Abstract
Purpose
Morbid obesity is associated with reduced patients’ perception quality of life (QoL). The health benefit of Laparoscopic Roux-en-Y gastric bypass (LRYGB) is well established with long-term weight control and QoL improvement. The laparoscopic functional gastric bypass with fundectomy and gastric remnant exploration (LRYGBfse) has been described with promising results in terms of weight loss and comorbid resolution. The purpose of this study was to investigate its contribution on patients’ QoL at 5-year follow-up.
Material and Methods
Multicenter prospective study (2009–2018). QoL was assessed at baseline and annually with the Gastrointestinal Quality of Life Index (GIQLI), Moorehead-Ardelt Quality of Life Questionnaire II (M-A-QoLQII), and Short-Form 36 (SF-36).
Results
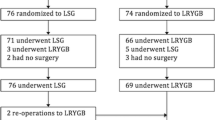
Overall, 752 patients underwent the LRYGBfse. Three-hundred forty-four patients completed the 5-year follow-up. Median postoperative %TBWL at 1, 2, 3, and 5 years were 33.6, 33.9, 33.7, and 31.4%, respectively. Median GIQLI total score before and at 1, 2, 3, and 5 years after LRYGBfse was 82.6, 96.1, 113.1, 112.5, and 108.4. Median M-A-QoLQII total score before and at 1, 2, 3, and 5 years after surgery was 0.6, 1.6, 2.1, 2.0, and 1.6. Compared with baseline, the 5-year follow-up improvement was statistically significant for the GIQLI and M-A-QoLQII (p < 0.001). Similarly, all eight SF-36 items and both the Physical and Mental component scores were significantly improved (p < 0.001).
Conclusions
The functional LRYGBfse seems associated with a long-standing weight loss and QoL improvement. This seems driven by better gastrointestinal symptoms and physical and social functions combined with improved emotional aspects.



Similar content being viewed by others
References
van Nunen AM, Wouters EJ, Vingerhoets AJ, et al. The healthrelated quality of life of obese persons seeking or not seeking surgical or non-surgical treatment: a meta-analysis. Obes Surg. 2007;17(10):1357–66.
Sarwer DB, Lavery M, Spitzer JC. A review of the relationships between extreme obesity, quality of life, and sexual function. Obes Surg. 2012;22(4):668–76.
Andersen JR, Aasprang A, Karlsen TI, et al. Health-related quality of life after bariatric surgery: a systematic review of prospective long-term studies. Surg Obes Relat Dis. 2015;11(2):466–73.
Rausa E, Kelly ME, Galfrascoli E, et al. Quality of life and gastrointestinal symptoms following laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy: a systematic review. Obes Surg. 2019;29(4):1397–402.
Cherick F, Te V, Anty R, et al. Bariatric surgery significantly improves the quality of sexual life and self-esteem in morbidly obese women. Obes Surg. 2019;29(5):1576–82.
Hu Z, Sun J, Li R, et al. A comprehensive comparison of LRYGB and LSG in obese patients including the effects on QoL, comorbidities, weight loss, and complications: a systematic review and meta-analysis. Obes Surg. 2019;30:819–27. https://doi.org/10.1007/s11695-019-04306-4. [Epub ahead of print].
Porta A, Aiolfi A, Musolino C, et al. Prospective comparison and quality of life for single-incision and conventional laparoscopic sleeve gastrectomy in a series of morbidly obese patients. Obes Surg. 2017;27(3):681–7.
Lindekilde N, Gladstone BP, Lübeck M, et al. The impact of bariatric surgery on quality of life: a systematic review and meta-analysis. Obes Rev. 2015;16(8):639–51.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23:427–36.
Kolotkin RL, Davidson LE, Crosby RD, et al. Six-year changes in health-related quality of life in gastric bypass patients versus obese comparison groups. Surg Obes Relat Dis. 2012;8(5):625–33.
Aiolfi A, Asti E, Rausa E, Bernardi D, Bonitta G, Bonavina L. Trans-gastric ERCP after Roux-en-Y gastric bypass: systematic review and meta-analysis. Obes Rev 2018;28(9):2836-2843.
Zappa MA, Aiolfi A, Musolino C, et al. Vertical gastric bypass with fundectomy: feasibility and 2-year follow-up in a series of morbidly obese patients. Obes Surg. 2017;27(8):2145–50.
Lesti G, Aiolfi A, Mozzi E, et al. Laparoscopic gastric bypass with fundectomy and gastric remnant exploration (LRYGBfse): results at 5-year follow-up. Obes Surg. 2018;28(9):2626–33.
Eypasch E, Williams JI, Wood-Dauphinee S, et al. Gastrointestinal quality of life index: development, validation and application of a new instrument. Br J Surg. 1995;82(2):216–22.
Moorehead MK, Ardelt-Gattinger E, Lechner H, et al. The validation of the Moorehead–Ardelt quality of life questionnaire II. Obes Surg. 2003;13:684–92.
Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
R Core Team R: a language and environment for statistical computing. R Foundation for Statistical Computing [cited 2018 Mar 30]. Available from: www.r-project.org.
Abilés V, Rodríguez-Ruiz S, Abilés J, et al. Psychological characteristics of morbidly obese candidates for bariatric surgery. Obes Surg. 2010;20(2):161–7.
Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring). 2009;17(5):941–64.
Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220–9.
Pimenta FB, Bertrand E, Mograbi DC, et al. The relationship between obesity and quality of life in Brazilian adults. Front Psychol. 2015;6:966.
