Abstract
Objective
To determine whether vertical sleeve gastrectomy (VSG) attenuates fibrosis in mice on a high-fat high-cholesterol (HFHC) diet.
Background
Bariatric surgery mitigates non-alcoholic steatohepatitis in 85–90% of obese patients. While animal models demonstrate similar results on a high-fat diet, none have observed the effects of bariatric surgery on a combined HFHC diet.
Methods
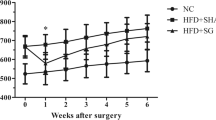
Mice on a HFHC diet were used to confirm the development of hepatic fibrosis at 8 (n = 15) and 24 (n = 15) weeks. A separate cohort of mice on a HFHC diet for 12 weeks was subjected to either VSG (n = 18) or sham (n = 12) operations and remained on a HFHC diet for an additional 20 weeks. Changes in weight, dyslipidemia, and the development of steatosis and fibrosis were documented. Serum was obtained for bile acid analysis by liquid chromatography and mass spectrometry, while hepatic gene expression by RT-PCR was performed to evaluate intrahepatic lipid metabolism.
Results
Hepatic steatosis and fibrosis developed after 8 weeks on the HFHC diet. After VSG, mice demonstrated a sustained decrease in weight with a significant decrease in fibrosis compared to sham mice. Serum total cholesterol, HDL, and LDL were significantly reduced following surgery, while serum bile acids were significantly elevated. Intra-hepatic cholesterol excretion was not upregulated based on hepatic gene expression of CYP7A1 and ABCG5/8.
Conclusions
VSG attenuates the development of hepatic fibrosis in diet-induced obese mice, presumably through enhancement of cholesterol elimination at the intestinal level.






Similar content being viewed by others
References
Jahn D, Rau M, Wohlfahrt J, et al. Non-alcoholic steatohepatitis: from pathophysiology to novel therapies. Dig Dis. 2016;34(4):356–63.
Hales CM, Fryar CD, Carroll MD, et al. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007-2008 to 2015-2016. Jama. 2018;319(16):1723–5.
Mrad RA, Merjaneh N, Mubarak G, et al. The increasing burden of nonalcoholic fatty liver disease among young adults in the United States: a growing epidemic. Hepatology. 2016;64(4):1386–7.
Schwimmer JB, Deutsch R, Kahen T, et al. Prevalence of fatty liver in children and adolescents. Pediatrics. 2006;118(4):1388–93.
Younossi ZM, Koenig AB, Abdelatif D, et al. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84.
Charlton MR, Burns JM, Pedersen RA, et al. Frequency and outcomes of liver transplantation for nonalcoholic steatohepatitis in the United States. Gastroenterology. 2011;141(4):1249–53.
Glass LM, Dickson RC, Anderson JC, et al. Total body weight loss of ≥ 10% is associated with improved hepatic fibrosis in patients with nonalcoholic steatohepatitis. Dig Dis Sci. 2015;60(4):1024–30.
Hannah Jr WN, Harrison SA. Lifestyle and dietary interventions in the management of nonalcoholic fatty liver disease. Dig Dis Sci. 2016;61(5):1365–74.
Burguera B, Agusti A, Arner P, et al. Critical assessment of the current guidelines for the management and treatment of morbidly obese patients. J Endocrinol Investig. 2017;30(10):844–52.
Dixon JB, Bhathal PS, Hughes NR, et al. Nonalcoholic fatty liver disease: improvement in liver histological analysis with weight loss. Hepatology. 2004;39(6):1647–54.
Lassailly G, Caiazzo R, Buob D, et al. Bariatric surgery reduces features of nonalcoholic steatohepatitis in morbidly obese patients. Gastroenterology. 2015;149(2):379–88.
Liou AP, Paziuk M, Luevano Jr JM, et al. Conserved shifts in the gut microbiota due to gastric bypass reduce host weight and adiposity. Sci Transl Med. 2013;5(178):178ra141.
Kohli R, Myronovych A, Tan BK, et al. Bile acid signaling: mechanism for bariatric surgery, cure for NASH? Dig Dis. 2015;33(3):440–6.
Myronovych A, Kirby M, Ryan KK, et al. Vertical sleeve gastrectomy reduces hepatic steatosis while increasing serum bile acids in a weight-loss-independent manner. Obesity (Silver Spring). 2014;22(2):390–400.
Ioannou GN. The role of cholesterol in the pathogenesis of NASH. Trends Endocrinol Metab. 2016;27(2):84–95.
Savard C, Tartaglione EV, Kuver R, et al. Synergistic interaction of dietary cholesterol and dietary fat in inducing experimental steatohepatitis. Hepatology. 2013;57(1):81–92.
Krishnan A, Abdullah TS, Mounajjed T, et al. A longitudinal study of whole body, tissue, and cellular physiology in a mouse model of fibrosing NASH with high fidelity to the human condition. Am J Physiol Gastrointest Liver Physiol. 2017;312(6):G666–g680.
Clapper JR, Hendricks MD, Gu G, et al. Diet-induced mouse model of fatty liver disease and nonalcoholic steatohepatitis reflecting clinical disease progression and methods of assessment. Am J Physiol Gastrointest Liver Physiol. 2013;305(7):G483–95.
