Abstract
Purpose
Morbid obesity represents the most severe form of obesity and surgical intervention would be its only successful treatment. Bariatric surgery could generate modifications in carbohydrate metabolism and in lipid profile plus lipoprotein-associated proteins and enzymes, such as lipoprotein-associated phoslipase A2 (Lp-PLA2), cholesteryl ester transfer protein (CETP), and paraoxonase (PON) 1. The aim of the present study was to analyze changes in inflammation markers, carbohydrate metabolism, and lipid parameters in patients who underwent bariatric surgery.
Methods
Thirty-seven patients with morbid obesity were recruited. Evaluations were performed before (T0) and 1 (T1) and 6 (T2) months after surgery. Glucose, insulin, high-sensitivity C-reactive protein (hsCRP), triglycerides, total cholesterol, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol, apolipoproteins (apo) A-I, and B plus Interleukin 1β and 6 levels in addition to CETP, Lp-PLA2, and PON 1 activities were determined.
Results
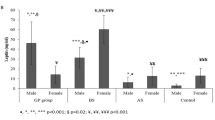
Body mass index decreased at T1 and T2 (p < 0.01). An improvement in all markers of insulin resistance (p < 0.05) was observed at T1. hsCRP levels diminished at T2 (p < 0.05). Triglyceride levels decreased at T1 and T2 (p < 0.05). HDL-C and apo A-I showed a decrease at T1 which was completely reversed at T2 (p < 0.05). Lp-PLA2 activity increased at T1, which was reversed at T2 (p < 0.05), and CETP activity was diminished at T2 (p < 0.05). PON and ARE activities decreased at T1 and partially recovered at T2 (p < 0.05).
Conclusions
These results would be indicative of a favorable effect of bariatric surgery on markers of carbohydrate metabolism and cardiovascular disease lipid risk factors.



Similar content being viewed by others
Change history
30 March 2022
This article was revised to correct the metadata tagging for author Andrea Iglesias Molli.
References
Moore D. The developing genome: an introduction to behavioral epigenetics. 1st ed: Oxford University Press; 2015.
Arteaga A. Overweight and obesity as a universal health problem. Rev Med Clin Condes. 2012;23:145–53.
Galic S, Oakhill J, Steinberg G. Adipose tissue as an endocrine organ. Mol Cell Endocrinol. 2010;316:129–39.
Michaud A, Boulet M, Veilleux A, et al. Abdominal subcutaneous and omental adipocyte morphology and its relation to gene expression, lipolysis and adipocytokine levels in women. Metabolism. 2013;63:372–81.
Wellen K, Hotamisligil G. Obesity-induced inflammatory changes in adipose tissue. J Clin Invest. 2003;112:1785–8.
Morisset A, Huot C, Légaré D, et al. Circulating IL-6 concentrations and abdominal adipocyte isoproterenol-stimulated lipolysis in women. Obesity (Silver Spring). 2008;16:1487–92.
Patel L, Buckels A, Kinghorn I, et al. Resistin is expressed in human macrophages and directly regulated by PPAR gamma activators. Biochem Biophys Res Commun. 2003;300:472–6.
Dinarello CA. Immunological and inflammatory functions of the interleukin-1 family. Annu Rev Immunol. 2009;27:519–50.
Paik J, Kim M, Kim M, et al. Circulating Lp-PLA2 activity correlates with oxidative stress and cytokines in overweight/obese postmenopausal women not using hormone replacement therapy. AGE. 2015;37:32–42.
da Silva IT, de Souza Timm A, Damasceno N. Influence of obesity and cardiometabolic makers on lipoprotein associated phospholipase A2 (Lp-PLA2) activity in adolescents: the healthy young cross-sectional study. Lipids Health Dis. 2013;12:19–27.
Onat A, Hergenç G. Low-grade inflammation, and dysfunction of high-density lipoprotein and its apolipoproteins as a major driver of cardiometabolic risk. Metab Clin Exp. 2011;60:499–512.
Onat A, Can G, Yüksel H. Dysfunction of high-density lipoprotein and its apolipoproteins: new mechanisms underlying cardiometabolic risk in the population at large. Turk Kardiyol Dern Ars. 2012;40:368–85.
