801. https://doi.org/10.1007/S11695-016-2372-0.
Toh BC, Chan WH, Eng AKH, et al. Five-year long-term clinical outcome after bariatric metabolic surgery: a multi-ethnic asian population in Singapore. Diabetes Obes Metab. 2018;20(7):1762–5. https://doi.org/10.1111/Dom.13263.
Stamler R, Stamler J, Riedlinger WF, et al. Weight and blood pressure. Findings in hypertension screening of 1 million Americans. JAMA. 1978;240(15):1607–10. https://doi.org/10.1001/Jama.240.15.1607.
Wilhelm SM, Young J, Kale-Pradhan PB. Effect of Bariatric surgery on hypertension: a meta-analysis. Ann Pharmacother. 2014;48(6):674–82. https://doi.org/10.1177/1060028014529260.
Pareek M, Schauer PR, Kaplan LM, et al. Metabolic Surgery: Weight Loss, Diabetes, and Beyond. J Am Coll Cardiol. 2018;71(6):670–87. https://doi.org/10.1016/j.Jacc.2017.12.014.
Antono C. Valezi, Fernando A.M. Herbella, Francisco Schlottmann et al. Journal of Laparoendoscopic & Advanced Surgical Techniques.Aug 2018; .949–952. https://doi.org/10.1089/Lap.2018.0395.
Himpens J, Dobbeleir J, Peeters G. Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann Surg. 2010;252(2):319–24.
DuPree CE, Blair K, Steele SR, et al. Laparoscopic sleeve gastrectomy in patients with preexisting gastroesophageal reflux disease: a national analysis. JAMA. 2014;149(4):328–34.
Rundo JV. Obstructive sleep apnea basics. Cleve Clin J Med. 2019;86(9 Suppl 1):2–9. https://doi.org/10.3949/ccjm.86.s1.02.
Frey WC, Pilcher J. Obstructive sleep-related breathing disorders in patients evaluated for bariatric surgery. Obes Surg. 2003;13(5):676–83. https://doi.org/10.1381/096089203322509228.
Drager LF, Togeiro SM, Polotsky VY, et al. Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol. 2013;62(7):569–76. https://doi.org/10.1016/j.jacc.2013.05.045.
Romero-Corral A, Caples SM, Lopez-Jimenez F, et al. Interactions between obesity and obstructive sleep apnea: implications for treatment. Chest. 2010;137(3):711–9. https://doi.org/10.1378/Chest.09-0360.
Lopez PP, Stefan B, Schulman CI, et al. Prevalence of sleep apnea in morbidly obese patients who presented for weight loss surgery evaluation: more evidence for routine screening for obstructive sleep apnea before weight loss surgery. Am Surg. 2008;74(9):834–8.
Acknowledgements
We would like to thank Mr. Hukauf for his contributions to the statistical analysis of our data. We thank all hospitals participating in the study for their active engagement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
For this type of retrospective study, no formal consent was required. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Sleeve gastrectomy and gastric bypass achieved identical results in terms of peri- and postoperative complications.
• Reflux within 5 years after surgery was four times higher after SG than after RYGB.
• No significant difference between SG and RYGB in terms of remission of obesity-associated diseases
Rights and permissions
About this article
Cite this article
Thaher, O., Hukauf, M. & Stroh, C. Propensity Score Matching Sleeve Gastrectomy vs. Gastric Bypass with 5 Years of Follow-Up. OBES SURG 31, 5156–5165 (2021). https://doi.org/10.1007/s11695-021-05706-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05706-1



