Abstract
Background
We sought to evaluate the safety and effectiveness of magnetic sphincter augmentation (MSA) in patients with GERD after bariatric surgery.
Methods
Pre- and post-operative GERD quality of life (G-QOL) surveys were conducted. Standard indications (SI) group or the post-bariatric group (PB) created. Outcomes were compared between groups.
Results
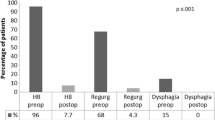
Twenty-eight patients analyzed with no losses to follow-up. All patients had preoperative testing confirming normal motility and presence of GERD. No patients were lost to follow-up. The PB group (N = 10) were mostly prior sleeve gastrectomies (N = 8) with two previous gastric bypasses. PB patients required larger MSA device size (16 beads) compared to the SI group (14 beads, p < 0.001). Outcomes were no different with percent improvement between pre- and post-operative G-QOL survey scores with 70% improvement for PB and 84% for SI (p = 0.13). Medication cessation was possible in 90% for PB versus 94% for SI (p = 0.99). Rates of post-operative dysphagia were similar between the two groups.
Conclusions
Although larger prospective randomized studies are needed, there is an exciting potential for the role of MSA, providing surgeons a new and much needed tool in their armamentarium against refractory or de novo GERD after bariatric procedures.


Similar content being viewed by others
References
Ganz RA, Peters JH, Horgan S. Esophageal sphincter device for gastroesophageal reflux disease. N Engl J Med. 2013;368(21):2039–40.
Bonavina L, Saino G, Bona D, et al. One hundred consecutive patients treated with magnetic sphincter augmentation for gastroesophageal reflux disease: 6 years of clinical experience from a single center. J Am Coll Surg. 2013;217(4):577–85.
Lipham JC, Taiganides PA, Louie BE, et al. Safety analysis of first 1000 patients treated with magnetic sphincter augmentation for gastroesophageal reflux disease. Dis Esophagus. 2015;28(4):305–11.
DuPree CE, Blair K, Steele SR, et al. Laparoscopic sleeve gastrectomy in patients with preexisting gastroesophageal reflux disease: a national analysis. JAMA Surg. 2014;149(4):328–34.
Nagpal AP, Soni H, Haribhakti S. Is oesophageal manometry a must before laparoscopic fundoplication? Analysis of 46 consecutive patients treated without preoperative manometry. J Minim Access Surg. 2010;6(3):66–9.
Hewson EG, Dalton CB, Richter JE. Comparison of esophageal manometry, provocative testing, and ambulatory monitoring in patients with unexplained chest pain. Dig Dis Sci. 1990;35(3):302–9.
Hewson EG, Ott DJ, Dalton CB, et al. Manometry and radiology. Complementary studies in the assessment of esophageal motility disorders. Gastroenterology. 1990;98(3):626–32.
Bonavina L, DeMeester T, Fockens P, et al. Laparoscopic sphincter augmentation device eliminates reflux symptoms and normalizes esophageal acid exposure: one- and 2-year results of a feasibility trial. Ann Surg. 2010;252(5):857–62.
Lipham JC, DeMeester TR, Ganz RA, et al. The LINX(R) reflux management system: confirmed safety and efficacy now at 4 years. Surg Endosc. 2012;26(10):2944–9.
Saino G, Bonavina L, Lipham JC, et al. Magnetic sphincter augmentation for gastroesophageal reflux at 5 Years: final results of a pilot study show long-term acid reduction and symptom improvement. J laparoendosc Adv Surg Tech A. 2015;25(10):787–92.
Kuckelman JP, Phillips CJ, Hardin MO, et al. Standard vs expanded indications for esophageal magnetic sphincter augmentation for reflux disease. JAMA Surg. 2017;152:890–1.
Rona KA, Reynolds J, Schwameis K, et al. Efficacy of magnetic sphincter augmentation in patients with large hiatal hernias. Surg Endosc. 2017;31(5):2096–102.