Murphy A, Woollard K, Hoang A, et al. High-density lipoprotein reduces the human monocyte inflammatory response. Arterioscler Thromb Vasc Biol. 2008;28:2071–7.
Murphy A, Woollard K. High-density lipoprotein: a potent inhibitor of inflammation. Clin Exp Pharmacol Physiol. 2010;37:710–8.
Movva R, Rader D. Laboratory assessment of HDL heterogeneity and function. Clin Chem. 2008;54:788–800.
Rye K, Barter P. Formation and metabolism of pre beta-migrating, lipid-poor apolipoprotein A-I. Arterioscler Thromb Vasc Biol. 2004;24:421–8.
Davidson W, Silva R, Chantepie S, et al. Proteomic análisis of defined HDL subpopulations reveals article specific protein clusters: relevance to antioxidative function. Arterioscler Thromb Vasc Biol. 2009;29:870–6.
Kontush A, Therond P, Zerrad A, et al. Preferential sphingosine-1-phosphate enrichment and sphingomyelin depletion are key features of small dense HDL3 particles: relevance to antiapoptotic and antioxidative activities. Arterioscler Thromb Vasc Biol. 2007;27:1843–9.
Chapman M, Le Goff W, Guerin M, et al. Cholesteryl ester transfer protein: at the heart of the action of lipid modulating therapy with statins, fibrates, niacin, and cholesteryl-ester transfer protein inhibitors. Eur Heart J. 2010;31:149–64.
Arai T, Yamashita S, Hirano K, et al. Increased plasma cholesteryl-ester transfer protein in obese subjects. A possible mechanism for the reduction of serum HDL cholesterol levels in obesity. Arterioscler Thromb. 1994;14:1129–36.
Ebenbichler C, Laimer M, Kaser S, et al. Relationship between cholesterylester transfer protein and atherogenic lipoprotein profile in morbidly obese women. Arterioscler Thromb Vasc Biol. 2002;22:1465–9.
Aviram M, Rosenblat M, Bisgaier C, et al. Paraoxonase inhibits high-density lipoprotein oxidation and preserves its functions. A possible peroxidative role forparaoxonase. J Clin Invest. 1998;101:1581–90.
Bajnok L, Csongradi E, Seres I, et al. Relationship of adiponectin to serum paraoxonase 1. Atherosclerosis. 2008;197:363–7.
Abell T, Minocha A. Gastrointestinal complications of bariatric surgery: diagnosis and therapy. Am J Med Sci. 2006;331:214–8.
Arterburn D, Courcoulas A. Bariatric surgery for obesity and metabolic conditions in adults. BMJ. 2014;349:g3961.
Nguyen N, DeMaria E, Ikramuddin S, et al. The SAGES manual: a practical guide to bariatric surgery. New York: Springer; 2008.
Blank M, Hall M, Cress E, et al. Inactivation of 1-alkyl-2-acetyl-sn-glycero-3-phosphocholine by a plasma acetylhydrolase: higher activities in hypertensive rats. Biochem Biophys Res Commun. 1983;113:666–71.
Lowry O, Rosebrough N, Farr A, et al. Protein measurement with the folinphenol reagent. J Biol Chem. 1951;193:265–75.
Furlong C, Richter R, Seidel S, et al. Spectrophotometric assays for the enzymatic hydrolysis of the active metabolites of chlorpyrifos and parathion by plasma paraoxonase/arylesterase. Anal Biochem. 1989;80:242–7.
Han TS, Lean ME. A clinical perspective of obesity, metabolic syndrome and cardiovascular disease. JRSM Cardiovasc Dis. 2016;5:2048004016633371.
Yan Y, Sha Y, Yao G, et al. Roux-en-Y gastric bypass versus medical treatment for type 2 diabetes mellitus in obese patients: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2016;95:e3462.
Vest AR, Heneghan HM, Agarwal S, et al. Bariatric surgery and cardiovascular outcomes: a systematic review. Heart. 2012;98:1763–77.
Poirier P, Cornier MA, Mazzone T, et al. Bariatric surgery and cardiovascular risk factors: a scientific statement from the American Heart Association. Circulation. 2011;123:1683–701.