Andrikopoulos S, Blair AR, Deluca N, et al. Evaluating the glucose tolerance test in mice. Am J Physiol Endocrinol Metab. 2008;295(6):E1323–32.
Perwaiz S, Tuchweber B, Mignault D, et al. Determination of bile acids in biological fluids by liquid chromatography-electrospray tandem mass spectrometry. J Lipid Res. 2001;42(1):114–9.
Mul JD, Begg DP, Haller AM, et al. MGAT2 deficiency and vertical sleeve gastrectomy have independent metabolic effects in the mouse. Am J Physiolendocrinol Metab. 2014;307(11):E1065–72.
Ryan KK, Tremaroli V, Clemmensen C, et al. FXR is a molecular target for the effects of vertical sleeve gastrectomy. Nature. 2014;509(7499):183–8.
Osland E, Yunus RM, Khan S, et al. Changes in non-diabetic comorbid disease status following laparoscopic vertical sleeve gastrectomy (LVSG) versus laparoscopic roux-En-Y gastric bypass (LRYGB) procedures: a systematic review of randomized controlled trials. Obes Surg. 2017;27(5):1208–21.
Stefater MA, Sandoval DA, Chambers AP, et al. Sleeve gastrectomy in rats improves postprandial lipid clearance by reducing intestinal triglyceride secretion. Gastroenterology. 2011;141(3):939–49.
Temel RE, Brown JM. Biliary and nonbiliary contributions to reverse cholesterol transport. Curr Opin Lipidol. 2012;23(2):85–90.
Vrins CL. From blood to gut: direct secretion of cholesterol via transintestinal cholesterol efflux. World J Gastroenterol. 2010;16(47):5953–7.
Wang B, Tontonoz P. Liver X receptors in lipid signalling and membrane homeostasis. Nat Rev Endocrinol. 2018;14:452–63.
Kruit JK, Plosch T, Havinga R, et al. Increased fecal neutral sterol loss upon liver X receptor activation is independent of biliary sterol secretion in mice. Gastroenterology. 2005;128(1):147–56.
van der Veen JN, van Dijk TH, Vrins CL, et al. Activation of the liver X receptor stimulates trans-intestinal excretion of plasma cholesterol. J Biol Chem. 2009;284(29):19211–9.
Lo Sasso G, Murzilli S, Salvatore L, et al. Intestinal specific LXR activation stimulates reverse cholesterol transport and protects from atherosclerosis. Cell Metab. 2010;12(2):187–93.
Damms-Machado A, Mitra S, Schollenberger AE, et al. Effects of surgical and dietary weight loss therapy for obesity on gut microbiota composition and nutrient absorption. Biomed Res Int. 2015;2015:806248.
Furet JP, Kong LC, Tap J, et al. Differential adaptation of human gut microbiota to bariatric surgery-induced weight loss: links with metabolic and low-grade inflammation markers. Diabetes. 2010;59(12):3049–57.
Palleja A, Kashani A, Allin KH, et al. Roux-en-Y gastric bypass surgery of morbidly obese patients induces swift and persistent changes of the individual gut microbiota. Genome Med. 2016;8(1):67.
Jahansouz C, Staley C, Kizy S, et al. Antibiotic-induced disruption of intestinal microbiota contributes to failure of vertical sleeve gastrectomy. Ann Surg. 2018;2018
Zhang L, Xie C, Nichols RG, et al. Farnesoid X receptor signaling shapes the gut microbiota and controls hepatic lipid metabolism. mSystems. 2016;1(5):00070-16.
Jiang C, Xie C, Li F, et al. Intestinal farnesoid X receptor signaling promotes nonalcoholic fatty liver disease. J Clin Invest. 2015;125(1):386–402.
Nakatani H, Kasama K, Oshiro T, et al. Serum bile acid along with plasma incretins and serum high-molecular weight adiponectin levels are increased after bariatric surgery. Metabolism. 2009;58(10):1400–7.
Patti ME, Houten SM, Bianco AC, et al. Serum bile acids are higher in humans with prior gastric bypass: potential contribution to improved glucose and lipid metabolism. Obesity (Silver Spring). 2009;17(9):1671–7.
Financial Support
The research reported in this publication was financially supported by the Children’s Discovery Institute, Seed Grant Program (EW); NIH (grants R01 DK102110, R01 DK107533, and R01 DK062357; NIH P01 AI120944 (JWKW)); and the Dumont Research Foundation.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
The animal studies were approved by the Institutional Animal Care and Use Committee at UCLA.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Statement
All applicable institutional and/or national guidelines for the care and use of animals were followed.
Informed Consent
Does not apply.
Disclosure
The content is solely the responsibility of all the authors and does not necessarily represent the official views of the Children’s Discovery Institute.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Whang, E., Liu, Y., Kageyama, S. et al. Vertical Sleeve Gastrectomy Attenuates the Progression of Non-Alcoholic Steatohepatitis in Mice on a High-Fat High-Cholesterol Diet. OBES SURG 29, 2420–2429 (2019). https://doi.org/10.1007/s11695-019-03860-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03860-1