Abstract
Background
In recent years, several articles have reported considerable results with the Mini/One Anastomosis Gastric Bypass (MGB/OAGB) in terms of both weight loss and resolution of comorbidities. Despite those positive reports, some controversies still limit the widespread acceptance of this procedure. Therefore, a multicenter retrospective study, with the aim to investigate complications following this procedure, has been designed.
Patients and Methods
To report the complications rate following the MGB/OAGB and their management, and to assess the role of this approach in determining eventual complications related especially to the loop reconstruction, in the early and late postoperative periods, the clinical records of 2678 patients who underwent MGB/OAGB between 2006 and 2015 have been studied.
Results
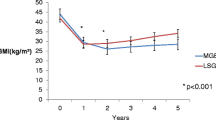
Intraoperative and early complications rates were 0.5 and 3.1%, respectively. Follow-up at 5 years was 62.6%. Late complications rate was 10.1%. A statistical correlation was found for perioperative bleeding both with operative time (p < 0.001) or a learning curve of less than 50 cases (p < 0.001). A statistical correlation was found for postoperative duodenal-gastro-esophageal reflux (DGER) with a preexisting gastro-esophageal-reflux disease (GERD) or with a gastric pouch shorter than 9 cm, (p < 0.001 and p = 0.001), respectively. An excessive weight loss correlated with a biliopancreatic limb longer than 250 cm (p < 0.001).
Conclusions
Our results confirm MGB/OAGB to be a reliable bariatric procedure. According to other large and long-term published series, MGB/OAGB seems to compare very favorably, in terms of complication rate, with two mainstream procedures as standard Roux-en-Y gastric bypass (RYGBP) and laparoscopic sleeve gastrectomy (LSG).




Similar content being viewed by others
References
Rutledge R. The mini gastric bypass: experience with the first 1274 cases. Obes Surg. 2001;11:276–80.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25:1822–32.
Deitel M. Letter to the editor: bariatric surgery worldwide 2013 reveals a rise in mini gastric bypass. Obes Surg. 2015;25:2165.
Lee WJ, Ser KH, Lee YC, et al. Laparoscopic Roux-en-Y vs. mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg. 2012;22:1827–34.
Musella M, Susa A, Greco F, et al. The laparoscopic mini-gastric bypass: the Italian experience: outcomes from 974 consecutive cases in a multicenter review. Surg Endosc. 2014;28:156–63.
Chevallier JM, Arman GA, Guenzi M, et al. One thousand single anastomosis (omega loop) gastric bypasses to treat morbid obesity in a 7-year period: outcomes show few complications and good efficacy. Obes Surg. 2015;25:951–8.
Musella M, Milone M. Still “controversies” about the mini gastric bypass? Obes Surg. 2014;24:643–4.
www.ifso.com/one-anastomosis-gastric-bypass as Accessed 23 Nov 2016.
www.sicob.org as Accessed 23 Nov 2016.
Vakil N, van Zanten SV, Kahrilas P, et al., Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–20.
Sifrim D. Management of bile reflux. Gastroenterol Hepatol (NY). 2013;9(3):179–80.
Vaezi MF, Richter JE. Duodenogastroesophageal reflux and methods to monitor nonacidic reflux. Am J Med. 2001;111(Suppl 8A):160S–8S.
Carbajo M, García-Caballero M, Toledano M, et al. One-anastomosis gastric bypass by laparoscopy: results of the first 209 patients. Obes Surg. 2005;15:398–404.
Dindo D, Demartines S, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Musella M, Apers J, Rheinwalt K, et al. Efficacy of bariatric surgery in type 2 diabetes mellitus remission: the role of mini gastric bypass/one anastomosis gastric bypass and sleeve gastrectomy at 1 year of follow-up. A European survey. Obes Surg. 2016;26(5):933–40.
Fisher BL, Buchwald H, Clark W, et al. Mini-gastric bypass controversy. Obes Surg. 2001;11:773–7.
Johnson WH, Fernanadez AZ, Farrell TM, et al. Surgical revision of loop (“mini”) gastric bypass procedure: multicenter review of complications and conversions to Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2007;3:37–41.
Collins BJ, Miyashita T, Schweitzer M, et al. Gastric bypass why Roux-en-Y? A review of experimental data. Arch Surg. 2007;142:1000–3.
Mahawar KK, Carr WR, Balupuri S, et al. Controversy surrounding “mini” gastric bypass. Obes Surg. 2014;24:324–33.
Victorzon M. Single-anastomosis gastric bypass: better, faster, and safer? Scand J Surg. 2015;104:48–53.
