Abstract
Purpose
Bariatric surgery is the method of choice for the management or treatment of obesity. Bariatric surgery brings about several physiological changes in the body and is associated with set of complications. The aim of this study is to provide guidelines on post bariatric surgery management based on consensus by the Spanish society for Obesity Surgery (Sociedad Española de Cirugía de la Obesidad) (SECO) and the Spanish Society for the Study of Obesity (Sociedad Española para el Estudio de la Obesidad) (SEEDO).
Method
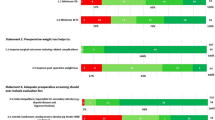
The boards proposed seven experts from each society. The experts provided the evidence and a grade of recommendation on the selected topics based on systematic reviews/meta-analysis. A list of clinical practical recommendations levels of evidence and grades of these recommendations was derived from the consensus statements from the members of these societies.
Results
Seventeen topics related to post-operative management were reviewed after bariatric surgery. The experts came with 47 recommendations and statements. The mean number of persons voting at each statement was 54 (range 36-76).
Conclusion
In this consensus, we have designed a set of guidelines to be followed while managing patients after bariatric surgery. Expertise and knowledge of the clinicians are required to convey suitable considerations to the post-bariatric patients. There should also be extensive follow-up plans for the bariatric surgery patients.
Similar content being viewed by others
References
WHO Global Health Observatory Data Repository [online database]. Geneva, World Health Organization. 2016. http://apps.who.int/gho/data/view.main
Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273:219–34.
Lopez-de-Andres A, Jiménez-García R, Hernández-Barrera V, et al. Trends in utilization and outcomes of bariatric surgery in obese people with and without type 2 diabetes in Spain (2001–2010). Diabetes Res Clin Pract. 2013;99:300–6.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric Surgery Worldwide 2013. Obes Surg. 2015;25:1822–32.
Isom KA, Andromalos L, Ariagno M, et al. Nutrition and metabolic support recommendations for the bariatric patient. Nutr Clin Pract. 2014;29:718–39.
Rubio MA, Martínez C, Vidal O, et al. Documento de consenso sobre cirugía bariátrica. Rev Esp Obes. 2004;4:223–49.
Heber D, Greenway FL, Kaplan LM, et al. Still C; Endocrine Society.Endocrine and nutritional management of the post-bariatric surgery patient: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2010;95:4823–43.
Fried M, Yumuk V, Oppert JM, et al. Frühbeck G; International Federation for Surgery of Obesity and Metabolic Disorders-European Chapter (IFSO-EC); European Association for the Study of Obesity (EASO); European Association for the Study of Obesity Obesity Management Task Force (EASO OMTF). Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg. 2014;24:42–55.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient--2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity (Silver Spring). 2013;21(Suppl 1):S1–27.
Jericó C, Bretón I. García Ruiz de Gordejuela A, de Oliveira AC, Rubio MÁ, Tinahones FJ, Vidal J, Vilarrasa N. Diagnóstico y tratamiento del déficit de hierro, con o sin anemia, pre y poscirugía bariátrica. Endocrinol Nutr. 2016;63:32–42.
Alexandrou A, Armeni E, Kouskouni E, et al. Lambrinoudaki I Cross-sectional long-term micronutrient deficiencies after sleeve gastrectomy versus Roux-en-Y gastric bypass: a pilot study. Surg Obes Relat Dis. 2014;10:262–8.
Weng TC, Chang CH, Dong YH, et al. Anaemia and related nutrient deficiencies after Roux-en-Y gastric bypass surgery: a systematic review and meta-analysis. BMJ Open. 2015;5:e006964.
Majumder S, Soriano J, Louie Cruz A, et al. Vitamin B12 deficiency in patients undergoing bariatric surgery: preventive strategies and key recommendations. Surg Obes Relat Dis. 2013;9:1013–9.
Kwon Y, Kim HJ, Lo Menzo E, et al. Anemia, iron and vitamin B12 deficiencies after sleeve gastrectomy compared to Roux-en-Y gastric bypass: a meta-analysis. Surg Obes Relat Dis. 2014;10:589–97.
Smelt HJ, Pouwels S, Smulders JF. Different Supplementation Regimes to Treat Perioperative Vitamin B12 Deficiencies in Bariatric Surgery: a Systematic Review. Obes Surg. 2017;27:254–62.
