Abstract
Background
Insufficient weight loss and weight regain is seen in 20–30% of the post-bariatric population. More knowledge about the effect of physical activity and eating style on weight change after Roux-en-Y gastric bypass is essential since behaviour can be modified and thereby results improved. The goal of this study is to determine the relationship between weight change, self-reported physical activity and eating style.
Methods
Weight, physical activity (PA) and eating style (ES) were assessed before surgery and 15, 24, 36 and 48 months after surgery. A linear mixed model was performed to assess the association between the change in PA and ES and percentage total weight loss (% TWL).
Results
There were 4569 patients included. Preoperative PA and ES were not related to weight change. Change in PA was positively associated with % TWL at 15, 36 and 48 months follow-up. Change in emotional eating was negatively related to % TWL at all follow-up moments. Change in external eating was only negatively related to weight loss at 24 months follow-up. Change in restrained eating was negatively associated with weight loss up to 36 months follow-up. More restrained eating at 36 months follow-up was related to higher weight regain, and more emotional eating at 48 months to 48-month weight regain.
Conclusion
Preoperative self-reported PA and ES did not predict weight change after RYGB. Being are more physically active and showing less emotional and restrained eating was related to a higher weight loss. Emotional and restrained eating were related to higher weight regain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery has proven to effectively treat morbid obesity and its comorbidities [1, 2]. However, in 20–30% of the bariatric population insufficient weight loss (< 50% excess weight loss) or substantial weight regain is observed; both can lead to re-emerging of comorbidities and secondary and/or tertiary bariatric procedures [3,4,4]. Behavioural factors can be modified and thereby reoperations could be avoided. A recent review focussed on the association between behaviour, mainly physical activity and eating, and weight change after bariatric surgery [5]. This review showed that these factors have only been studied sparsely.
Physical activity is considered an important way to achieve weight loss and maintain a healthy weight [6,8,8]. Therefore, bariatric patients are advised to engage in regular physical activity [8,10,11,11]. Previous studies indicate that low physical activity after bariatric surgery is related to less weight loss and more weight regain [12,14,14], though more recent studies question whether weight loss is positively influenced by adherence to a healthy lifestyle with regular physical activity [15, 16].
Self-reported eating styles, like emotional, restrained or external eating, have not been studied frequently in the bariatric population. Emotional eating, in which patients report to eat more in response to emotions, has been linked to less weight loss in two studies [17, 18]. However, others did not support this association [12, 13]. Studies on self-reported external and restrained eating show the same conflicting results; some suggest a negative effect on weight change, while other studies show no effect [12, 13, 17, 19].
In addition to these conflicting results, most of the previous studies, assessing the physical activity and eating style, include small populations and relatively short follow-ups [12, 13, 17, 18]. A longer follow-up is of interest since weight loss plateaus around 18 months after surgery [20].
In the present study, the relationship between weight change and self-reported physical activity and eating style was examined in a large bariatric population (primary RYGB) with a longer follow-up (15, 24, 36 and 48 months). It was hypothesised that patients with better physical activity and better eating styles have higher weight loss and less weight regain.
Methods
Standard Treatment
This is a retrospective analysis of prospectively collected data of patients who were treated at the Nederlandse Obesitas Kliniek (NOK, Dutch Obesity Clinic). Data were collected until 22nd February 2017. The NOK is the largest outpatient clinic for bariatric surgery in the Netherlands, with eight locations throughout the country. In addition to the bariatric procedure, the treatment program entails group counselling by a multidisciplinary team. Group counselling starts before surgery and is focussed on behavioural change. After 15-month follow-up, patients are invited yearly for consultation with the whole multidisciplinary team.
Routine assessment (as part of the treatment program) of self-reported physical activity and eating style was enrolled over the different locations at several time points during 2012 and 2013.
Patients
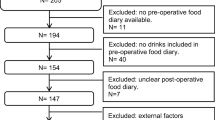
There were 4829 patients who had undergone a primary RYGB between 2012 and 2015 and had a follow-up of 24 months or more were selected from the prospective database. A total of 260 patients (5.6%) patients were excluded because they were lost to follow-up before 12 months post-surgery and/or no results were available for the questionnaires (see below).