Kuckelman JP, Barron MR, Martin MJ. “The missing LINX” for gastroesophageal reflux disease: operative techniques video for the Linx magnetic sphincter augmentation procedure. Am J Surg. 2017;213(5):984–7.
Melissas J, Braghetto I, Molina JC, et al. Gastroesophageal reflux disease and sleeve gastrectomy. Obes Surg. 2015;25(12):2430–5.
Soricelli E, Iossa A, Casella G, et al. Sleeve gastrectomy and crural repair in obese patients with gastroesophageal reflux disease and/or hiatal hernia. Surg Obes Relat Dis. 2013;9(3):356–61.
Petersen WV, Meile T, Kuper MA, et al. Functional importance of laparoscopic sleeve gastrectomy for the lower esophageal sphincter in patients with morbid obesity. Obes Surg. 2012;22(3):360–6.
Hendricks L, Alvarenga E, Dhanabalsamy N, et al. Impact of sleeve gastrectomy on gastroesophageal reflux disease in a morbidly obese population undergoing bariatric surgery. Surg Obes Relat Dis. 2016;12(3):511–7.
El-Hadi M, Birch DW, Gill RS, et al. The effect of bariatric surgery on gastroesophageal reflux disease. Cana J Surg J Can Chir. 2014;57(2):139–44.
Altieri MS, Pryor AD. Gastroesophageal reflux disease after bariatric procedures. Surg Clin North Am. 2015;95(3):579–91.
Zhang L, Tan WH, Chang R, et al. Perioperative risk and complications of revisional bariatric surgery compared to primary Roux-en-Y gastric bypass. Surg Endosc. 2015;29(6):1316–20.
Chen RH, Lautz D, Gilbert RJ, et al. Antireflux operation for gastroesophageal reflux after Roux-en-y gastric bypass for obesity. Ann Thorac Surg. 2005;80(5):1938–40.
Desart K, Rossidis G, Michel M, et al. Gastroesophageal reflux management with the LINX(R) system for gastroesophageal reflux disease following laparoscopic sleeve gastrectomy. J Gastrointest Surg. 2015;19(10):1782–6.
Perry Y, Courcoulas AP, Fernando HC, et al. Laparoscopic Roux-en-Y gastric bypass for recalcitrant gastroesophageal reflux disease in morbidly obese patients. JSLS. 2004;8(1):19–23.
Tack J, Deloose E. Complications of bariatric surgery: dumping syndrome, reflux and vitamin deficiencies. Best Pract Res Clin Gastroenterol. 2014;28(4):741–9.
Siilin H, Wanders A, Gustavsson S, et al. The proximal gastric pouch invariably contains acid-producing parietal cells in roux-en-Y gastric bypass. Obes Surg. 2005;15(6):771–7.
Kawahara NT, Alster C, Maluf-Filho F, et al. Modified Nissen fundoplication: laparoscopic antireflux surgery after Roux-en-Y gastric bypass for obesity. Clinics. 2012;67(5):531–3.
Pescarus R, Sharata AM, Dunst CM, et al. Hill procedure for recurrent GERD post-Roux-en-Y gastric bypass. Surg Endosc. 2016;30(5):2141–2.
Hawasli A, Phillips A, Tarboush M. Laparoscopic management of reflux after Roux-en-Y gastric bypass using the LINX system and repair of hiatal hernia: a case report. Surg Obes Relat Dis. 2016;12(5):e51–4.
Mattar SG, Qureshi F, Taylor D, et al. Treatment of refractory gastroesophageal reflux disease with radiofrequency energy (Stretta) in patients after Roux-en-Y gastric bypass. Surg Endosc. 2006;20(6):850–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study. This was performed in conjunction with the pre and post-operative surveys performed.
Statement of Human Rights
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Kuckelman, J.P., Phillips, C.J., Derickson, M.J. et al. Esophageal Magnetic Sphincter Augmentation as a Novel Approach to Post-bariatric Surgery Gastroesophageal Reflux Disease. OBES SURG 28, 3080–3086 (2018). https://doi.org/10.1007/s11695-018-3292-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3292-y