Abstract
Introduction
Laparoscopic sleeve gastrectomy (LSG) has rapidly become popular with excellent results. However, LSG may exacerbate or increase the risk of “de novo” gastroesophageal reflux disease (GERD). Adding a fundoplication has been proposed to increase the lower esophageal sphincter competency. The aim of this study was to examine the current evidence and outcomes of sleeve-fundoplication (Sleeve-F).
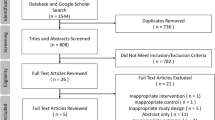
Materials and Methods
Systematic review and meta-analysis. Web of Science, PubMed, and Embase data sets were consulted.
Results
Six studies (485 patients) met the inclusion criteria. The age of the patient population ranged from 17 to 72 years old and 82% were females. All patients underwent sleeve-fundoplication. Rossetti, Collis-Nissen, and Nissen were the most commonly performed fundoplications. The estimated pooled prevalence of postoperative leak, gastric perforation, and overall complications were 1.0% (95% CI = 0.0–2.0%), 2.9% (95% CI = 0.0–8.3%), and 9.8% (95% CI = 6.7–13.4%), respectively. The pooled reoperation rate was 4.1% (95% CI = 1.3–10%). There was no mortality. At 12-month follow-up, the estimated pooled BMI and %EWL were 29.9 kg/m2 (95% CI = 28.5–31.2) and 66.2% (95% CI = 59.3–71.1), respectively, while esophagitis, PPI consumption, and GERD rates were 8.0% (95% CI 3–21%), 7.8% (95% CI 5–13%), and 11% (95% CI 4–26%).
Conclusions
This systematic review and meta-analysis shows that current evidence for Sleeve-F is limited with high postoperative gastric perforation and overall complication rates. Weight loss and GERD resolution seem promising in the short term; however, further studies are warranted to explore long-term effects with instrumental investigations. Sleeve-F should be considered cautiously while future well-structured randomized trials are warranted.




Similar content being viewed by others
Change history
16 May 2022
A Correction to this paper has been published: https://doi.org/10.1007/s11695-022-06105-w
References
Gagner M, Deitel M, Erickson AL, et al. Survey on laparoscopic sleeve gastrectomy (LSG) at the Fourth International Consensus Summit on Sleeve Gastrectomy. Obes Surg. 2013 Dec;23(12):2013–7.
Gagner M, Hutchinson C, Rosenthal R. Fifth International Consensus Conference: current status of sleeve gastrectomy. Surg Obes Relat Dis. 2016 May;12(4):750–6.
Nedelcu M, Noel P, Iannelli A, et al. Revised sleeve gastrectomy (re-sleeve). Surg Obes Relat Dis. 2015 Nov-Dec;11(6):1282–8.
Porta A, Aiolfi A, Musolino C, et al. Prospective comparison and quality of life for single-incision and conventional laparoscopic sleeve gastrectomy in a series of morbidly obese patients. Obes Surg. 2017 Mar;27(3):681–7.
Braghetto I, Korn O. Late esophagogastric anatomic and functional changes after sleeve gastrectomy and its clinical consequences with regards to gastroesophageal reflux disease. Dis Esophagus. 2019 Jun 1;32(6):doz020.
Sebastianelli L, Benois M, Vanbiervliet G, et al. Systematic endoscopy 5 years after sleeve gastrectomy results in a high rate of Barrett’s esophagus: results of a multicenter study. Obes Surg. 2019 May;29(5):1462–9.
Sharma A, Aggarwal S, Ahuja V, et al. Evaluation of gastroesophageal reflux before and after sleeve gastrectomy using symptom scoring, scintigraphy, and endoscopy. Surg Obes Relat Dis. 2014 Jul-Aug;10(4):600–5.
Snyder B, Wilson E, Wilson T, et al. A randomized trial comparing reflux symptoms in sleeve gastrectomy patients with or without hiatal hernia repair. Surg Obes Relat Dis. 2016 Nov;12(9):1681–8.
Soricelli E, Iossa A, Casella G, et al. Sleeve gastrectomy and crural repair in obese patients with gastroesophageal reflux disease and/or hiatal hernia. Surg Obes Relat Dis. 2013 May-Jun;9(3):356–61.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009 21;6(7):e1000097.
Goossen K, Tenckhoff S, Probst P, et al. Optimal literature search for systematic reviews in surgery. Langenbeck’s Arch Surg. 2018 Feb;403(1):119–29.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Vakil N, van Zanten SV, Kahrilas P, et al. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006 Aug;101(8):1900–20.
Lin L, Chu H. Meta-analysis of proportions using generalized linear mixed models. Epidemiology. 2020 Sep;31(5):713–7.
Schwarzer G, Chemaitelly H, Abu-Raddad LJ, et al. Seriously misleading results using inverse of Freeman-Tukey double arcsine transformation in meta-analysis of single proportions. Res Synth Methods. 2019 Sep;10(3):476–83.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Ferrari D, Aiolfi A, Bonitta G, Riva CG, Rausa E, Siboni S, et. al. (2018) Flexible versus rigid endoscopy in the management of esophageal foreign body impaction: systematic review and meta-analysis. World Journal of Emergency Surgery 13(1).
Clopper CJ, Pearson ES. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika. 1934;26(4):404–13.
Aiolfi A, Asti E, Rausa E, et al. Trans-gastric ERCP after Roux-en-Y gastric bypass: systematic review and meta-analysis. Obes Surg. 2018 Sep;28(9):2836–43.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Anzures-Cabrera J, Higgins JP. Graphical displays for meta-analysis: an overview with suggestions for practice. Res Synth Methods. 2010;1(1):66–80.