Assessments
Physical Activity
Physical activity was evaluated preoperatively (baseline) and at 15, 24, 36 and 48 months after surgery with the Baecke questionnaire [21]. This questionnaire has shown good test-retest reliability and validity, and was used in the bariatric population before [14, 21, 22]. The Baecke consists of 22 questions assessing physical activity at work, during sports and during leisure time. A total score can be calculated, which ranges from 3 to 15, with higher scores indicating increasing self-reported activity. For this analysis, the scores at baseline and follow-up were used. Based on weight loss plateau around 18 months, the maximum change in physical activity (ΔPA) from baseline to 15 or 24 months follow-up was calculated.
Eating Style
Eating style was evaluated at the same time points as the physical activity measurements, using the Dutch Eating Behaviour Questionnaire (DEBQ) [23]. The DEBQ is a widely used questionnaire to measure eating style [23]. It consists of 33 questions assessing three styles of eating: emotional eating, external eating and restrained eating. Emotional eating means eating in response to negative emotions. External eating refers to eating in response to external cues (like seeing food). Restrained eating refers to the intention to eat less. For all subscales, a total score can be calculated. These scores range from 1 to 5; a higher score means the patient indicates being a more emotional, external and/or restrained eater. For the DEBQ score, a maximum change score was also calculated using baseline and 15 or 24 months follow-up scores: ΔEME for change in emotional eating; ΔEXE for change in external eating and ΔREE for change in restrained eating.
Weight Change
Body weight was assessed preoperatively (baseline) and at 12, 15, 24, 36 and 48 months after surgery; height was assessed during preoperative screening. Weight loss was calculated and reported as stated in the most recent guidelines: body mass index (BMI in kg/m2) and percent total weight loss (% TWL) [24]. New variables were created for maximum weight loss and weight regain, since up to date, there are no uniform definitions to report this [3, 25]. First, nadir body weight was defined as the lowest weight up to 24 months post-surgery. Based on that, maximum postoperative weight loss (TWLmax) was calculated using the following formula:
Since weight regain usually develops after the weight plateau, weight regain (WR) was calculated for 36 and 48 months follow-up with the following formulas:
Statistical Analyses
Descriptive statistics were used to summarise patients’ baseline and follow-up characteristics. Changes in body weight and scores of Baecke and DEBQ were analysed using repeated measures ANOVA. Quartiles for preoperative physical activity and eating style were calculated and a MANCOVA analysis was conducted to assess the different weight loss trajectories. Creating weight loss trajectories in four groups ranging from low preoperative physical activity to high preoperative physical activity and four groups ranging from low preoperative emotional, external and restrained eating to high preoperative emotional, external and restrained eating. Plots were created to visualise the differences between these groups. All above analyses were performed using SPSS software, version 23 (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.).
Regression analyses were used to investigate the relationship between baseline self-reported physical activity/eating style and weight change (TWLmax, 36mWR and 48mWR), and between physical activity and eating style at follow-up and weight regain at 36 and 48 months.
A linear mixed model was conducted to assess the association between physical activity and % TWL over all the follow-up moments. This model compared Baecke scoring at the specific follow-up moment with the baseline score, thus focussing on how Baecke scores changed. The relationship between Baecke scores and % TWL over all follow-up moments was assessed using a random intercept, thereby the model takes into account different intercepts for each patient. Then, baseline score, gender and age were added to the model as fixed effects. In the last part of the model, effect modification of time on Baecke was assessed. First calculating if the interaction of Baecke and time had a significant impact on the model and then assessing on which follow-up moments this was. The same model was performed for each of the eating styles (separately). All assumptions for regression analysis were met. These analyses were performed using STATA, version 13 (StataCorp. 2013. Stata 13 Base Reference Manual. College Station, TX: Stata Press.).
Findings were considered statistically significant if the p value was < 0.05.
Results
Study Population
The patients included in the analysis (n = 4569) had a mean age of 47.1 years (± 10.7), which was higher compared to those who were excluded from the analysis (mean age 44.3 (± 11.2), p < 0.001). More females (81.7%) were observed in the included population compared to the excluded population (69.2%, p < 0.001). Mean follow-up (FU) since surgery was 38.7 months (range 24–59 months), which was shorter compared to the excluded population (42.3 months, p < 0.001).
Weight Change
Mean baseline BMI was 44.4 kg/m2 (range 30.3–75.7 kg/m2, Table 1). Mean TWL at 12 months after surgery was 30.8%, at 15 months this was 31.6% and at 24 month 31.4%. Mean TWLmax was 32.7% (±7.9).
