Abstract
Background
Percentage of excess weight loss (%EWL) is the most common metric used after bariatric surgery. However, there has been consistent argument against its use since it varies significantly by initial body mass index (BMI). This study aimed to validate the newly suggested percentage of alterable weight loss (%AWL) metric in Korean patients.
Methods
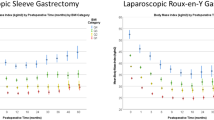
A retrospective review of the prospectively established database at Soonchunhyang University Seoul Hospital identified 165 patients who underwent primary laparoscopic Roux-en-Y gastric bypass (RYGB) and had at least 2-year follow-up weight loss results after surgery. Patients were classified into subgroups based on initial BMI, and their weight loss results expressed as BMI, %EWL, %AWL, and percentage of total weight loss (%TWL) were compared in terms of nadir weight and weight loss trajectory.
Results
The study cohort included 27 male (16.4%) and 138 female (83.6%) patients with a mean baseline BMI of 38.1 ± 5.4. Nadir weight was achieved at mean 24.1 ± 10.6 months postoperatively. Female patients required significantly longer to achieve nadir weight than male patients (16.2 vs. 22.4 months, p = 0.001), and they achieved less weight loss expressed as nadir BMI, %EWL, and %AWL. Of these metrics, only %AWL was not significantly influenced by preoperative BMI and showed the least variation (25.2%) for reporting weight loss.
Conclusion
The AWL metric can report weight loss regardless of baseline BMI in Korean patients undergoing RYGB; however, it must be validated in a larger population involving multiple centers from the Asia-Pacific area before being used clinically.


Similar content being viewed by others
References
Dixon JB, McPhail T, O'Brien PE. Minimal reporting requirements for weight loss: current methods not ideal. Obes Surg. 2005;15(7):1034–1039. PubMed Epub 2005/08/18. eng. https://doi.org/10.1381/0960892054621053.
Oria HE, Carrasquilla C, Cunningham P, et al. Guidelines for weight calculations and follow-up in bariatric surgery. Surg Obes Relat Dis: Off J Am Soc Bariatric Surg. 2005;1(1):67–68. PubMed Epub 2006/08/24. eng. https://doi.org/10.1016/j.soard.2004.12.005.
Deitel M, Gawdat K, Melissas J. Reporting weight loss 2007. Obes Surg. 2007;17(5):565–8. https://doi.org/10.1007/s11695-007-9116-0.
Higa KD, Boone KB, Ho T, et al. Laparoscopic Roux-en-Y gastric bypass for morbid obesity: technique and preliminary results of our first 400 patients. Arch Surg (Chicago, Ill : 1960). 2000;135(9):1029–33. discussion 33-4. PubMed Epub 2000/09/12. eng
Biertho L, Steffen R, Ricklin T, et al. Laparoscopic gastric bypass versus laparoscopic adjustable gastric banding: a comparative study of 1,200 cases. J Am Coll Surg 2003;197(4):536–544; discussion 44-5. PubMed Epub 2003/10/03. eng, doi: https://doi.org/10.1016/S1072-7515(03)00730-0.
Biron S, Hould FS, Lebel S, et al. Twenty years of biliopancreatic diversion: what is the goal of the surgery? Obes Surg. 2004;14(2):160–164. PubMed Epub 2004/03/17. eng. https://doi.org/10.1381/096089204322857492.
Park JY, Kim YJ. Efficacy of laparoscopic sleeve gastrectomy in mildly obese patients with body mass index of 30-35 kg/m(2). Obes Surg. 2015;25(8):1351–1357. PubMed Epub 2015/02/07. eng. https://doi.org/10.1007/s11695-015-1575-0.
Karmali S, Birch DW, Sharma AM. Is it time to abandon excess weight loss in reporting surgical weight loss? Surg Obes Relat Dis: Off J Am Soc Bariatric Surg. 2009;5(4):503–506PubMed Epub 2009/07/28. eng. https://doi.org/10.1016/j.soard.2009.04.014.
Hatoum IJ, Kaplan LM. Advantages of percent weight loss as a method of reporting weight loss after Roux-en-Y gastric bypass. Obesity (Silver Spring, Md). 2013;21(8):1519–25. PubMed Pubmed Central PMCID. Epub 2013/05/15. eng
Brethauer SA, Kim J, el Chaar M, et al. ASMBS Clinical Issues Committee. Standardized outcomes reporting in metabolic and bariatric surgery. Sur Obes Relat Dis: Off J Am Soc Bariatric Surg. 2015;11(3):489–506. PubMed Epub 2015/06/22. eng. https://doi.org/10.1016/j.soard.2015.02.003.
van de Laar AW, Dolle MH, de Brauw LM, et al. Validating the alterable weight loss (AWL) metric with 2-year weight loss outcome of 500 patients after gastric bypass. Obes Surg. 2014;24(7):1085–1089. PubMed Epub 2014/02/25. eng. https://doi.org/10.1007/s11695-014-1203-4.
van de Laar AW. Algorithm for weight loss after gastric bypass surgery considering body mass index, gender, and age from the Bariatric Outcome Longitudinal Database (BOLD). Surg Obes Relat Dis: Off J Am Soc Bariatric Surg. 2014;10(1):55–61. PubMed Epub 2013/10/15. eng. https://doi.org/10.1016/j.soard.2013.05.008.
Park JY, Kim YJ. Laparoscopic Roux-en-Y gastric bypass in obese Korean patients: efficacy and potential adverse events. Surg Today. 2016;46(3):348–355. PubMed Epub 2015/04/29. eng. https://doi.org/10.1007/s00595-015-1170-y.
Organization WH. The Asia-Pacific perspective: redefining obesity and its treatment. Health Communications Australia: Sydney; 2000.
van de Laar AW, de Brauw M, Bruin SC, et al. Weight-independent percentile chart of 2880 gastric bypass patients: a new look at bariatric weight loss results. Obes Surg. 2016;26(12):2891–2898. PubMed Epub 2016/05/04. eng. https://doi.org/10.1007/s11695-016-2200-6.
Park JY, Kim YJ. Reply to the Letter to Editor entitled “the %EBMIL/%EWL double-booby trap. A comment on studies that compare the effect of bariatric surgery between heavier and lighter patients”. Obes Surg. 2016;26(3):614–616. PubMed Epub 2015/12/02. eng. https://doi.org/10.1007/s11695-015-1970-6.
van de Laar AW, de Brauw LM, Meesters EW. Relationships between type 2 diabetes remission after gastric bypass and different weight loss metrics: arguments against excess weight loss in metabolic surgery. Surg Obes Relat Dis: Off J Am Soc Bariatric Surg. 2016;12(2):274–282. PubMed Epub 2015/10/20. eng. https://doi.org/10.1016/j.soard.2015.07.005.
Acknowledgements
This research was supported by the Soonchunhyang University Research Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Informed Consent
The need for patient informed consent for this retrospective study was waived by the institutional review board.
Ethical Approval
This study was approved by the institutional ethics committee of Soonchunhyang University Seoul Hospital and has been performed in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Park, J.Y., Kim, Y.J. Validation of the Alterable Weight Loss Metric in Morbidly Obese Patients Undergoing Gastric Bypass in Korea. OBES SURG 28, 1704–1710 (2018). https://doi.org/10.1007/s11695-017-3084-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-3084-9