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 13;315(7109):629-634
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR (2009) Introduction to meta-analysis, John Wiley & Sons, Ltd, Chichester, UK
R Development Core Team (2015) A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. ISBN 3-900051-07-0.
da Silva LE, Alves MM, El-Ajouz TK, et al. Laparoscopic Sleeve-Collis-Nissen gastroplasty: a safe alternative for morbidly obese patients with gastroesophageal reflux disease. Obes Surg. 2015 Jul;25(7):1217–22.
Moon RC, Teixeira AF, Jawad MA. Safety and effectiveness of anterior fundoplication sleeve gastrectomy in patients with severe reflux. Surg Obes Relat Dis. 2017 Apr;13(4):547–52.
Nocca D, Skalli EM, Boulay E, et al. Nissen Sleeve (N-Sleeve) operation: preliminary results of a pilot study. Surg Obes Relat Dis. 2016 Dec;12(10):1832–7.
Lasnibat JP, Braghetto I, Gutierrez L, et al. Sleeve gastrectomy and fundoplication as a single procedure in patients with obesity and gastroesophageal reflux. Arq Bras Cir Dig. 2017 Jul-Sep;30(3):216–21.
Amor IB, Casanova V, Vanbiervliet G, et al. The Nissen-Sleeve (N-Sleeve): results of a cohort study. Obes Surg. 2020 Sep;30(9):3267–72.
Olmi S, Uccelli M, Cesana GC, et al. Modified laparoscopic sleeve gastrectomy with Rossetti antireflux fundoplication: results after 220 procedures with 24-month follow-up. Surg Obes Relat Dis. 2020 Sep;16(9):1202–11.
Gagner M, Ramos A, Palermo M, et al. The perfect sleeve gastrectomy. A clinical guide to evaluation, treatment, and techniques. Cham, Switzerland: Springer, 2020.
Palermo M, Edgardo S. Laparoscopic sleeve gastrectomy: how I do it J Laparoendosc Adv Surg Tech 2019, https://doi.org/10.1089/lap.2019.0452.
Patti MG, Schlottmann F. Gastroesophageal reflux after sleeve gastrectomy. JAMA Surg. 2018 Dec 1;153(12):1147–8.
Mahawar KK, Jennings N, Balupuri S, et al. Sleeve gastrectomy and gastro-oesophageal reflux disease: a complex relationship. Obes Surg. 2013 Jul;23(7):987–91.
Samakar K, McKenzie TJ, Tavakkoli A, et al. The effect of laparoscopic sleeve gastrectomy with concomitant hiatal hernia repair on gastroesophageal reflux disease in the morbidly obese. Obes Surg. 2016 Jan;26(1):61–6.
Nocca D, Nedelcu M, Loureiro M, et al. The Nissen sleeve gastrectomy: technical considerations. J Laparoendosc Adv Surg Tech A. 2020 Nov;30(11):1231–6.
Rebecchi F, Allaix ME, Patti MG, et al. Gastroesophageal reflux disease and morbid obesity: to sleeve or not to sleeve? World J Gastroenterol. 2017 Apr 7;23(13):2269–75.
Rosenthal RJ, Diaz AA, Arvidsson D, et al. International sleeve gastrectomy expert panel consensus statement: best practice guidelines based on experience of > 12,000 cases. Surg Obes Relat Dis. 2012;8:8–19.
Kichler K, Rosenthal RJ, DeMaria E, et al. Reoperative surgery for nonresponders and complicated sleeve gastrectomy operations in patients with severe obesity. An international expert panel consensus statement to define best practice guidelines. Surg Obes Relat Dis. 2019 Feb;15(2):173–86.
Angrisani L, Santonicola A, Iovino P, et al. IFSO worldwide survey 2016: primary, endoluminal, and revisional procedures. Obes Surg. 2018 Dec;28(12):3783–94.
Cottam S, Cottam D, Cottam A. Sleeve gastrectomy weight loss and the preoperative and postoperative predictors: a systematic review. Obes Surg. 2019 Apr;29(4):1388–96.
Peterli R, Wölnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA. 2018 Jan 16;319(3):255–65.
Arman GA, Himpens J, Dhaenens J, et al. Long-term (11+years) outcomes in weight, patient satisfaction, comorbidities, and gastroesophageal reflux treatment after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2016 Dec;12(10):1778–86.
Himpens J, Dobbeleir J, Peeters G. Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann Surg. 2010 Aug;252(2):319–24.
Lim CH, Lee PC, Lim E, et al. Correlation between symptomatic gastro-esophageal reflux disease (GERD) and erosive esophagitis (EE) post-vertical sleeve gastrectomy (VSG). Obes Surg. 2019 Jan;29(1):207–14.
Del Genio G, Tolone S, Gambardella C, et al. Sleeve gastrectomy and anterior fundoplication (D-SLEEVE) prevents gastroesophageal reflux in symptomatic GERD. Obes Surg. 2020 May;30(5):1642–52.
Author information
Authors and Affiliations
Contributions
AA, JM, and ER did the literature search. AA and DB formed the study design. Data collection done by AA, JM, and ER. AA and GB analyzed the data. AA, GM, and DB interpreted the data. AA wrote the manuscript. AA, GM, and DB critically reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed consent does not apply.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised to cancel Open Access
Supplementary Information
ESM 1
(DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Aiolfi, A., Micheletto, G., Marin, J. et al. Laparoscopic Sleeve-Fundoplication for Morbidly Obese Patients with Gastroesophageal Reflux: Systematic Review and Meta-analysis. OBES SURG 31, 1714–1721 (2021). https://doi.org/10.1007/s11695-020-05189-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-05189-6