Mean TWL was 29.2% at 36-month FU and 27.3% at 48-month FU (p < 0.001). Mean 36 mWR was 5.3% ± 6.7 and the mean 48 mWR was 7.2% ± 9.2 (p < 0.001).
Physical Activity
Mean Baecke scores were lowest before surgery (8.12 ± 1.39) and highest 15 months after surgery, mean score 8.66 ± 1.29 (p < 0.001, Table 2). At 24 months, the mean score was 8.54 ± 1.31, which was significantly lower than the score at 15-month FU (p = 0.042). And at 36-month FU, the mean score was 8.38 ± 1.34, which was lower than the score at 24 months (p = 0.006). Mean maximum change in Baecke score, ΔPA, was 0.76 (range − 6.25 to 7.62).
Eating Style
For emotional eating, the lowest score was observed 15 months after surgery (mean score 1.94 ± 0.77, Table 2). This score was significantly lower compared to the mean score before surgery (2.43 ± 0.82, p < 0.001) and compared to the score at 24 months (2.09 ± 0.78, p < 0.001).
For external eating, the mean score was highest before surgery, 2.84 ± 0.58, and lowest at 15-month FU (2.23 ± 0.56, p < 0.001). There was also a significant difference when comparing scores at 15 and 24-month FU (2.35 ± 0.54, p < 0.001).
For restrained eating, there was only a significant difference when comparing baseline score (3.01 ± 0.60) and score 15 months after surgery (2.49 ± 0.75, p < 0.001). Mean score at 24 months was 2.56 ± 0.75.
Patients reported less emotional eating after surgery, mean maximum change, ΔEME, was − 0.32 (range − 3.54 to 2.39). External eating also decreased after surgery, mean maximum change, ΔEXE, was − 0.61 (range − 3.00 to 1.80). For restrained eating the maximum change, ΔREE, was − 0.53 (range − 3.60 to 3.30).
Preoperative Physical Activity and Eating Style
Preoperative Baecke and DEBQ scores were not related to TWLmax or WR at 36 and 48 months. Figure 1a shows the weight loss trajectories for the four groups of patients based on the quartiles of preoperative Baecke scores, ranging from the group with the lowest physical activity (1st quartile) to the group with the highest physical activity (4th quartile). Weight loss was not significantly different between these groups (p = 0.238). Weight loss trajectories for the four group, based quartiles of preoperative DEBQ scores, are shown in Fig. 1b–d. A lower quartile means a patient has less emotional, restrained or external eating. Weight loss was not significantly different between the four groups for emotional eating (p = 0.699). There was also no significant difference for restrained eating (p = 0.586) and for external eating (p = 0.526).
Weight Regain
Restrained eating at 36 months was significantly, positively related to 36mWR (β = 1.10, p = 0.025). Thus, more restrained eating at 36-month FU was related to higher weight regain. Emotional eating at 48-month FU was significantly, positively related to 48mWR (β = 3.89, p = 0.002); patients who reported more emotional eating 48 months after RYGB, regained more weight. None of the other Baecke and DEBQ scores at 15, 24, 36 and 48 months were related to 36 or 48 months weight regain.
Mixed Model for Physical Activity
There was a significant, positive relationship between change in physical activity and % TWL. Looking at the specific follow-up moments, there was a significant, positive association between physical activity and % TWL at 15 months follow-up (β = 0.22, p = 0.012, Table 3). Patients who engaged in more physical activity at 15-months follow-up had higher weight loss compared to baseline. There was also a significant association at 36 months (β = 0.39, p = 0.002) and 48 months (β = 0.62, p = 0.005). Gender and age did not significantly influence the model; baseline Baecke score did and thus, the aforementioned models were adjusted for the baseline Baecke score.
Mixed Model for Eating Styles
For emotional eating, there was a significant, negative association with % TWL at all follow-up moments, with the most prominent association at 48 months FU (β = −1.66, p = 0.014, Table 3). Patients who experienced more emotional eating compared to baseline had less weight loss.
