Abstract
Background
Studies investigating the underlying pathophysiology are needed to help explain and understand the postoperative complications following Roux-en-Y gastric bypass (RYGB) surgery. This study aimed to characterize segmental gastrointestinal pH profiles, motility measures, and transit times in patients with RYGB.
Materials and Methods
Nineteen patients with RYGB underwent a standardized wireless motility capsule assessment. The oro-cecal segment was defined from capsule ingestion until the passage of the ileocecal junction. Segmental median pH, motility index, and transit time were determined for the oro-cecal and colonic segment as well as for the first and last hour of both these segments. For comparison to reference values, data from 17 healthy age- and gender-matched controls was used. A mixed effect model was used to describe differences between groups.
Results
Median pH was high in patients with RYGB during the first hour of the oro-cecal segment (6.45 ± 0.4 vs 3.65 ± 1.55 pH units for healthy controls; P < 0.001), as well as during the entire oro-cecal segment (6.97 ± 0.4 vs 5.51 ± 1.1 pH units; P < 0.001). The same was evident for the median motility index (152 ± 64 vs 35.8 ± 31.1 mmHg*sec/min; P < 0.001 and 130 ± 65.9 vs 89.1 ± 20 mmHg*sec/min; P < 0.012, respectively). Median motility index was low the first hour of the colon (55.2 ± 45.7 vs 122 ± 77.9 mmHg*sec/min; P < 0.002). Additionally, patients had short oro-cecal transit time (5.8 ± 1.6 vs 7.6 ± 1.4 h; P < 0.001) and long colonic transit time (29.4 ± 17.5 vs 19.6 ± 12.2 h; P = 0.048).
Conclusions
In patients with RYGB, the oro-cecal segment was characterized by an alkaline intraluminal environment, high motility activity, and short transit time. In contrast, colonic transit time was long.
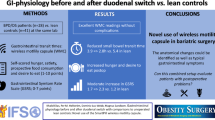
Graphical abstract


Similar content being viewed by others
References
Tremmel M, Gerdtham U-G, Nilsson P, et al. Economic burden of obesity: a systematic literature review. Int J Environ Res Public Health. 2017;14:435.
World Health Organization. Obesity and overweight. 2018 [cited 2019 Aug 22]. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 22 Aug 2020.
Sundhedsstyrelsen. National Klinisk Retningslinje for fedmekirurgi. Vol. 150, InPharma. 2013 [cited 2019 Apr 10]. 9–10 p. Available from: http://www.sst.dk. Accessed 10 April 2020.
Carlsson LMS, Sjöholm K, Jacobson P, et al. Life expectancy after bariatric surgery in the Swedish obese subjects study. N Engl J Med. 2020;383:1535–43.
Dimitriadis GK, Randeva MS, Miras AD. Potential hormone mechanisms of bariatric surgery. Curr Obes Rep. 2017;6:253–65.
Seeras K, Lopez PP. Roux-en-Y gastric bypass chronic complications. StatPearls. 2019 [cited 2019 Jul 16];Available from: http://www.ncbi.nlm.nih.gov/pubmed/30137773. Accessed 16 July 2020.
Angeles PC, Robertsen I, Seeberg LT, et al. The influence of bariatric surgery on oral drug bioavailability in patients with obesity: a systematic review. Obes Rev. 2019;20:1299–311.
Hedberg J, Hedenström H, Sundbom M. Wireless pH-metry at the gastrojejunostomy after Roux-en-Y gastric bypass: a novel use of the BRAVO™ system. Surg Endosc. 2011;25:2302–7.
Hedberg J, Hedenström H, Nilsson S, et al. Role of gastric acid in stomal ulcer after gastric bypass. Obes Surg. 2005;15:1375–8.
Mason EE, Munns JR, Kealey GP, et al. Effect of gastric bypass on gastric secretion. Surg Obes Relat Dis. 2005;1:155–60.
Dirksen C, Damgaard M, Bojsen-Møller KN, et al. Fast pouch emptying, delayed small intestinal transit, and exaggerated gut hormone responses after Roux-en-Y gastric bypass. Neurogastroenterol Motil. 2013;25:346–e255.
