Abstract
Objective
To validate the GOAL questionnaire as obstructive sleep apnea (OSA) screening tool in bariatric surgery (BS) patients and compare it with other existing instruments.
Methods
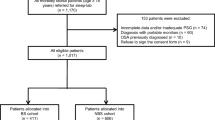
Before performing full polysomnography (PSG), all participants were screened for OSA with the following instruments: GOAL, STOP, STOP-Bang, No-Apnea, NoSAS, and Epworth Sleepiness Scale (ESS). Discrimination was assessed by area under the curve (AUC), while predictive parameters were calculated by contingency tables. Correlation was evaluated by the Spearman correlation coefficient (r). OSA severity was classified based on the apnea/hypopnea index (AHI): ≥ 5.0/h (OSA≥ 5), ≥ 15.0/h (OSA≥ 15), and ≥ 30.0/h (OSA≥ 30).
Results
Overall, 814 BS individuals (70.8% of females) were enrolled. We found a high prevalence of OSA≥ 5 (82.6%), OSA≥ 15 (60.0%), and OSA≥ 30 (38.8%). GOAL questionnaire was positively correlated with the AHI (r = 0.570, p < 0.001). Using a score ≥ 2 to classify patients at high risk of OSA, GOAL questionnaire had sensitivities ranging from 73.7 to 89.2% and specificities ranging from 78.2 to 51.0% for predicting OSA≥ 5, OSA≥ 15, and OSA≥ 30. At all OSA severity levels, GOAL exhibited similar and non-inferior discrimination when compared with STOP-Bang, No-Apnea, and NoSAS (all p values > 0.05), and performed significantly better than STOP and ESS (all p values < 0.001).
Conclusions
In a cohort of BS patients, GOAL, No-Apnea, STOP-Bang, and NoSAS, but not ESS and STOP, enable satisfactory discrimination as OSA screening instruments at all disease severity levels.



Similar content being viewed by others
References
Benjafield AV, Ayas NT, Eastwood PR, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019;7(8):687–98.
Heinzer R, Vat S, Marques-Vidal P, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015;3(4):310–8.
Peppard PE, Young T, Barnet JH, et al. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–14.
Tufik S, Santos-Silva R, Taddei JA, et al. Obstructive sleep apnea syndrome in the Sao Paulo Epidemiologic Sleep Study. Sleep Med. 2010;11(5):441–6.
Kapur VK, Auckley DH, Chowdhuri S, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13(3):479–504.
Wickwire EM, Tom SE, Vadlamani A, et al. Older adult US Medicare beneficiaries with untreated obstructive sleep apnea are heavier users of health care than matched control patients. J Clin Sleep Med. 2020;16(1):81–9.
Burks SV, Anderson JE, Panda B, et al. Employer-mandated obstructive sleep apnea treatment and healthcare cost savings among truckers. Sleep. 2020;43(4):zsz262.
Vo TN, Kats AM, Langsetmo L, et al. Association of sleep-disordered breathing with total healthcare costs and utilization in older men: the Outcomes of Sleep Disorders in Older Men (MrOS Sleep) study. Sleep. 2020;43(1):zsz209.
Newman AB, Foster G, Givelber R, et al. Progression and regression of sleep-disordered breathing with changes in weight: the Sleep Heart Health Study. Arch Intern Med. 2005;165(20):2408–13.
Mortimore I, Marshall I, Wraith PK, et al. Neck and total body fat deposition in nonobese and obese patients with sleep apnea compared with that in control subjects. Am J Respir Crit Care Med. 1998;157(1):280–3.
Young T, Peppard PE, Taheri S. Excess weight and sleep-disordered breathing. J Appl Physiol (1985). 2005;99(4):1592–9.
Kositanurit W, Muntham D, Udomsawaengsup S, et al. Prevalence and associated factors of obstructive sleep apnea in morbidly obese patients undergoing bariatric surgery. Sleep Breath. 2018;22(1):251–6.
Duarte RL, Magalhães-da-Silveira FJ. Factors predictive of obstructive sleep apnea in patients undergoing pre-operative evaluation for bariatric surgery and referred to a sleep laboratory for polysomnography. J Bras Pneumol. 2015;41(5):440–8.
Gasa M, Salord N, Fortuna AM, et al. Optimizing screening of severe obstructive sleep apnea in patients undergoing bariatric surgery. Surg Obes Relat Dis. 2013;9(4):539–46.
Loo GH, Rajan R, Mohd Tamil A, et al. Prevalence of obstructive sleep apnea in an Asian bariatric population: an underdiagnosed dilemma. Surg Obes Relat Dis. 2020:S1550-7289(20)30083-6.