Silva JN. Vasconcelos H1, Figueiredo-Braga M, et al. How is bariatric surgery improving the quality of life of obese patients: a Portuguese cross-sectional study. Acta Medica Port. 2018;31(7–8):391–8.
Nickel F, Schmidt L, Bruckner T, et al. Gastrointestinal quality of life improves significantly after sleeve gastrectomy and Roux-en-Y gastric bypass-a prospective cross-sectional study within a 2-year follow-up. Obes Surg. 2017;27(5):1292–7.
Dreber H, Thorell A, Reynisdottir S, et al. Health-related quality of life 5 years after Roux-en-Y gastric bypass in young (18-25 years) versus older (≥ 26 years) adults: a Scandinavian Obesity Surgery Registry study. Obes Surg. 2019;29(2):434–43.
Macano CAW, Nyasavajjala SM, Brookes A, et al. Comparing quality of life outcomes between laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass using the RAND36 questionnaire. Int J Surg. 2017;42:138–42.
Reynolds CL, Byrne SM, Hamdorf JM, et al. Treatment success: investigating clinically significant change in quality of life following bariatric surgery. Obes Surg. 2017;27(7):1842–8.
Warkentin LM, Majumdar SR, Johnson JA, et al. Weight loss required by the severely obese to achieve clinically important differences in health-related quality of life: two-year prospective cohort study. BMC Med. 2014;12:175–84.
Kolotkin RL, Kim J, Davidson LE, et al. 12-year trajectory of health-related quality of life in gastric bypass patients versus comparison groups. Surg Obes Relat Dis. 2018;14(9):1359–65.
Salminen P, Helmiö M, Ovaska J, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity the SLEEVEPASS randomized clinical trial. JAMA J Am Med Assoc. 2018;319(3):241–54.
Lee WJ, Pok EH, Almulaifi A, et al. Medium-term results of laparoscopic sleeve gastrectomy: a matched comparison with gastric bypass. Obes Surg. 2015;25(8):1431–8.
Slim K, Bousquet J, Kwiatkowski F, et al. First validation of the French version of the Gastrointestinal Quality of Life Index (GIQLI). Gastroenterol Clin Biol. 1999;23(1):25–31.
Peterli R, Wölnerhanssen BK, Vetter D, et al. Laparoscopic sleeve gastrectomy versus Roux-Y-gastric bypass for morbid obesity-3-year outcomes of the prospective randomized Swiss Multicenter Bypass Or Sleeve Study (SM-BOSS). Ann Surg. 2017;265(3):466–73.
Ignat M, Vix M, Imad I, et al. Randomized trial of Roux-en-Y gastric bypass versus sleeve gastrectomy in achieving excess weight loss. Br J Surg. 2017;104(3):248–56.
Boan J, Kolotkin RL, Westman EC, et al. Binge eating, quality of life and physical activity improve after Roux-en-Y gastric bypass for morbid obesity. Obes Surg. 2004;14(3):341–8.
Maniscalco M, Zedda A, Giardiello C, et al. Effect of bariatric surgery on the six-minute walk test in severe uncomplicated obesity. Obes Surg. 2006;16(7):836–41.
Szmulewicz A, Wanis KN, Gripper A, et al. Mental health quality of life after bariatric surgery: a systematic review and meta-analysis of randomized clinical trials. Clin Obes. 2019;9(1):e12290.
Zhang Y, Zhao H, Cao Z, et al. A randomized clinical trial of laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy for the treatment of morbid obesity in China: a 5-year outcome. Obes Surg. 2014;24(10):1617–24.
Arolfo S, Scozzari G, Di Benedetto G, et al. Surgically induced weight loss effects on sexual quality of life of obese men: a prospective evaluation. Surg Endosc. 2020; https://doi.org/10.1007/s00464-019-07356-y. [Epub ahead of print]
Arcila D, Velázquez D, Gamino R, et al. Quality of life in bariatric surgery. Obes Surg. 2002;12(5):661–5.
Gils Contreras A, Bonada Sanjaume A, Becerra-Tomás N, et al. Adherence to Mediterranean diet or physical activity after bariatric surgery and its effects on weight loss, quality of life, and food tolerance. Obes Surg. 2020;30(2):687–96.
Dagsland V, Andenæs R, Karlsen TI. Generic health-related quality of life may not be associated with weight loss 4 years after bariatric surgery: a cross-sectional study. Obes Surg. 2018;28(10):3142–50.
Yu P-J, Tsou J-J, Lee W-J, et al. Impairment of gastrointestinal quality of life in severely obese patients. World J Gastroenterol. 2014;20(22):7027–33.
Author information
Authors and Affiliations
Contributions
AA, FL, and MAZ did the literature search. AA, DB, and GL formed the study design. Data collection done by AA, FL, AS, GB, GL, and MAZ. AA, GB, GL, and DB analysed the data. AA, GL, DB, and MAZ interpreted the data. AA wrote the manuscript. AA, GL, DB, and MAZ critically reviewed the manuscript
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Statement
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lesti, G., Bona, D., Sozzi, A. et al. Impact of Functional Laparoscopic Gastric Bypass with Fundectomy and Gastric Remnant Exploration (LRYGBfse) on Patients’ Quality of Life: Trajectory and 5-Year Follow-up Result. OBES SURG 30, 3046–3053 (2020). https://doi.org/10.1007/s11695-020-04650-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04650-w