Courcoulas AP, Christian NJ, Belle SH, et al. Longitudinal Assessment of Bariatric Surgery (LABS) Consortium. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA. 2013;310:2416–25.
Adams TD, Davidson LE, Litwin SE, et al. Health benefits of gastric bypass surgery after 6 years. JAMA. 2012;308:1122–31.
Asztalos BF, Swarbrick MM, Schaefer EJ, et al. Effects of weight loss, induced by gastric bypass surgery, on HDL remodeling in obese women. J Lipid Res. 2010;51:2405–12.
Carlsson E, Allin K, Madsbad S, et al. Phosphatidylcholine and its relation to apolipoproteins A-1 and B changes after roux-en-Y gastric bypass: a cohort study. Lipids Health Dis. 2019;18:169.
Shih KC, Janckila AJ, Lee WJ, et al. Effects of bariatric weight loss surgery on glucose metabolism, inflammatory cytokines, and serum tartrate-resistant acid phosphatase 5a in obese Chinese adults. Clin Chim Acta. 2016;453:197–202.
Bray GA, Siri-Tarino PW. The role of macronutrient content in the diet for weight management. Endocrinol Metab Clin N Am. 2016;45:581–604.
Rolland C. Broom I the effects of very-low-calorie diets on HDL: a review. Cholesterol. 2011;306278:2011.
Shoji T, Nishizawa Y, Koyama H, et al. High-density-lipoprotein metabolism during a very-low-calorie diet. Am J Clin Nutr. 1992;56:297S–8S.
Desroches S, Paradis ME, Pérusse M, et al. A-II, and VLDL-B-100 metabolism in men: comparison of a low-fat diet and a high-monounsaturated fatty acid diet. J Lipid Res. 2004;45:2331–8.
Vélez-Carrasco W, Lichtenstein AH, Welty FK, et al. Dietary restriction of saturated fat and cholesterol decreases HDL ApoA-I secretion. Arterioscler Thromb Vasc Biol. 1999;19:918–24.
Gero D, Favre L, Allemann P, et al. Laparoscopic roux-en-Y gastric bypass improves lipid profile and decreases cardiovascular risk: a 5-year longitudinal cohort study of 1048 patients. Obes Surg. 2018;28:805–11.
De Stefano A, Mannucci L, Tamburi F, et al. Lp-PLA2, a new biomarkerof vascular disorders in metabolicdiseases. Int J Immunopathol Pharmacol. 2019;33:2058738419827154.
Julve J, Pardina E, Pérez-Cuéllar M, et al. Bariatric surgery in morbidly obese patients improves the atherogenic qualitative properties of the plasma lipoproteins. Atherosclerosis. 2014;234:200–5.
Oberbach A, von Bergen M, Blüher S, et al. Combined serum proteomic and metabolomics profiling after laparoscopic sleeve gastrectomy in children and adolescents. J Laparoendosc Adv Surg Tech A. 2012;22:184–8.
Ferretti G, Bacchetti T, Masciangelo S, et al. Altered inflammation, paraoxonase-1 activity and HDL physicochemical properties in obese humans with and without Prader-Willi syndrome. Dis Model Mech. 2012;5:698–705.
Van Gaal L, Zhang A, Steijaert M, et al. Human obesity: from lipid abnormalities to lipidoxidation. Int J Obes Relat Metab Disord. 1995;3:21–6.
Funding
The present work was supported by grants from Agencia Nacional de Promoción Científica y Tecnológica (PICT 2016–2018), Universidad de Buenos Aires (UBACyT 20020150100054BA), and CONICET (PIP 112201 501003 00CO).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article was revised to correct the metadata tagging for author Andrea Iglesias Molli.
Rights and permissions
About this article
Cite this article
Chiappe, E.L., Martin, M., Iglesias Molli, A. et al. Effect of Roux-en-Y Gastric Bypass on Lipoprotein Metabolism and Markers of HDL Functionality in Morbid Obese Patients. OBES SURG 31, 1092–1098 (2021). https://doi.org/10.1007/s11695-020-05076-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-05076-0