Schafer AL, Weaver CM, Black DM, et al. Intestinal Calcium Absorption Decreases Dramatically After Gastric Bypass Surgery Despite Optimization of Vitamin D Status. J Bone Miner Res. 2015;30:1377–85.
Chakhtoura MT, Nakhoul NN, Shawwa K, et al. Hypovitaminosis D in bariatric surgery: A systematic review of observational studies. Metabolism. 2016;65:574–85.
Homan J, Ruinemans-Koerts J, Aarts EO, et al. Management of vitamin K deficiency after biliopancreatic diversion with or without duodenal switch. Surg Obes Relat Dis. 2016;12:338–44.
Nett P, Borbély Y, Kröll D. Micronutrient Supplementation after Biliopancreatic Diversion with Duodenal Switch in the Long Term. Obes Surg. 2016;26:2469–74.
Moore CE, Sherman V. Vitamin D supplementation efficacy: sleeve gastrectomy versus gastric bypass surgery. Obes Surg. 2014;24:2055–60.
Chakhtoura MT, Nakhoul N, Akl EA, et al. Guidelines on vitamin D replacement in bariatric surgery: Identification and systematic appraisal. Metabolism. 2016;65:586–97.
de Luis DA, Pacheco D, Izaola O, et al. Zinc and copper serum levels of morbidly obese patients before and after biliopancreatic diversion: 4 years of follow-up. J Gastrointest Surg. 2011;15:2178–81.
Boldery R, Fielding G, Rafter T, et al. Nutritional deficiency of selenium secondary to weight loss (bariatric) surgery associated with life-threatening cardiomyopathy. Heart Lung Circ. 2007;16:123–6.
Moizé V, Andreu A, Flores L, et al. Long-term dietary intake and nutritional deficiencies following sleeve gastrectomy or Roux-En-Y gastric bypass in a mediterranean population. J Acad Nutr Diet. 2013;113:400–10.
Balsa JA, Botella-Carretero JI, Gómez-Martín JM, et al. Copper and zinc serum levels after derivative bariatric surgery: differences between Roux-en-Y gastric bypass and biliopancreatic diversion. Obes Surg. 2011;21:744–50.
Kumar P, Hamza N, Madhok B, et al. Copper Deficiency after Gastric Bypass for Morbid Obesity: a Systematic Review. Obes Surg. 2016;26:1335–42.
Mahawar KK, Bhasker AG, Bindal V, et al. Zinc Deficiency after Gastric Bypass for Morbid Obesity: a Systematic Review. Obes Surg. 2017;27:522–9.
Allied Health Sciences Section Ad Hoc Nutrition Committee, Aills L, Blankenship J, et al. ASMBS Allied Health Nutritional Guidelines for the Surgical Weight Loss Patient. Surg Obes Relat Dis. 2008;4(5 Suppl):S73–108.
Gillon S, Jeanes YM, Andersen JR, et al. Micronutrient Status in Morbidly Obese Patients Prior to Laparoscopic Sleeve Gastrectomy and Micronutrient Changes 5 years Post-surgery. Obes Surg. 2017;27:606–12.
Scopinaro N, Marinari GM, Pretolesi F, et al. Energy and nitrogen absorption after biliopancreatic diversion. Obes Surg. 2000;10:436–41.
Handzlik-Orlik G, Holecki M, Orlik B, et al. Nutrition management of the post-bariatric surgery patient. Nutr Clin Pract. 2015;30:383–92.
Moizé V, Andreu A, Rodríguez L, et al. Protein intake and lean tissue mass retention following bariatric surgery. Clin Nutr. 2013;32:550–5.
Andreu A, Moizé V, Rodríguez L, et al. Protein intake, body composition, and protein status following bariatric surgery. Obes Surg. 2010;20:1509–15.
Schollenberger AE, Karschin J, Meile T, et al. Impact of protein supplementation after bariatric surgery: A randomized controlled double-blind pilot study. Nutrition. 2016;32:186–92.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient--2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Surg Obes Relat Dis. 2013;9:159–91.