Lee WJ, Chong K, Ser KH, et al. Gastric bypass vs sleeve gastrectomy for type 2 diabetes mellitus: a randomized controlled trial. Arch Surg. 2011;146(2):143–8.
Lee WJ, Lin YH. Single-anastomosis gastric bypass (SAGB): appraisal of clinical evidence. Obes Surg. 2014;24:1749–56.
Kular KS, Manchanda N, Rutledge R. A 6-year experience with 1,054 mini-gastric bypasses-first study from Indian subcontinent. Obes Surg. 2014;24:1430–5.
Bruzzi M, Rau C, Voron T, et al. Single anastomosis or mini-gastric bypass: long-term results and quality of life after a 5-year follow-up. Surg Obes Relat Dis. 2015;11:321–6.
Gagner M, Deitel M, Erickson AL, et al. Survey on laparoscopic sleeve gastrectomy (LSG) at the Fourth International Consensus Summit on Sleeve Gastrectomy. Obes Surg. 2013;23:2013–7.
Stenberg E, Szabo E, Agren G, et al., Scandinavian Obesity Surgery Registry Study Group. Early complications after laparoscopic gastric bypass surgery: results from the Scandinavian Obesity Surgery Registry. Ann Surg. 2014;260:1040–7.
Greenstein AJ, Wahed AS, Adeniji A, et al. Prevalence of adverse intraoperative events during obesity surgery and their sequelae. J Am Coll Surg. 2012;215:271–7.e3.
Higa K, Ho T, Tercero F, et al. Laparoscopic Roux-en-Y gastric bypass: 10-year follow-up. Surg Obes Relat Dis. 2011;7:516–25.
Hutter MM, Schirmer BD, Jones DB, et al. First report from the American College of Surgeons Bariatric Surgery Center Network: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann Surg. 2011;254:410–22.
Boza C, Gamboa C, Salinas J, et al. Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy: a case-control study and 3 years of follow-up. Surg Obes Relat Dis. 2012;8:243–9.
Obeid A, Long J, Kakade M, et al. Laparoscopic Roux-en-Y gastric bypass: long-term clinical outcomes. Surg Endosc. 2012;26:3515–20.
Fridman A, Moon R, Cozacov Y, et al. Procedure-related morbidity in bariatric surgery: a retrospective short- and mid-term follow-up of a single institution of the American College of Surgeons Bariatric Surgery Centers of Excellence. J Am Coll Surg. 2013;217:614–20.
Mehaffey JH, LaPar DJ, Clement KC, et al. 10-Year outcomes after Roux-en-Y gastric bypass. Ann Surg. 2016;264:121–6.
Zhang Y, Wang J, Sun X, et al. Laparoscopic sleeve gastrectomy versus laparoscopic Roux-en-Y gastric bypass for morbid obesity and related comorbidities: a meta-analysis of 21 studies. Obes Surg. 2015;25:19–26.
Rausa E, Bonavina L, Asti E, et al. Rate of death and complications in laparoscopic and open Roux-en-Y gastric bypass. A meta-analysis and meta-regression analysis on 69,494 patients. Obes Surg. 2016;26:1956–63.
Sverdén E, Mattsson F, Sondén A, et al. Risk factors for marginal ulcer after gastric bypass surgery for obesity: a population-based cohort study. Ann Surg. 2016;263:733–7.
Carbajo MA, Luque-de-León E, Jiménez JM, Ortiz-de-Solórzano J, Pérez-Miranda M, Castro-Alija MJ Laparoscopic one-anastomosis gastric bypass: technique, results, and long-term follow-up in 1200 patients. Obes Surg 2016.
Tran TB, Worhunsky DJ, Squires MH, et al. To Roux or not to Roux: a comparison between Roux-en-Y and Billroth II reconstruction following partial gastrectomy for gastric cancer. Gastric Cancer. 2016;19:994–1001.
Csendes A, Burgos AM, Smok G, et al. Latest results (12-21 years) of a prospective randomized study comparing Billroth II and Roux-en-Y anastomosis after a partial gastrectomy plus vagotomy in patients with duodenal ulcers. Ann Surg. 2009;249:189–94.
Tolone S, Cristiano S, Savarino E, et al. Effects of omega-loop bypass on esophagogastric junction function. Surg Obes Relat Dis. 2016;12:62–9.
Hendricks L, Alvarenga E, Dhanabalsamy N, et al. Impact of sleeve gastrectomy on gastroesophageal reflux disease in a morbidly obese population undergoing bariatric surgery. Surg Obes Relat Dis. 2016;12:511–7.
DuPree CE, Blair K, Steele SR, et al. Laparoscopic sleeve gastrectomy in patients with preexisting gastroesophageal reflux disease: a national analysis. JAMA Surg. 2014;149:328–34.