There was a negative association between external eating and % TWL. Patients who experienced more external eating had less weight loss; this association was only significant at 24 months FU (β = − 1.06, p = 0.003). For restrained eating, there was also a negative association with % TWL; more restrained eating was associated with less weight loss. This association was significant at 15, 24 and 36-month follow-up, while it was not significant at 48 months after surgery. In all eating style models, baseline score of the specific eating style influenced the model, so models were adjusted for baseline score.
Discussion
The goal of this study was to evaluate the effect of physical activity and self-reported eating style on weight change up to 48 months after primary RYGB. The results suggest that patients’ activity and eating style before RYGB are not related to weight loss or weight regain after surgery. In general, patients became more active after surgery and had less emotional, external and restrained eating. Physical activity at 15, 36 and 48 months follow-up was positively associated with weight loss; patients who became more active compared to baseline had higher weight loss. Emotional eating was related to weight loss at all follow-up moments; patients with more emotional eating showed less weight loss. The reporting of more emotional eating at 48 months follow-up was also related to higher weight regain at 48 months. External eating was only related to weight loss at 24 months follow-up; patients who reported more external eating had less weight loss. Restrained eating was negatively associated with weight loss up to 36 months follow-up; patients who reported more restrained eating at follow-up had less weight loss. Patients who experienced more restrained eating at 36 months follow-up also had higher weight regain at this FU moment. Since the mixed model compared scores on the questionnaire with baselines scoring, the model in fact shows that the post-surgery change in physical activity and self-reported eating style was related to weight loss.
Preoperative screening of eligible patients is standard part of bariatric treatment. According to the IFSO criteria, motivation of the patient to follow-up and adherence to, non-specified, behavioural changes is part of the pre-operative assessment [26]. Thus, preoperative behaviour of the patients is, at least partly, used to decide whether a patient is suitable for bariatric surgery. Thereby, it is assumed that current (preoperative) behaviours influence behaviour and weight change after surgery. This has been questioned before [27]. The results of the current study show that preoperative self-reported physical activity and eating style are not related to weight loss or weight regain at any of the follow-up moments. This indicates that questionnaires evaluating physical activity and eating style do not provide information that should be used to decide whether a patient is suitable for bariatric surgery. Preoperative scores did influence the association between changes in physical activity/eating styles and weight loss after surgery and changing of physical activity and eating style should thus be focus of post-operative care.
Like in the non-bariatric population, regular physical activity is advised to all bariatric patients [8,10,11,11]. In previous publications, higher physical activity after surgery was related to better weight loss [28,30,31,32,33,34,34]. In our population, patients who became increasingly active showed higher weight loss at almost all follow-up moments. This has been shown before, even when looking at preoperative change in physical activity [22, 35].
Emotional eating is thought to negatively influence weight loss results, after non-surgical and surgical weight loss treatments [18, 36, 37]. There was a decrease in emotional eating after surgery, this decrease was mostly observed between baseline and 15 months; after that, emotional eating scores gradually increased. The mixed model showed that patients who experienced more emotional eating after surgery had lower weight loss. In addition, at 48-month follow-up, reporting more emotional eating was related to more weight regain. These data do not permit conclusions about causality: self-reported emotional eating might be a factor that contributes to weight regain, though it is also possible that weight regain leads to an increase in emotional eating.
For external and restrained eating, studies assessing the effect on weight loss in bariatric patients are sparse and show conflicting results [12, 13, 17, 19]. In the large population of the current study, higher self-reported restrained eating at 15, 24 and 36 months after RYGB was related with a lower weight loss. Higher restrained eating was also related to more weight regain 36 months after surgery. It was interesting that, like emotional and external eating, restrained eating scores decreased after surgery and that higher restrained had a negative relationship with weight loss. These results again show that self-reported restrained eating seems to reflect intentions to restrain intake instead of actual restrained eating [38]. For external eating, there was only a significant relationship with 24 months weight loss; patients had a higher decrease in external eating lost more weight. Contrary to previous research, in our study, external eating was not related to weight regain [12].
A surprising result was that the mean changes in self-reported physical activity (0.76) and eating styles (− 0.32 to − 0.61) were quite small. Other studies have also shown a small change in physical activity [39]. For eating style, results are hard to compare since this was the first large study using the DEBQ. Other studies, using other questionnaires, show variable results in changes of eating style [12, 19, 40]. We did see a large range in the changes in physical activity and eating style. An explanation for the small changes can be that in our treatment program patients are educated on physical activity and eating styles, patients might overestimate physical activity and underestimate eating style before surgery and, with the education of the program, their own estimations change.
