Abstract
Background
Marginal ulceration (MU) and bleeding are possible complications following laparoscopic Roux-en-Y gastric bypass (RYGB). Our institution utilizes three techniques for performing the gastrojejunal anastomosis (GJA), providing a means to compare postoperative MU and bleeding as it relates to GJA technique.
Objectives
We sought to analyze the incidence of MU and bleeding between the 25-mm end-to-end anastomosis (EEA) stapler, linear stapler (LS), and robotic hand-sewn (RHS) GJA techniques.
Methods
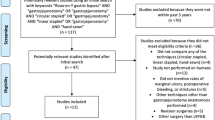
Electronic health records for all patients who had an upper endoscopy (EGD) after RYGB were queried (2010–2014). Charts were retrospectively reviewed for type of GJA, complications, endoscopic interventions, and smoking and NSAID use.
Results
Out of 1112 RYGBs, the GJA was created using an EEA, LS, or RHS approach in 58.6%, 33.6%, and 7.7% of patients, respectively. 17.4% had an EGD (19.9% EEA, 13.9% LS, and 14.0% RHS). Incidence of MU was 7.3% (9.3% EEA, 4.8% LS, and 5.8% RHS). Rates of EGD and MU were significantly higher after EEA vs. LS GJA (p<0.05). The bleeding rate was 1.5%, [1.1% EEA, 2.1% LS, and 2.3% RHS (p=NS)]. MU within 90 days of RYGB occurred in 4.1%, 0.8%, and 4.7%, respectively (p<0.05 for EEA vs LS only). NSAID and cigarette use were identified in 29.3%, 38.9%, and 60% and 17.2%, 22.2%, and 20%, respectively, for the EEA, LS, and RHS GJA (p=NS).
Conclusion
The method of GJA has an impact on rate of MU formation. A GJA fashioned with a 25-mm EEA stapler tends to have higher rates of EGD and MU.
Similar content being viewed by others
References
Cai JX, Schweitzer MA, Kumbhari V. Endoscopic management of bariatric surgery complications. Surg Laparosc Endosc Percutan Tech. 2016;26(2):93–101. https://doi.org/10.1097/SLE.0000000000000230.
Dittrich L, Schwenninger MV, Dittrich K, et al. Marginal ulcers after laparoscopic Roux-en-Y gastric bypass: analysis of the amount of daily and lifetime smoking on postoperative risk. Surg Obes Relat Dis. 2020;16(3):389–96. https://doi.org/10.1016/j.soard.2019.11.022.
Coblijn UK, Lagarde SM, de Castro SM, et al. Symptomatic marginal ulcer disease after Roux-en-Y gastric bypass: incidence, risk factors and management. Obes Surg. 2015;25(5):805–11. https://doi.org/10.1007/s11695-014-1482-9.
Major P, Janik MR, Wysocki M, et al. Comparison of circular- and linear-stapled gastrojejunostomy in laparoscopic Roux-en-Y gastric bypass: a multicenter study. Wideochir Inne Tech Maloinwazyjne. 2017;12(2):140–6. https://doi.org/10.5114/wiitm.2017.66868.
Edholm D, Sundbom M. Comparison between circular- and linear-stapled gastrojejunostomy in laparoscopic Roux-en-Y gastric bypass--a cohort from the Scandinavian Obesity Registry. Surg Obes Relat Dis. 2015;11(6):1233–6. https://doi.org/10.1016/j.soard.2015.03.010.
Edholm D, Ottosson J, Sundbom M. Importance of pouch size in laparoscopic Roux-en-Y gastric bypass: a cohort study of 14,168 patients. Surg Endosc. 2016;30(5):2011–5. https://doi.org/10.1007/s00464-015-4432-2.
Azagury DE, Abu Dayyeh BK, Greenwalt IT, et al. Marginal ulceration after Roux-en-Y gastric bypass surgery: characteristics, risk factors, treatment, and outcomes. Endoscopy. 2011;43(11):950–4. https://doi.org/10.1055/s-0030-1256951.
Siilin H, Wanders A, Gustavsson S, et al. The proximal gastric pouch invariably contains acid-producing parietal cells in Roux-en-Y gastric bypass. Obes Surg. 2005;15(6):771–7. https://doi.org/10.1381/0960892054222849.
Finks JF, Carlin A, Share D, et al. Effect of surgical techniques on clinical outcomes after laparoscopic gastric bypass--results from the Michigan Bariatric Surgery Collaborative. Surg Obes Relat Dis. 2011;7(3):284–9. https://doi.org/10.1016/j.soard.2010.10.004.
Madan AK, Harper JL, Tichansky DS. Techniques of laparoscopic gastric bypass: on-line survey of American Society for Bariatric Surgery practicing surgeons. Surg Obes Relat Dis. 2008;4(2):166–73. https://doi.org/10.1016/j.soard.2007.08.006.
Barr AC, Lak KL, Helm MC, et al. Linear vs. circular-stapled gastrojejunostomy in Roux-en-Y gastric bypass. Surg Endosc. 2019;33(12):4098–101. https://doi.org/10.1007/s00464-019-06712-2.
Ribeiro-Parenti L, Arapis K, Chosidow D, et al. Comparison of marginal ulcer rates between antecolic and retrocolic laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2015 Feb;25(2):215–21. https://doi.org/10.1007/s11695-014-1392-x.
Wennerlund J, Gunnarsson U, Strigård K, et al. Acid-related complications after laparoscopic Roux-en-Y gastric bypass: risk factors and impact of proton pump inhibitors. Surg Obes Relat Dis. 2020;16(5):620–5. https://doi.org/10.1016/j.soard.2020.01.005.
Ying VW, Kim SH, Khan KJ, et al. Prophylactic PPI help reduce marginal ulcers after gastric bypass surgery: a systematic review and meta-analysis of cohort studies. Surg Endosc. 2015;29(5):1018–23. https://doi.org/10.1007/s00464-014-3794-1.
Coblijn UK, Lagarde SM, de Castro SM, et al. The influence of prophylactic proton pump inhibitor treatment on the development of symptomatic marginal ulceration in Roux-en-Y gastric bypass patients: a historic cohort study. Surg Obes Relat Dis. 2016;12(2):246–52. https://doi.org/10.1016/j.soard.2015.04.022.
Kang X, Zurita-Macias L, Hong D, et al. A comparison of 30-day versus 90-day proton pump inhibitor therapy in prevention of marginal ulcers after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2016;12(5):1003–7. https://doi.org/10.1016/j.soard.2015.11.010.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Consent Statement
Informed consent does not apply.
Conflict of Interest
Authors 1, 2, 3, 4, 5, 6, 7, and 8 have no conflicts of interest or financial ties to disclose. Author 9 is a speaker for BD Bard and WL Gore and a consultant for Medtronic. Author 10 is a speaker for WL Gore and Medtronic, an investor in Standard Bariatrics, and a consultant for GI dynamics. Author 11 is on the speakers’ bureau of Medtronic.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sundaresan, N., Sullivan, M., Hiticas, B.A. et al. Impacts of Gastrojejunal Anastomotic Technique on Rates of Marginal Ulcer Formation and Anastomotic Bleeding Following Roux-en-Y Gastric Bypass. OBES SURG 31, 2921–2926 (2021). https://doi.org/10.1007/s11695-021-05292-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05292-2