Arman GA, Himpens J, Dhaenens J, et al. Long-term (11+years) outcomes in weight, patient satisfaction, comorbidities, and gastroesophageal reflux treatment after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2016; doi:10.1016/j.soard.2016.01.013.
Oor JE, Roks DJ, Ünlü Ç, et al. Laparoscopic sleeve gastrectomy and gastroesophageal reflux disease: a systematic review and meta-analysis. Am J Surg. 2016;211:250–67.
Pradarelli JC, Varban OA, Dimick JB. Hospital variation in rates of acid-reducing medication use after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2016;12:1382–9.
Facchiano E, Leuratti L, Veltri M, et al. Laparoscopic conversion of one anastomosis gastric bypass to Roux-en-Y gastric bypass for chronic bile reflux. Obes Surg. 2016;26:701–3.
Nimeri A, Al Shaban T, Maasher A. Laparoscopic conversion of one anastomosis gastric bypass/mini gastric bypass to Roux-en-Y gastric bypass for bile reflux gastritis. Surg Obes Relat Dis. 2017;13:119–21.
Musella M, Milone M, Deitel M, et al. What a mini/one anastomosis gastric bypass (MGB/OAGB) is. Obes Surg. 2016;26:1322–3.
Caygill CP, Hill MJ, Kirkham JS, et al. Mortality from gastric cancer following gastric surgery for peptic ulcer. Lancet. 1986;1(8487):929–31.
Viste A, Bjørnestad E, Opheim P, et al. Risk of carcinoma following gastric operations for benign disease. A historical cohort study of 3470 patients. Lancet. 1986;2(8505):502–5.
Lundegårdh G, Adami HO, Helmick C, et al. Stomach cancer after partial gastrectomy for benign ulcer disease. N Engl J Med. 1988;319:195–200.
Ito M, Takata S, Tatsugami M, et al. Clinical prevention of gastric cancer by Helicobacter pylori eradication therapy: a systematic review. J Gastroenterol. 2009;44:365–71.
Rutledge R, Walsh W. Continued excellent results with the mini-gastric bypass: six-year study in 2410 patients. Obes Surg. 2005;15:1304–8.
Wu CC, Lee WJ, Ser KH, et al. Gastric cancer after mini-gastric bypass surgery: a case report and literature review. Asian J Endosc Surg. 2013;6:303–6.
Scozzari G, Trapani R, Toppino M, et al. Esophagogastric cancer after bariatric surgery: systematic review of the literature. Surg Obes Relat Dis. 2013;9:133–42.
Angrisani L, Santonicola A, Iovino P. Gastric cancer: a de novo diagnosis after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2014;10:186–7.
Cavin JB, Voitellier E, Cluzeaud F, et al. Malabsorption and intestinal adaptation after one anastomosis gastric bypass compared with Roux-en-Y gastric bypass in rats. Am J Physiol Gastrointest Liver Physiol. 2016;311:G492–500.
Bétry C, Disse E, Chambrier C, et al. Need for intensive nutrition care after bariatric surgery: is mini gastric bypass at fault? JPEN J Parenter Enteral Nutr. 2016;41:258–62.
Jammu GS, Sharma R. A 7-year clinical audit of 1107 cases comparing sleeve gastrectomy, Roux-En-Y gastric bypass, and mini-gastric bypass, to determine an effective and safe bariatric and Metabolic procedure. Obes Surg. 2016;26:926–32.
Lee WJ, Lee YC, Ser KH, et al. Revisional surgery for laparoscopic minigastric bypass. Surg Obes Relat Dis. 2011;7:486–91.
Lee WJ, Wang W, Lee YC, et al. Laparoscopic mini-gastric bypass: experience with tailored bypass limb according to body weight. Obes Surg. 2008;18:294–9.
Acknowledgements
The authors would like to acknowledge Prof. Maurizio Taglialatela for his precious help in drafting this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Although an “ethical approval” statement does not apply to a retrospective study, it has to be remarked that all MGB/OAGB procedures performed by authors were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Informed Consent
An informed consent to surgery was obtained from all patients who underwent an MGB/OAGB procedure performed by anyone of the authors of this study during these years.
Rights and permissions
About this article
Cite this article
Musella, M., Susa, A., Manno, E. et al. Complications Following the Mini/One Anastomosis Gastric Bypass (MGB/OAGB): a Multi-institutional Survey on 2678 Patients with a Mid-term (5 Years) Follow-up. OBES SURG 27, 2956–2967 (2017). https://doi.org/10.1007/s11695-017-2726-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2726-2