Although we included more than four thousand post-bariatric patients in this longitudinal study, our data cannot be interpreted in a causal way. It could be that an increase in physical activity is causal to an increase in weight loss, but the association might as well be the other way around; a decrease in weight loss facilitating physical activity. Another limitation is the lost to follow-up of 39% and 53% of the patients at respectively 36 and 48-month follow-up. Nonetheless, this is the first study assessing the effect of self-reported physical activity, emotional, external and restrained eating in such a large population with a follow-up until 48 months.
Conclusion
Based on our results, we could argue that success after RYGB is not related to self-reported preoperative physical activity or eating behaviour. Therefore, the decision whether a patient is suitable for surgery should not be made on these self-reports of physical activity and eating style. In addition, professionals working in the bariatric field should be aware that these specific preoperative behaviours are not predictive of results.
Changes in self-reported physical activity, emotional eating and restrained eating and were related to increased weight loss. Future research should study whether changes in self-reported physical activity and/or eating style are causal to weight change after surgery. Lastly, efforts should be made in order to predict which patients will experience weight regain in an earlier stage.
References
Chang SH, Stoll CR, Song J, et al. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003-2012. JAMA Surg. 2014;149(3):275–87.
Courcoulas AP, King WC, Belle SH, Berk P, Flum DR, Garcia L, et al. Seven-year weight trajectories and health outcomes in the longitudinal assessment of bariatric surgery (LABS) study. JAMA Surg. 2018;153(5):427–34.
Karmali S, Brar B, Shi X, et al. Weight recidivism post-bariatric surgery: a systematic review. Obes Surg. 2013;23(11):1922–33.
Kuzminov A, Palmer AJ, Wilkinson S, et al. Re-operations after secondary bariatric surgery: a systematic review. Obes Surg. 2016;26(9):2237–47.
Pinto-Bastos A, Conceicao EM, Machado PPP. Reoperative bariatric surgery: a systematic review of the reasons for surgery, medical and weight loss outcomes, relevant behavioral factors. Obes Surg. 2017;27(10):2707–15.
Swift DL, Johannsen NM, Lavie CJ, et al. The role of exercise and physical activity in weight loss and maintenance. Prog Cardiovasc Dis. 2014;56(4):441–7.
Donnelly JE, Blair SN, Jakicic JM, et al. American College of Sports Medicine position stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41(2):459–71.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient--2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity (Silver Spring). 2013;21(Suppl 1):S1–27.
Faria SL, Faria OP, Buffington C, et al. Dietary protein intake and bariatric surgery patients: a review. Obes Surg. 2011;21(11):1798–805.
van Baak MA, van Mil E, Astrup AV, et al. Leisure-time activity is an important determinant of long-term weight maintenance after weight loss in the Sibutramine trial on obesity reduction and maintenance (STORM trial). Am J Clin Nutr. 2003;78(2):209–14.
van Baak MA. Physical activity and energy balance. Public Health Nutr. 1999;2(3A):335–9.
Amundsen T, Strommen M, Martins C. Suboptimal weight loss and weight regain after gastric bypass surgery-postoperative status of energy intake, eating behavior, physical activity, and psychometrics. Obes Surg. 2017;27(5):1316–23.
Colles SL, Dixon JB, O'Brien PE. Hunger control and regular physical activity facilitate weight loss after laparoscopic adjustable gastric banding. Obes Surg. 2008;18(7):833–40.
Livhits M, Mercado C, Yermilov I, et al. Exercise following bariatric surgery: systematic review. Obes Surg. 2010;20(5):657–65.
Bergh I, Kvalem IL, Mala T, et al. Predictors of physical activity after gastric bypass-a prospective study. Obes Surg. 2017 Aug;27(8):2050–7.
Sherf Dagan S, Keidar A, Raziel A, et al. Do bariatric patients follow dietary and lifestyle recommendations during the first postoperative year? Obes Surg. 2017;27(9):2258–71.
Mathus-Vliegen EM. Long-term health and psychosocial outcomes from surgically induced weight loss: results obtained in patients not attending protocolled follow-up visits. Int J Obes. 2007;31(2):299–307.