Yeh PS, Lee YC, Lee WJ, et al. Clinical predictors of obstructive sleep apnea in Asian bariatric patients. Obes Surg. 2010;20(1):30–5.
Sareli AE, Cantor CR, Williams NN, et al. Obstructive sleep apnea in patients undergoing bariatric surgery-a tertiary center experience. Obes Surg. 2011;21(3):316–27.
Peromaa-Haavisto P, Tuomilehto H, Kössi J, et al. Prevalence of obstructive sleep apnoea among patients admitted for bariatric surgery. A prospective multicentre trial. Obes Surg. 2016;26(7):1384–90.
Fritscher LG, Canani S, Mottin CC, et al. Bariatric surgery in the treatment of obstructive sleep apnea in morbidly obese patients. Respiration. 2007;74(6):647–52.
Zhang Y, Wang W, Yang C, et al. Improvement in nocturnal hypoxemia in obese patients with obstructive sleep apnea after bariatric surgery: a meta-analysis. Obes Surg. 2019;29(2):601–8.
Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–52.
Rasmussen JJ, Fuller WD, Ali MR. Sleep apnea syndrome is significantly underdiagnosed in bariatric surgical patients. Surg Obes Relat Dis. 2012;8(5):569–73.
Ravesloot MJ, van Maanen JP, Hilgevoord AA, et al. Obstructive sleep apnea is underrecognized and underdiagnosed in patients undergoing bariatric surgery. Eur Arch Otorhinolaryngol. 2012;269(7):1865–71.
Carneiro G, Flório RT, Zanella MT, et al. Is mandatory screening for obstructive sleep apnea with polysomnography in all severely obese patients indicated? Sleep Breath. 2012;16(1):163–8.
Farinholt GN, Carr AD, Chang EJ, et al. A call to arms: obese men with more severe comorbid disease and underutilization of bariatric operations. Surg Endosc. 2013;27(12):4556–63.
O’Keeffe T, Patterson EJ. Evidence supporting routine polysonography before bariatric surgery. Obes Surg. 2004;14(1):23–6.
Lopez PP, Stefan B, Schulman CI, et al. Prevalence of sleep apnea in morbidly obese patients who presented for weight loss surgery evaluation: more evidence for routine screening for obstructive sleep apnea before weight loss surgery. Am Surg. 2008;74(9):834–8.
de Raaff CA, Pierik AS, Coblijn UK, et al. Value of routine polysomnography in bariatric surgery. Surg Endosc. 2017;31(1):245–8.
Nepomnayshy D, Hesham W, Erikson B, et al. Sleep apnea: is routine preoperative screening necessary? Obes Surg. 2013;23(3):287–91.
O’Reilly E, Doherty L, O’Boyle C. How relevant is pre-operative obstructive sleep apnoea in the asymptomatic bariatric surgery patient? Obes Surg. 2020;30(3):969–74.
Kong WT, Chopra S, Kopf M, et al. Perioperative risks of untreated obstructive sleep apnea in the bariatric surgery patient: a retrospective study. Obes Surg. 2016;26(12):2886–90.
Carron M, Zarantonello F, Tellaroli P, et al. Perioperative noninvasive ventilation in obese patients: a qualitative review and meta-analysis. Surg Obes Relat Dis. 2016;12(3):681–92.
Nagappa M, Patra J, Wong J, et al. Association of STOP-Bang questionnaire as a screening tool for sleep apnea and postoperative complications: a systematic review and bayesian meta-analysis of prospective and retrospective cohort studies. Anesth Analg. 2017;125(4):1301–8.
Chang KW, Steward DL, Tabangin ME, et al. Clinical use of the STOP-BANG questionnaire to determine postoperative risk in veterans. Laryngoscope. 2019;129(1):259–64.
de Raaff CA, Coblijn UK, de Vries N, et al. Is fear for postoperative cardiopulmonary complications after bariatric surgery in patients with obstructive sleep apnea justified? A systematic review. Am J Surg. 2016;211(4):793–801.
van Veldhuisen SL, Arslan I, Deden LN, et al. Safety of continuous postoperative pulse oximetry monitoring without obstructive sleep apnea screening in > 5000 patients undergoing bariatric surgery. Obes Surg. 2020;30(3):1079–85.
Abrishami A, Khajehdehi A, Chung F. A systematic review of screening questionnaires for obstructive sleep apnea. Can J Anesth. 2010;57:423–38.
Ramachandran SK, Josephs LA. A meta-analysis of clinical screening tests for obstructive sleep apnea. Anesthesiology. 2009;110:928–39.