Yumuk V, Tsigos C, Fried M, et al. Toplak H; Obesity Management Task Force of the European Association for the Study of Obesity. European Guidelines for Obesity Management in Adults. Obes Facts. 2015;8:402–24.
Díez I, Martínez C, Sánchez-Santos R, Ruiz JC, Frutos MD, De la Cruz F et al. RecomendacionesRecomendaciones de la SECO para la práctica de la cirugía bariátrica y metabólica (Declaración de Vitoria-Gasteiz,
Thorell A, Hagström-Toft E. Treatment of diabetes prior to and after bariatric surgery. J Diabetes Sci Technol. 2012;6:1226–32.
Panunzi S, Carlsson L, De Gaetano A, et al. Determinants of Diabetes Remission and Glycemic Control After Bariatric Surgery. Diabetes Care. 2016;39:166–74.
Miller GD, Hale E, Dunlap G. Current Evidence for Physical Activity in the Bariatric Surgery Patient for Weight Loss Success. J Obes Weight Loss Ther. 2015;5:274.
Coen PM, Goodpaster BH. A role for exercise after bariatric surgery? Diabetes Obes Metab. 2016;18:16-23. https://doi.org/10.1111/dom.12545. Accessed 31 Jul 2015.
Lecube A, Monereo S, Rubio MÁ, et al. Prevention, diagnosis, and treatment of obesity. 2016 position statement of the Spanish Society for the Study of Obesity. Endocrinol Diabetes Nutr. 2017;64(Suppl 1):15–22.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient-2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Endocr Pract. 2013;19:337–72.
Greestein AJ, O’Rourke RW. Abdominal pain after gastric bypass: suspects and solutions. Am J Surg. 2011;201:819–27.
Sarwer DB, Dilks RJ, West-Smith L. Dietary intake and eating behaviour after bariatric surgery: threats to weight loss maintenance and strategies for success. Surg Obes Relat Dis. 2011;7:644–51.
Pedersen JS, Borup C, Damgaard M, et al. Gadsbøll N Early 24-hour blood pressure response to Roux-en-Y gastric bypass in obese patients. Scand J Clin Lab Invest. 2017;77:53–9.
Benaiges D, Sagué M, Flores-Le Roux JA, et al. Predictors of Hypertension Remission and Recurrence After Bariatric Surgery. Am J Hypertens. 2016;29:653–9.
Sugerman HJ, Brewer WH, Shiffman ML, et al. A multicenter, placebo-controlled, randomized, double-blind, prospective trial of prophylactic ursodiol for the prevention of gallstone formation following gastric-bypass-induced rapid weight loss. Am J Surg. 1995;169:91–6. discussion 96-7
Adams LB, Chang C, Pope J, et al. Randomized, Prospective Comparison of Ursodeoxycholic Acid for the Prevention of Gallstones after Sleeve Gastrectomy. Obes Surg. 2016;26:990–4.
Coupaye M, Calabrese D, Sami O, et al. Evaluation of incidence of cholelithiasis after bariatric surgery in subjects treated or not treated with ursodeoxycholic acid. Surg Obes Relat Dis. 2017;13:681–685.
Abdallah E, Emile SH, Elfeki H, et al. Role of ursodeoxycholic acid in the prevention of gallstone formation after laparoscopic sleeve gastrectomy. Surg Today. 2017;47:844–50.
Stokes CS, Gluud LL, Casper M, et al. Ursodeoxycholic acid and diets higher in fat prevent gallbladder stones during weight loss: a meta-analysis of randomized controlled trials. ClinGastroenterolHepatol. 2014;12:1090–1100.e2.
Uy MC, Talingdan-Te MC, Espinosa WZ, et al. Ursodeoxycholic acid in the prevention of gallstone formation after bariatric surgery: a meta-analysis. Obes Surg. 2008;18:1532–8.
Coblijn UK, Lagarde SM, de Castro SM, et al. The influence of prophylactic proton pump inhibitor treatment on the development of symptomatic marginal ulceration in Roux-en-Y gastric bypass patients: a historic cohort study. Surg Obes Relat Dis. 2016;12:246–52.
Tsirline VB, Keilani ZM, El Djouzi S, et al. How frequently and when do patients undergo cholecystectomy after bariatric surgery? Surg Obes Relat Dis. 2014;10:313–21.
