Abstract
Background
There is no well-recognized guideline for intraoperative fluid management in bariatric surgery. Goal-directed fluid therapy (GDFT) is a new concept of perioperative fluid management which was shown to improve patients’ prognoses. Dynamic indicators may better predict fluid response compared to static indicators. In this study, we aimed to assess effects of administering GDFT protocol via Pleth Variability Index (PVI) in morbidly obese patients undergoing laparoscopic Roux-en-Y gastric bypass (RYGB) surgery.
Methods
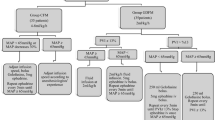
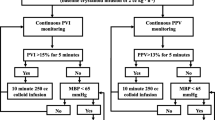
The study included 60 patients who underwent elective laparoscopic RYGB surgery. Subjects were randomized to two groups as being managed with either standard fluid regimen (control group) or PVI (PVI group) during intraoperative period. After induction of general anesthesia, control group received 500 ml crystalloid bolus followed by 4–8 ml/kg/h infusion. Fluid management of the control group was guided by central venous pressure and mean arterial pressure. PVI group received 500 ml crystalloid bolus followed by 2 ml/kg/h infusion. If PVI had been > 14%, 250 ml colloid was administered. Norepinephrine was given by infusion to keep mean arterial pressure > 65 mmHg, if needed. Perioperative lactate levels, hemodynamic parameters, and renal functions were recorded.
Results
In PVI group, volume of crystalloid and total fluid infusion during intraoperative period was significantly lower than the control group (p < 0.05). The groups did not significantly differ in terms of lactate or creatinine levels before or after the surgery (p > 0.05).
Conclusions
There is no need to administer extra volume of fluid to obese patients undergoing laparoscopic bariatric surgery. Use of dynamic indicators like PVI helps to decrease intraoperative volume of infused fluids with no effects on either intraoperative or postoperative lactate levels in laparoscopic bariatric interventions.


Similar content being viewed by others
References
Marik PE, Cavallazzi R. Does the central venous pressure predict fluid responsiveness? An updated meta-analysis and a plea for some common sense. Crit Care Med. 2013;41:1774–81.
Le Manach Y, Hofer CK, Lehot JJ, et al. Can changes in arterial pressure be used to detect changes in cardiac output during volume expansion in the perioperative period? Anesthesiology. 2012;117:1165–74.
Cavallaro F, Sandroni C, Antonelli M. Functional hemodynamic monitoring and dynamic indices of fluid responsiveness. Minerva Anestesiol. 2008;74:123–35.
Cannesson M, Attof Y, Rosamel P, et al. Respiratory variations in pulse oximetry plethysmographic waveform amplitude to predict fluid responsiveness in the operating room. Anesthesiology. 2007;106:1105–11.
Michard F. Changes in arterial pressure during mechanical ventilation. Anesthesiology. 2005;103:419–28.
Michard F, Boussat S, Chemla D, et al. Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med. 2000;162:134–8.
Cannesson M, Slieker J, Desebbe O, et al. The ability of a novel algorithm for automatic estimation of the respiratory variations in arterial pulse pressure to monitor fluid responsiveness in the operating room. Anesth Analg. 2008;106:1195–200.
Cannesson M, Desebbe O, Rosamel P, et al. Pleth variability index to monitor the respiratory variations in the pulse oximeter plethysmographic waveform amplitude and predict fluid responsiveness in the operating theatre. Br J Anaesth. 2008;101:200–6.
Hamilton MA, Cecconi M, Rhodes A. A systematic review and meta-analysis on the use of preemptive hemodynamic intervention to improve postoperative outcomes in moderate and high-risk surgical patients. Anesth Analg. 2011;112:1392–402.
Pearse RM, Harrison DA, MacDonald N, et al. Effect of a perioperative, cardiac output-guided hemodynamic therapy algorithm on outcomes following major gastrointestinal surgery: a randomized clinical trial and systematic review. JAMA. 2014;311:2181–90.
Brienza N, Giglio MT, Marucci M, et al. Does perioperative hemodynamic optimization protect renal function in surgical patients? A meta-analytic study. Crit Care Med. 2009;37:2079–90.
Wyffels PA, Durnez PJ, Helderweirt J, et al. Ventilation-induced plethysmographic variations predict fluid responsiveness in ventilated postoperative cardiac surgery patients. Anesth Analg. 2007;105:448–52.