Castellini G, Godini L, Amedei SG, Faravelli C, Lucchese M, Ricca V. Psychological effects and outcome predictors of three bariatric surgery interventions: a 1-year follow-up study. Eat Weight Disord. 2014;19(2):217–24.
Konttinen H, Peltonen M, Sjostrom L, et al. Psychological aspects of eating behavior as predictors of 10-y weight changes after surgical and conventional treatment of severe obesity: results from the Swedish obese subjects intervention study. Am J Clin Nutr. 2015;101(1):16–24.
Sjostrom L. Review of the key results from the Swedish obese subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273(3):219–34.
Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36(5):936–42.
Ledoux S, Sami O, Breuil MC, et al. Relevance of self-reported behavioral changes before bariatric surgery to predict success after surgery. Obes Surg. 2017;27(6):1453–9.
van Strien T, Frijters JER, Bergers GPA, et al. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int J Eat Disord. 1986;5(2):295–315.
Brethauer SA, Kim J, El Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Obes Surg. 2015;25(4):587–606.
Nedelcu M, Khwaja HA, Rogula TG. Weight regain after bariatric surgery-how should it be defined? Surg Obes Relat Dis. 2016;12(5):1129–30.
Fried M, Yumuk V, Oppert JM, et al. Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg. 2014;24(1):42–55.
Mahawar KK, Parmar C, Carr WR, et al. Preoperative interventions for patients being considered for bariatric surgery: separating the fact from fiction. Obes Surg. 2015;25(8):1527–33.
Bond DS, Evans RK, Wolfe LG, et al. Impact of self-reported physical activity participation on proportion of excess weight loss and BMI among gastric bypass surgery patients. Am Surg. 2004;70(9):811–4.
Forbush S, Nof L, Echternach J, et al. Influence of activity levels and energy intake on percent excess weight loss after Roux-en-Y gastric bypass. Obes Surg. 2011;21(11):1731–8.
Livhits M, Mercado C, Yermilov I, et al. Behavioral factors associated with successful weight loss after gastric bypass. Am Surg. 2010;76(10):1139–42.
Coleman KJ, Toussi R, Fujioka K. Do gastric bypass patient characteristics, behavior, and health differ depending upon how successful weight loss is defined? Obes Surg. 2010;20(10):1385–92.
Silver HJ, Torquati A, Jensen GL, et al. Weight, dietary and physical activity behaviors two years after gastric bypass. Obes Surg. 2006;16(7):859–64.
Rosenberger PH, Henderson KE, White MA, et al. Physical activity in gastric bypass patients: associations with weight loss and psychosocial functioning at 12-month follow-up. Obes Surg. 2011;21(10):1564–9.
Welch G, Wesolowski C, Piepul B, et al. Physical activity predicts weight loss following gastric bypass surgery: findings from a support group survey. Obes Surg. 2008;18(5):517–24.
Bond DS, Phelan S, Wolfe LG, et al. Becoming physically active after bariatric surgery is associated with improved weight loss and health-related quality of life. Obesity (Silver Spring). 2009;17(1):78–83.
Canetti L, Berry EM, Elizur Y. Psychosocial predictors of weight loss and psychological adjustment following bariatric surgery and a weight-loss program: the mediating role of emotional eating. Int J Eat Disord. 2009;42(2):109–17.
Braden A, Flatt SW, Boutelle KN, et al. Emotional eating is associated with weight loss success among adults enrolled in a weight loss program. J Behav Med. 2016;39(4):727–32.
Jansen A. Eating disorders need more experimental psychopathology. Behav Res Ther. 2016;86:2–10.
Josbeno DA, Jakicic JM, Hergenroeder A, et al. Physical activity and physical function changes in obese individuals after gastric bypass surgery. Surg Obes Relat Dis. 2010;6(4):361–6.
Conceicao EM, Utzinger LM, Pisetsky EM. Eating disorders and problematic eating behaviours before and after bariatric surgery: Characterization, assessment and association with treatment outcomes. Eur Eat Disord Rev. 2015;23(6):417–25.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
For this type of study formal consent is not required.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Monpellier, V.M., Janssen, I.M.C., Antoniou, E.E. et al. Weight Change After Roux-en Y Gastric Bypass, Physical Activity and Eating Style: Is There a Relationship?. OBES SURG 29, 526–533 (2019). https://doi.org/10.1007/s11695-018-3560-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3560-x