Abstract
Aims
There is a lack of population studies evaluating the impact of bariatric surgery (BRS) on all-cause inpatient mortality. We sought to determine the impact of prior BRS on all-cause mortality and healthcare utilization in hospitalized patients.
Methods
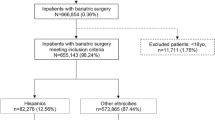
We analyzed the National Inpatient Sample database from 2007 to 2013. Participants were adult (≥ 18 years) inpatients admitted with a diagnosis of morbid obesity or a history of BRS. Propensity score-matched analyses were performed to compare mortality and healthcare resource utilization (hospital length of stay and cost).
Results
There were 9,044,103 patient admissions with morbid obesity and 1,066,779 with prior BRS. A propensity score-matched cohort analysis demonstrated that prior BRS was associated with decreased mortality (OR = 0.58; 95% CI [0.54, 0.63]), shorter length of stay (0.59 days; P < 0.001), and lower hospital costs ($2152; P < 0.001) compared to morbid obesity. A subgroup of propensity score-matched analysis among patients with high-risk of mortality (leading ten causes of mortality in morbid obesity) revealed a consistently significant reduction in odds of mortality for patients with prior BRS (OR = 0.82; 95% CI [0.72, 0.92]).
Conclusion and Relevance
Hospitalized patients with a history of BRS have lower all-cause mortality and healthcare resource utilization compared to those who are morbidly obese. These observations support the continued application of BRS as an effective and resource-conscious treatment for morbid obesity.

Similar content being viewed by others
References
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i-xii, 1–253.
Kuczmarski RJ, Flegal KM. Criteria for definition of overweight in transition: background and recommendations for the United States. Am J Clin Nutr. 2000;72(5):1074–81.
Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet (London, England). 2009;373(9669):1083–96.
Krishna SG, Behzadi J, Hinton A, et al. Effects of bariatric surgery on outcomes of patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2016;14:1001–1010.e5.
O'Brien PE, MacDonald L, Anderson M, et al. Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg. 2013;257(1):87–94.
Maggard MA, Shugarman LR, Suttorp M, et al. Meta-analysis: surgical treatment of obesity. Ann Intern Med. 2005;142(7):547–59.
Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357(8):753–61.
Gloy VL, Briel M, Bhatt DL, et al. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJ (Clin Res Ed). 2013;f5934:347.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Telem DA, Talamini M, Shroyer AL, et al. Long-term mortality rates (>8-year) improve as compared to the general and obese population following bariatric surgery. Surg Endosc. 2015;29(3):529–36.
Arterburn DE, Olsen MK, Smith VA, et al. Association between bariatric surgery and long-term survival. JAMA. 2015;313(1):62–70.
Kwok CS, Pradhan A, Khan MA, et al. Bariatric surgery and its impact on cardiovascular disease and mortality: a systematic review and meta-analysis. Int J Cardiol. 2014;173(1):20–8.
Johnson RJ, Johnson BL, Blackhurst DW, et al. Bariatric surgery is associated with a reduced risk of mortality in morbidly obese patients with a history of major cardiovascular events. Am Surg. 2012;78(6):685–92.
Morgan DJ, Ho KM, Armstrong J, et al. Long-term clinical outcomes and health care utilization after bariatric surgery: a population-based study. Ann Surg. 2015;262(1):86–92.
Lopes EC, Heineck I, Athaydes G, et al. Is bariatric surgery effective in reducing comorbidities and drug costs? A systematic review and meta-analysis. Obes Surg. 2015;25(9):1741–9.
Picot J, Jones J, Colquitt JL, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess (Winchester, England). 2009;13(41):1–190. 215–357, iii-iv
Weiner JP, Goodwin SM, Chang HY, et al. Impact of bariatric surgery on health care costs of obese persons: a 6-year follow-up of surgical and comparison cohorts using health plan data. JAMA Surg. 2013;148(6):555–62.
Bruschi Kelles SM, Machado CJ, Barreto SM. Before-and-after study: does bariatric surgery reduce healthcare utilization and related costs among operated patients? Int J Technol Assess Health Care. 2015;31(6):407–13.
Kalanithi PA, Arrigo R, Boakye M. Morbid obesity increases cost and complication rates in spinal arthrodesis. Spine. 2012;37(11):982–8.
Shamji MF, Parker S, Cook C, et al. Impact of body habitus on perioperative morbidity associated with fusion of the thoracolumbar and lumbar spine. Neurosurgery. 2009;65(3):490–8. discussion 498
Nguyen NT, Masoomi H, Magno CP, et al. Trends in use of bariatric surgery, 2003-2008. J Am Coll Surg. 2011;213(2):261–6.
Parker MH, Berghella V, Nijjar JB. Bariatric surgery and associated adverse pregnancy outcomes among obese women. J Matern Fetal Neonatal Med. 2016;29(11):1747–50.
Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127(8 Pt 2):757–63.
Bergstralh EKJ. Computerized matching of cases to controls technical report series no. 56. 2003.
Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–52.
Nagendran M, Carlin AM, Bacal D, et al. Self-reported remission of obstructive sleep apnea following bariatric surgery: cohort study. Surg Obes Relat Dis. 2015;11(3):697–703.
Kotkiewicz A, Donaldson K, Dye C, et al. Anemia and the need for intravenous iron infusion after Roux-en-Y gastric bypass. Clin Med Insights Blood Disord. 2015;8:9–17.
Coblijn UK, Goucham AB, Lagarde SM, et al. Development of ulcer disease after Roux-en-Y gastric bypass, incidence, risk factors, and patient presentation: a systematic review. Obes Surg. 2014;24(2):299–309.
Capella JF, Capella RF. Gastro-gastric fistulas and marginal ulcers in gastric bypass procedures for weight reduction. Obes Surg. 1999;9(1):22–7. discussion 28
King WC, Chen JY, Mitchell JE, et al. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012;307(23):2516–25.
Conason A, Teixeira J, Hsu CH, et al. Substance use following bariatric weight loss surgery. JAMA Surg. 2013;148(2):145–50.
Funding
This work was funded in part by the Ohio State University College of Medicine Roessler Medical Student Research Scholarship (VR).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
For this type of study, formal consent is not required.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Key Points
Question: Does prior bariatric surgery provide significantly improved inpatient outcomes and healthcare resource utilization compared to comparable and matched patients with morbid obesity?Findings: In this propensity score-matched cohort study of nearly 10 million patients, we found that all-cause inpatient mortality among patients with a history of bariatric surgery was nearly one third the mortality rate for patients with morbid obesity; further, prior bariatric surgery was associated with lower healthcare resource utilization.Meaning: The findings of this study are highly relevant for future research studying the long-term health benefits and cost-effectiveness of bariatric surgery. The observations in this study support the continued application of bariatric surgery as an effective and resource-conscious treatment for morbid obesity.
Electronic Supplementary Material
ESM 1
(DOCX 57 kb)
Rights and permissions
About this article
Cite this article
Krishna, S.G., Rawal, V., Durkin, C. et al. Weight Loss Surgery Reduces Healthcare Resource Utilization and All-Cause Inpatient Mortality in Morbid Obesity: a Propensity-Matched Analysis. OBES SURG 28, 3213–3220 (2018). https://doi.org/10.1007/s11695-018-3345-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3345-2