Nguyen NQ, Debreceni TL, Burgstad CM, et al. Effects of fat and protein preloads on pouch emptying, intestinal transit, glycaemia, gut hormones, glucose absorption, blood pressure and gastrointestinal symptoms after Roux-en-Y gastric bypass. Obes Surg. 2016;26:77–84.
Carswell KA, Vincent RP, Belgaumkar AP, et al. The effect of bariatric surgery on intestinal absorption and transit time. Obes Surg. 2014;24:796–805.
Wang G, Agenor K, Pizot J, et al. Accelerated gastric emptying but no carbohydrate malabsorption 1 year after gastric bypass surgery (GBP). Obes Surg. 2012;22:1263–7.
Morínigo R, Moizé V, Musri M, et al. Glucagon-Like Peptide-1, Peptide YY, hunger, and satiety after gastric bypass surgery in morbidly obese subjects. J Clin Endocrinol Metab. 2006;91:1735–40.
Falkén Y, Hellström PM, Holst JJ, et al. Changes in glucose homeostasis after Roux-en-Y gastric bypass surgery for obesity at day three, two months, and one year after surgery: role of gut peptides. J Clin Endocrinol Metab. 2011;96:2227–35.
Sarosiek I, Selover KH, Katz LA, et al. The assessment of regional gut transit times in healthy controls and patients with gastroparesis using wireless motility technology. Aliment Pharmacol Ther. 2010;31:313–22.
Wang YT, Mohammed SD, Farmer AD, et al. Regional gastrointestinal transit and pH studied in 215 healthy volunteers using the wireless motility capsule: influence of age, gender, study country and testing protocol. Aliment Pharmacol Ther. 2015;42:761–72.
Farmer AD, Pedersen AG, Brock B, et al. Type 1 diabetic patients with peripheral neuropathy have pan-enteric prolongation of gastrointestinal transit times and an altered caecal pH profile. Diabetologia. 2017;60:709–18.
Farmer AD, Wegeberg A-ML, Brock B, et al. Regional gastrointestinal contractility parameters using the wireless motility capsule: inter-observer reproducibility and influence of age, gender and study country. Aliment Pharmacol Ther. 2018;47:391–400.
Portney LG, Watkins MP. Foundations of clinical research: applications to practice. 3rd ed. Pearson/Prentice Hall: Upper Saddle River; 2009.
Abuhelwa AY, Williams DB, Upton RN, et al. Food, gastrointestinal pH, and models of oral drug absorption. Eur J Pharm Biopharm. 2017;112:234–48.
Berg P, McCallum R. Dumping syndrome: a review of the current concepts of pathophysiology, diagnosis, and treatment. Dig Dis Sci. 2016;61:11–8.
Megan D. What is hypochlorhydria. Healthline Media. 2018 [cited 2019 Oct 2]. Available from: https://www.healthline.com/health/hypochlorhydria. Accessed 2 Oct 2020.
Camilleri M, Malagelada J-R. Abnormal intestinal motility in diabetics with the gastroparesis syndrome. Eur J Clin Investig. 1984;14:420–7.
Faria M, Pavin EJ, Parisi MCR, et al. Delayed small intestinal transit in patients with long-standing type 1 diabetes mellitus: investigation of the relationships with clinical features, gastric emptying, psychological distress, and nutritional parameters. Diabetes Technol Ther. 2013;15:32–8.
Nguyen NQ, Debreceni TL, Burgstad CM, et al. Effects of posture and meal volume on gastric emptying, intestinal transit, oral glucose tolerance, blood pressure and gastrointestinal symptoms after Roux-en-Y gastric bypass. Obes Surg. 2015;25:1392–400.
Näslund I, Beckman K-W. Gastric emptying rate after gastric bypass and gastroplasty. Scand J Gastroenterol. 1987;22:193–201.
Jacobsen SH, Bojsen-Møller KN, Dirksen C, et al. Effects of gastric bypass surgery on glucose absorption and metabolism during a mixed meal in glucose-tolerant individuals. Diabetologia. 2013;56:2250–4.