Stenberg E, Szabo E, Ågren G, et al. Closure of mesenteric defects in laparoscopic gastric bypass: a multicentre, randomised, parallel, open-label trial. Lancet. 2016;387:1397–404.
Chang J, Corcelles R, Boules M, et al. Predictive factors of biliary complications after bariatric surgery. Surg Obes Relat Dis. 2016;12:1706–10.
Lockhart ME, Tessler FN, Canon CL, et al. Internal hernia after gastric bypass: sensitivity and specificity of seven CT signs with surgical correlation and controls. AJR Am J Roentgenol. 2007;188:745–50.
Gandhi AD, Patel RA, Brolin RE. Elective laparoscopy for herald symptoms of mesenteric/internal hernia after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2009;5:144–9. discussion 149
Doraiswamy A, Rasmussen JJ, Pierce J, et al. The utility of routine postoperative upper GI series following laparoscopic gastric bypass. Surg Endosc. 2007;21:2159.
White S, Han SH, Lewis C, et al. Selective approach to use of upper gastroesophageal imaging study after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2008;4:122.
Kolakowski Jr S, Kirkland ML, Schuricht AL. Routine postoperative upper gastrointestinal series after Roux-en-Y gastric bypass: determination of whether it is necessary. Arch Surg. 2007;142:930.
Brown WA, Egberts KJ, Franke-Richard D, et al. Erosions after laparoscopic adjustable gastric banding: diagnosis and management. Ann Surg. 2013;257:1047–52.
Dixon JB, Bhasker AG, Lambert GW, et al. Leg to leg bioelectrical impedance analysis of percentage fat mass in obese patients-Can it tell us more than we already know? Surg Obes Relat Dis. 2016;12:1397–402.
Vassilev G, Hasenberg T, Krammer J, et al. The Phase Angle of the Bioelectrical Impedance Analysis as Predictor of Post-Bariatric Weight Loss Outcome. Obes Surg. 2017;27:665–9.
Faria SL, Faria OP, Cardeal MD, et al. Validation study of multi-frequency bioelectrical impedance with dual-energy X-ray absorptiometry among obese patients. Obes Surg. 2014;24:1476–80.
Widen EM, Strain G, King WC, et al. Validity of bioelectrical impedance analysis for measuring changes in body water and percent fat after bariatric surgery. Obes Surg. 2014;24:847–54.
Jiménez A, Omaña W, Flores L, et al. Prediction of whole-body and segmental body composition by bioelectrical impedance in morbidly obese subjects. Obes Surg. 2012;22:587–93.
O'Brien PE, MacDonald L, Anderson M, et al. Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg. 2013;257:87–94.
Sims TL, Mullican MA, Hamilton EC, et al. Routine upper gastrointestinal Gastrografin swallow after laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2003;13:66.
Schiesser M, Guber J, Wildi S, et al. Utility of routine versus selective upper gastrointestinal series to detect anastomotic leaks after laparoscopic gastric bypass. Obes Surg. 2011;21:1238–42.
Courcoulas AP, Yanovski SZ, Bonds D, et al. Long-term outcomes of bariatric surgery: national institutes of health symposium. JAMA Surg. 2014;149:1323–9.
Walsh C, Karmali S. Endoscopic management of bariatric complica¬tions: a review and update. World J Gastrointest Endosc. 2015;7:518–23.
De Roover A, Detry O, Desaive C, et al. Risk of Upper Gastrointestinal Cancer after Bariatric Operations. Obes Surg. 2006;16(12):1656–61.
Schirmer B, Erenoglu C, Miller A. Flexible Endoscopy in the Management of Patients Undergoing Roux-en-Y Gastric Bypass. Obes Surg. 2002;12(5):634–8.
Spinosa SR, Valezi AC. Endoscopic Findings of Asymptomatic Patients One Year After Roux-en-Y Gastric Bypass for Treatment of Obesity. Obes Surg. 2013;23(9):1431–5.
Joo MK. Endoscopic Approach for Major Complications of Bariatric Surgery. Clin Endosc. 2017;50:31–41.
Walsh C, Karmali S. Endoscopic management of bariatric complications: A review and update. World J Gastrointest Endosc. 2015;7:518–23.