Senaratna CV, Perret JL, Matheson MC, et al. Validity of the Berlin questionnaire in detecting obstructive sleep apnea: systematic review and meta-analysis. Sleep Med Rev. 2017;36:116–24.
Duarte RL, Magalhães-da-Silveira FJ, Oliveira-e-Sá TS, et al. Obstructive sleep apnea screening with a 4-item instrument, named GOAL questionnaire: development, validation and comparative study with No-Apnea, STOP-Bang, and NoSAS. Nat Sci Sleep. 2020;12:57–67.
Horvath CM, Jossen J, Kröll D, et al. Prevalence and prediction of obstructive sleep apnea prior to bariatric surgery-gender-specific performance of four sleep questionnaires. Obes Surg. 2018;28(9):2720–6.
Modena DAO, Cazzo E, Cândido EC, et al. Obstructive sleep apnea syndrome among obese individuals: a cross-sectional study. Rev Assoc Med Bras. 2017;63(10):862–8.
Duarte RLM, Mello FCQ, Magalhães-da-Silveira FJ, et al. Comparative performance of screening instruments for obstructive sleep apnea in morbidly obese patients referred to a sleep laboratory: a prospective cross-sectional study. Sleep Breath. 2019;23(4):1123–32.
Vasas P, Gupta A, Owers C, et al. Obstructive sleep apnoea screening preoperatively with the Epworth questionnaire: is it worth it…? Obes Surg. 2019;29(3):851–7.
Dixon JB, Schachter LM, O’Brien PE. Predicting sleep apnea and excessive day sleepiness in the severely obese: indicators for polysomnography. Chest. 2003;123(4):1134–41.
Glazer SA, Erickson AL, Crosby RD, et al. The evaluation of screening questionnaires for obstructive sleep apnea to identify high-risk obese patients undergoing bariatric surgery. Obes Surg. 2018;28(11):3544–52.
Duarte RLM, Rabahi MF, Magalhães-da-Silveira FJ, et al. Simplifying the screening of obstructive sleep apnea with a 2-item model, No-Apnea: a cross-sectional study. J Clin Sleep Med. 2018;14(7):1097–107.
Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108(5):812–21.
Marti-Soler H, Hirotsu C, Marques-Vidal P, et al. The NoSAS score for screening of sleep-disordered breathing: a derivation and validation study. Lancet Respir Med. 2016;4(9):742–8.
Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–5.
Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597–619.
Cowan DC, Allardice G, MacFarlane D, et al. Predicting sleep disordered breathing in outpatients with suspected OSA. BMJ Open. 2014;4(4):e004519.
Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983;148(3):839–43.
Fredheim JM, Røislien J, Hjelmesæth J. Validation of a portable monitor for the diagnosis of obstructive sleep apnea in morbidly obese patients. J Clin Sleep Med. 2014;10(7):751–7A.
Oliveira MG, Treptow EC, Fukuda C, et al. Diagnostic accuracy of home-based monitoring system in morbidly obese patients with high risk for sleep apnea. Obes Surg. 2015;25(5):845–51.
Chung F, Subramanyam R, Liao P, et al. High STOP-Bang score indicates a high probability of obstructive sleep apnoea. Br J Anaesth. 2012;108(5):768–75.
Farney RJ, Walker BS, Farney RM, et al. The STOP-Bang equivalent model and prediction of severity of obstructive sleep apnea: relation to polysomnographic measurements of the apnea/hypopnea index. J Clin Sleep Med. 2011;7(5):459–65.
Chung F, Yang Y, Liao P. Predictive performance of the STOP-Bang score for identifying obstructive sleep apnea in obese patients. Obes Surg. 2013;23(12):2050–7.
Ioachimescu OC, Allam JS, Samarghandi A, et al. Performance of peripheral arterial tonometry based testing for the diagnosis of obstructive sleep apnea in a large sleep clinic cohort. J Clin Sleep Med. 2020; https://doi.org/10.5664/jcsm.8620.
Yalamanchali S, Farajian V, Hamilton C, et al. Diagnosis of obstructive sleep apnea by peripheral arterial tonometry: meta-analysis. JAMA Otolaryngol Head Neck Surg. 2013;139(12):1343–50.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Duarte, R.L.M., Magalhães-da-Silveira, F.J. & Gozal, D. Validation of the GOAL Questionnaire as an Obstructive Sleep Apnea Screening Instrument in Bariatric Surgery Candidates: a Brazilian Single-Center Study. OBES SURG 30, 4802–4809 (2020). https://doi.org/10.1007/s11695-020-04888-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04888-4