Martinussen C, Bojsen-Møller KN, Dirksen C, et al. Augmented GLP-1 secretion as seen after gastric bypass may be obtained by delaying carbohydrate digestion. J Clin Endocrinol Metab. 2019;104:3233–44.
Bojsen-Møller KN, Jacobsen SH, Dirksen C, et al. Accelerated protein digestion and amino acid absorption after Roux-en-Y gastric bypass. Am J Clin Nutr. 2015;102:600–7.
Farmer AD, Mohammed SD, Dukes GE, et al. Caecal pH is a biomarker of excessive colonic fermentation. World J Gastroenterol. 2014;20:5000–7.
Hasler WL, Saad RJ, Rao SS, et al. Heightened colon motor activity measured by a wireless capsule in patients with constipation: relation to colon transit and IBS. Am J Physiol Gastrointest Liver Physiol. 2009;297:G1107–14.
Poulsen JL, Nilsson M, Brock C, et al. The impact of opioid treatment on regional gastrointestinal transit. J Neurogastroenterol Motil. 2016;22:282–91.
Müller M, Canfora EE, Blaak EE. Gastrointestinal transit time, glucose homeostasis and metabolic health: modulation by dietary fibers. Nutrients. 2018;10:275.
Afshar S, Kelly SB, Seymour K, et al. The effects of bariatric procedures on bowel habit. Obes Surg. 2016;26:2348–54.
Potoczna N, Harfmann S, Steffen R, et al. Bowel habits after bariatric surgery. Obes Surg. 2008;18:1287–96.
Titus R, Kastenmeier A, Otterson MF. Consequences of gastrointestinal surgery on drug absorption. Nutr Clin Pract. 2013;28:429–36.
Seeley RJ, Chambers AP, Sandoval DA. The role of gut adaptation in the potent effects of multiple bariatric surgeries on obesity and diabetes. Cell Metab. 2015;21:369–78.
Bohlin J, Dahlin E, Dreja J, et al. Longer colonic transit time is associated with laxative and drug use, lifestyle factors, and symptoms of constipation. Acta Radiol Open. 2018;7:205846011880723.
Roager HM, Hansen LBS, Bahl MI, et al. Colonic transit time is related to bacterial metabolism and mucosal turnover in the gut. Nat Microbiol. 2016;1:16093.
Saad RJ. The wireless motility capsule: a one-stop shop for the evaluation of GI motility disorders. Curr Gastroenterol Rep. 2016;18:14.
Wright RA, Krinsky S, Fleeman C, et al. Gastric emptying and obesity. Gastroenterology. 1983;84:747–51.
Al Mushref M, Srinivasan S. Effect of high fat-diet and obesity on gastrointestinal motility. Ann Transl Med. 2013;1:14.
Vazquez Roque MI, Camilleri M, Stephens DA, et al. Gastric sensorimotor functions and hormone profile in normal weight, overweight, and obese people. Gastroenterology. 2006;131:1717–24.
Doran S, Jones KL, Andrews JM, et al. Effects of meal volume and posture on gastric emptying of solids and appetite. Am J Physiol. 1998;275:R1712–8.
Velchik MG, Reynolds JC, Alavi A. The effect of meal energy content on gastric emptying. J Nucl Med. 1989;30:1106–10.
Acknowledgements
The Talent Management Programme, Aalborg University, the Hørslev Foundation (No. 203866) and the Speciallæge Heinrich Kopps Foundation are acknowledged for supporting this study financially. Charlotte Skov at the Department of Clinical Medicine and Endocrinology, Aalborg University Hospital, is acknowledged for her contribution in regards to patient recruitment. Torben Tvedebrink at the Statistical Department at Aalborg University is acknowledged for statistical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Declaration
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ladebo, L., Pedersen, P.V., Pacyk, G.J. et al. Gastrointestinal pH, Motility Patterns, and Transit Times After Roux-en-Y Gastric Bypass. OBES SURG 31, 2632–2640 (2021). https://doi.org/10.1007/s11695-021-05308-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05308-x