Dalfino L, Giglio MT, Puntillo F, et al. Haemodynamic goal-directed therapy and postoperative infections: earlier is better. A systematic review and meta-analysis. Crit Care. 2011;15:R154.
Giglio MT, Marucci M, Testini M, et al. Goal-directed haemodynamic therapy and gastrointestinal complications in major surgery: a meta-analysis of randomized controlled trials. Br J Anaesth. 2009;103:637–46.
Grocott MP, Dushianthan A, Hamilton MA, et al. Perioperative increase in global blood flow to explicit defined goals and outcomes after surgery: a Cochrane Systematic Review. Cochrane Database Syst Rev. 2012;11:CD004082.
Jain AK, Dutta A. Stroke volume variation as a guide to fluid administration in morbidly obese patients undergoing laparoscopic bariatric surgery. Obes Surg. 2010;20:709–15.
O’Neill, Allam J. Anaesthetic considerations and management of the obese patient presenting for bariatric surgery. Curr Anaesth Crit Care. 2010;21:16–23.
Lansdorp B, Lemson J, van Putten MJ, et al. Dynamic indices do not predict volume responsiveness in routine clinical practice. Br J Anaesth. 2012;108:395–401.
Michard F, Biais M. Rational fluid management: dissecting facts from fiction. Br J Anaesth. 2012;108:369–71.
Serpa Neto A, Hemmes SN, Barbas CS, et al. Protective versus conventional ventilation for surgery: a systematic review and individual patient data meta-analysis. Anesthesiology. 2015;123:66–78.
Fernandez-Bustamante A, Hashimoto S, Serpa Neto A, et al. Perioperative lung protective ventilation in obese patients. BMC Anesthesiol. 2015;15:56.
Zimmermann M, Feibicke T, Keyl C, et al. Accuracy of stroke volume variation compared with pleth variability index to predict fluid responsiveness in mechanically ventilated patients undergoing major surgery. Eur J Anaesthesiol. 2010;27:555–61.
Corcoran T, Rhodes JE, Clarke S, et al. Perioperative fluid management strategies in major surgery: a stratified meta-analysis. Anesth Analg. 2012;114:640–51.
Gómez-Izquierdo JC, Feldman LS, Carli F, et al. Meta-analysis of the effect of goal-directed therapy on bowel function after abdominal surgery. Br J Surg. 2015;102:577–89.
Abbas SM, Hill AG. Systematic review of the literature for the use of oesophageal Doppler monitor for fluid replacement in major abdominal surgery. Anaesthesia. 2008;63:44–51.
Ripollés J, Espinosa Á, Casans R, et al. Colloids versus crystalloids in objective-guided fluid therapy, systematic review and meta-analysis. Too early or too late to draw conclusions. Braz J Anesthesiol. 2015;65:281–91.
Yates DR, Davies SJ, Milner HE, et al. Crystalloid or colloid for goal-directed fluid therapy in colorectal surgery. Br J Anaesth. 2014;112:281–9.
Nguyen NT, Wolfe BM. The physiologic effects of pneumoperitoneum in the morbidly obese. Ann Surg. 2005;241:219–26.
Wool DB, Lemmens HJ, Brodsky JB, et al. Intraoperative fluid replacement and postoperative creatine phosphokinase levels in laparoscopic bariatric patients. Obes Surg. 2010;20:698–701.
Gustafsson UO, Hausel J, Thorell A, et al. Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Arch Surg. 2011;146:571–7.
Perel A, Minkovich L, Preisman S, et al. Assessing fluid-responsiveness by a standardized ventilatory maneuver: the respiratory systolic variation test. Anesth Analg. 2005;100:942–5.
Lopes MR, Oliveira MA, Pereira VO, et al. Goal-directed fluid management based on pulse pressure variation monitoring during high-risk surgery: a pilot randomized controlled trial. Crit Care. 2007;11:R100.
Cannesson M, Delannoy B, Morand A, et al. Does the Pleth variability index indicate the respiratory-induced variation in the plethysmogram and arterial pressure waveforms? Anesth Analg. 2008;106:1189–94.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the local ethics prior to conduction of the study. The study was approved by the Ethics Committee for Non-Interventional Trials of Firat University.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Demirel, İ., Bolat, E., Altun, A.Y. et al. Efficacy of Goal-Directed Fluid Therapy via Pleth Variability Index During Laparoscopic Roux-en-Y Gastric Bypass Surgery in Morbidly Obese Patients. OBES SURG 28, 358–363 (2018). https://doi.org/10.1007/s11695-017-2840-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2840-1