Valli PV, Gubler C. Review article including treatment algorithm: endoscopic treatment of luminal complications after bariatric surgery. Clin Obes. 2017;7:115–22.
Stein EM, Silverberg SJ. Bone loss after bariatric surgery: causes, consequences, and management. Lancet Diabetes Endocrinol. 2014;2:165–74.
Rousseau C, Jean S, Gamache P, et al. Change in fracture risk and fracture pattern after bariatric surgery: nested case-control study. BMJ. 2016;354:i3794.
Kim J. Brethauer S; ASMBS Clinical Issues Committee.; American Society for Metabolic and Bariatric Surgery Clinical Issues Committee, Position Statement.. Metabolic bone changes after bariatric surgery. Surg Obes Relat Dis. 2015;11:406–11.
Deitel M, Gawdat K, Melissas J. Reporting weight loss 2007. Obes Surg. 2007;17:565–8.
Baltasar A, Perez N, Serra C, et al. Weight loss reporting: predicted body mass index after bariatric surgery. Obes Surg. 2011;21:367–72.
Vilallonga R, van de Vrande S, Himpens J. Laparoscopic reversal of Roux-en-Y gastric bypass into normal anatomy with or without sleeve gastrectomy. Surg Endosc. 2013;27:4640–8.
Ferraz A, Campos J, Dib V, et al. Food intolerance after banded gastric bypass without stenosis: aggressive endoscopic dilation avoids reoperation. Obes Surg. 2013;23:959–64.
Abu Dayyeh BK, Lautz DB, Thompson CC. Gastrojejunal stoma diameter predicts weight regain after Roux-en-Y gastric bypass. Clin Gastroenterol Hepatol. 2011;9:228–33.
Quigley S, Colledge J, Mukherjee S, et al. Bariatric surgery: A review of normal postoperative anatomy and complications. Clin Radiol. 2011;66:903–14.
Vasas P, Dillemans B, Van Cauwenberge S, et al. Short- and long-term outcomes of vertical banded gastroplasty converted to Roux-en-Y gastric bypass. Obes Surg. 2013;23:241–8.
Marins CJ, Moon RC, Magalhães Neto GEJ, et al. Endoscopic treatment of food intolerance after a banded gastric bypass: inducing band erosion for removal using a plastic stent. Endoscopy. 2016;48:516–20.
Júnior WS, Campos CS, Nonino BS. Reporting results after bariatric surgery: reproducibility of predicted body mass index. Obes Surg. 2012;22:519–22.
Van de Laar A. Bariatric Outcomes Longitudinal Database (BOLD) suggests excess weight loss and excess BMI loss to be inappropriate outcome measures, demonstrating better alternatives. Obes Surg. 2012;22:1843–7.
Sczepaniak JP, Owens ML, Shukla H, et al. Comparability of weight loss reporting after gastric bypass and sleeve gastrectomy using BOLD data 2008-2011. Obes Surg. 2015;25:788–95.
Warschkow R, Tarantino I, Ukegjini K, Beutner U, Güller U, Schmied BM, Müller SA, Schultes B, Thurnheer M. Concomitant cholecystectomy during laparoscopic Rouxen-Y gastric bypass in obese patients is not justified: a meta-analysis. Obes Surg. 2013;23:397–407.
Moon RC, Teixeira AF, DuCoin C, et al. Comparison of cholecystectomy cases after Roux-en-Y gastric bypass, sleeve gastrectomy, and gastric banding. Surg Obes Relat Dis. 2014;10:64–8.
Coblijn UK, Goucham AB, Lagarde SM, et al. Development of ulcer disease after Roux-en-Y gastric bypass, incidence, risk factors, and patient presentation: a systematic review. Obes Surg. 2014;24:299–309.
Sverden E, Mattson F, Sonden A, et al. Risk factors for marginal ulcer after Gastric Bypass Surgery: a population based cohorte. Ann Surg. 2016;263:733–7.
Moon RC, Teixeira AF, Jawad MA. Management and treatment outcomes of marginal ulcers after Roux-en-Y gastric bypass at a single high volume bariatric center. Surg Obes Relat Dis. 2014;10:229–34.
