Abstract
Introduction
Laparoscopic sleeve gastrectomy is becoming the most commonly performed bariatric surgery. Despite clinical efficacy, adverse events have gradually increase due to its rapid adoption. Sleeve stenosis is the second most common adverse event, occurring in 0.7 to 4% of patients undergoing laparoscopic sleeve gastrectomy (LSG). Endoscopic management with pneumatic balloon dilation (PBD) or stent placement is commonly performed, with a success rate of up to 88%. Recently, Moura et al. (VideoGIE 4(2):68–71, 2018) described a new technique, named as endoscopic tunneled stricturotomy. In this video, we demonstrated the evolution of this technique including full-thickness dissection with staple line disruption.
Methods
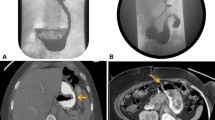
A 28-year-old woman with a BMI of 35.3 kg/m2 who underwent LSG, presented with dysphagia to solid food. An upper GI series showed a stenosis at the level of the incisura angularis. The patient was then referred for endoscopic evaluation.
Results
She underwent three endoscopic PBD in an attempt to treat the stenosis. Unfortunately, her symptoms did not improve. After failed PBD treatment, an endoscopic tunneled stricturotomy with full-thickness dissection was performed. The procedure is performed in 6 steps: (1) identification of the stenosis, (2) submucosal injection 3–5 cm before the stenosis, (3) incision, (4) submucosal tunneling, (5) stricturotomy with full-thickness dissection, and (6) mucosal closure. During follow-up, the patient maintained a 1200-cal diet, without recurrence of symptoms.
Conclusion
Endoscopic tunneled stricturotomy with full-thickness dissection is feasible and appears to be safe and effective in the management of stenosis after sleeve gastrectomy. This procedure may be an option after conventional treatment failure or may be considered as a primary alternative.
Similar content being viewed by others
References
Okazaki O, Bernardo WM, Brunaldi VO, et al. Efficacy and safety of stents in the treatment of fistula after bariatric surgery: a systematic review and meta-analysis. Obes Surg. 2018;28:1788–96.
Agnihotri A, Barola S, Hill C, et al. An algorithmic approach to the management of gastric stenosis following laparoscopic sleeve gastrectomy. Obes Surg. 2017;27(10):2628–36.
de Moura DTH, Jirapinyo P, Aihara H, et al. Endoscopic tunneled stricturotomy in the treatment of stenosis after sleeve gastrectomy. VideoGIE. 2018;4(2):68–71.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Eduardo Guimarães Hourneaux de Moura: Consultant for Boston Scientific and Olympus.
Christopher C. Thompson reports fee as a consultant for Boston Scientific, USGI Medical, Olympus, Fractyl Labs, and Apollo Endosurgery.
All other authors declare that they have no conflict of interest.
Ethical Approval
Institutional Review Board of the Hospital approved the study. Informed consent was obtained from the participant included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(MP4 147,445 kb)
Rights and permissions
About this article
Cite this article
De Moura, E.G.H., de Moura, D.T.H., Sakai, C.M. et al. Endoscopic Tunneled Stricturotomy with Full-Thickness Dissection in the Management of a Sleeve Gastrectomy Stenosis. OBES SURG 29, 2711–2712 (2019). https://doi.org/10.1007/s11695-019-03919-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03919-z