Carr WR, Mahawar KK, Balupuri S, et al. An evidence-based algorithm for the management of marginal ulcers following Roux-en-Y gastric bypass. Obes Surg. 2014;24:1520–7.
Ma P, Reddy S, Higa KD. Curr Atheroscler Rep. 2016;18:42.
Warschkow R, Tarantino I, Ukegjini K, Beutner U, Güller U, Schmied BM, Müller SA, Schultes B, Thurnheer M. Concomitant cholecystectomy during laparoscopic Rouxen-Y gastric bypass in obese patients is not justified: a meta-analysis. Obes Surg. 2013;23:397–407.
Brolin RE, Cody RP. Weight loss outcome of revisional bariatric operations varies according to the primary procedure. Ann Surg. 2008;248:227–32.
Brethauer SA, Kothari S, Sudan R, et al. Systematic review on reoperative bariatric surgery: American Society for Metabolic and Bariatric Surgery Revision Task Force. Surg Obes Relat Dis. 2014;10:952–72.
Management for Failed Bariatric Procedures: Surgical Strategies. New York: Nova Publishers; 2015. J. Himpens & R. Vilallonga (978-1-63483-753-8)
Swartz E, Mobley E, Felix EL. Bile reflux after Roux en Y gastric bypass: an unreconized cause of posoperative pain. Surg Obes Relat Dis. 2009;5:27–30.
Scozari TR, Toppino M, et al. Esophafogastric cancer after bariatric surgery; systematic review of the literature. Surg Obes Relat Dis. 2013;9:133–42.
Mendis S. Global status report on noncommunicable diseases. 2014. Chronic Disease—prevention and control. 2. Chronic Disease—epidemiology. 3.Chronic Disease—mortality. 4. Cost of Illness. 5. Delivery of Health Care. I World Health Organization. ISBN 9789241564854. http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf.
Balibrea JM, Vilallonga R, Hidalgo M, et al. Mid-Term Results and Responsiveness Predictors After Two-Step Single-Anastomosis Duodeno-Ileal Bypass with Sleeve Gastrectomy. Obes Surg. 2017;27:1302–8.
Coakley BA, Deveney CW, Spight DH, Thompson SK, Le D, Jobe BA, Wolfe BM, McConnell DB, O'Rourke RW. Revisional bariatric surgery for failed restrictive procedures. Surg Obes Relat Dis. 2008;4:581–6.
Patel LY, Lapin B, Brown CS, et al. Outcomes following 50 consecutive endoscopic gastrojejunal revisions for weight gain following Roux-en-Y gastric bypass: a comparison of endoscopic suturing techniques for stoma reduction. Surg Endosc. 2017;31:2667–77.
Goldner WS, Stoner JA, Lyden E, et al. Finding the optimal dose of vitamin D following Roux- en-Y gastric bypass: a prospective, randomized pilot clinical trial. Obes Surg. 2009;19:173–9.
Flores L, Moizé V, Ortega E, et al. Prospective study of individualized or high fixed doses of vitamin D supplementation after bariatric surgery. Obes Surg. 2015;25:470–6.
Oria HE, Moorehead MK. Bariatric Analysis and Reporting Outcome System (BAROS). Obes Surg. 1998;8:487–99.
Benedix F, Scheidbach H, Arend J, et al. Revision after failed bariatric surgery--review of complications and current therapeutic options. Zentralbl Chir. 2009;134:214–24. discussion 225
Kolotkin RL, Crosby RD. Psychometric evaluation of the impact of weight on quality of life-lite questionnaire (IWQOL-Lite) in a community simple. Qual Life Res. 2002;11:157–71.
Fort JM, Vilallonga R, Lecube A, et al. Bariatric surgery outcomes in a European Centre of Excellence (CoE). Obes Surg. 2013;23:1324–32. https://doi.org/10.1007/s11695-013-0980-5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest Statement
All authors have no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors and hence ethical approval and informed consent statement did not apply in the article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vilallonga, R., Pereira-Cunill, J., Morales-Conde, S. et al. A Spanish Society joint SECO and SEEDO approach to the Post-operative management of the patients undergoing surgery for obesity. OBES SURG 29, 3842–3853 (2019). https://doi.org/10.1007/s11695-019-04043-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04043-8