Abstract
Background
Roux-en-Y gastric bypass (RYGB) is an effective treatment for patients with type 2 diabetes mellitus (T2D) with obesity. However, T2D remission after surgery has not been adequately studied in Chinese patients with different obesity classes. The purpose of this study is to evaluate the medium-term metabolic results of RYGB in T2D patients with body mass index (BMI) >25 kg/m2 compared by obesity class.
Methods
We retrospectively divided 120 Chinese patients with T2D and BMI >25 kg/m2 into four groups from overweight to obesity class III and reviewed their medical records for metabolic outcomes 36 months after RYGB. T2D remission was defined as glycated hemoglobin <6.0 % and no current medications. Hypertension, dyslipidemia, cardiovascular risk, and medications were also evaluated.
Results
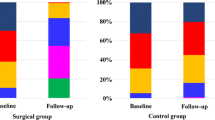
Sixty-two patients (62/120, 51.6 %) were female. All surgeries were performed laparoscopically without mortality or major complications. Mean follow-up duration was 38.7 ± 9.1 months and follow-up compliance was 86.7 %. Patients with BMI ≥28 kg/m2 benefitted more from weight loss following RYGB. Medication and remission results for hypertension and dyslipidemia did not differ significantly between groups. There was a significant reduction in the need for oral medication or insulin in all four groups. T2D remission occurred in 44–66.7 % of all patients at 36 months with no significant difference between groups. Initial BMI was correlated with A1C 36 months after surgery (r = −0.217, P = 0.027).
Conclusions
RYGB effectively treated T2D patients in our study, even in low-BMI patients, and resulted in diabetes remission and metabolic disorder control, reducing cardiovascular risk.


Similar content being viewed by others
References
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122(3):248–56.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370(21):2002–13.
Dixon JB, Zimmet P, Alberti KG, et al. Bariatric surgery: an IDF statement for obese type 2 diabetes. International Diabetes Federation Taskforce on Epidemiology and Prevention. Surg Obes Relat Dis. 2011;7(4):433–47.
Rubino F, Kaplan LM, Schauer PR, et al. The Diabetes Surgery Summit consensus conference: recommendations for the evaluation and use of gastrointestinal surgery to treat type 2 diabetes mellitus. Ann Surg. 2010;251(3):399–405.
Lee WJ, Hur KY, Lakadawala M, et al. Predicting success of metabolic surgery: age, body mass index, C-peptide, and duration score. Surg Obes Relat Dis. 2013;9(3):379–84.
Cohen RV, Pinheiro JC, Schiavon CA, et al. Effects of gastric bypass surgery in patients with type2 diabetes and only mild obesity. Diabetes Care. 2012;35(7):1420–8.
Malapan K, Goel R, Tai CM, et al. Laparoscopic Roux-en-Y gastric bypass for nonobese type II diabetes mellitus in Asian patients. Surg Obes Relat Dis. 2014;10(5):834–40.
Vetter ML, Cardillo S, Rickels MR, et al. Narrative review: effect of bariatric surgery on type 2 diabetes mellitus. Ann Intern Med. 2009;150(2):94–103.
Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in Chinese adults. J Am Med Assoc. 2013;310(9):948–59.
Yu H, Di J, Bao Y, et al. Visceral fat area as a new predictor of short-term diabetes remission after Roux-en-Y gastric bypass surgery in Chinese patients with a body mass index less than 35 kg/m2. Surg Obes Relat Dis. 2015;11(1):6–11.
Chen C, Lu FC. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci. 2004;17(Suppl):1–36.
Brethauer SA, Kim J, el Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11(3):489–506.
Sjöström L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93.
Huang CK, Shabbir A, Lo CH, et al. Laparoscopic Roux-en-Y gastric bypass for the treatment of type II diabetes mellitus in Chinese patients with body mass index of 25–35. Obes Surg. 2011;21(9):1344–9.
Dixon JB, Chuang LM, Chong K, et al. Predicting the glycemic response to gastric bypass surgery in patients with type 2 diabetes. Diabetes Care. 2013;36:20–6.
Lee WJ, Chong K, Chen JC, et al. Predictors of diabetes remission after bariatric surgery in Asia. Asian J Surg. 2012;35(2):67–73.
Puzziferri N, Roshek 3rd TB, Mayo HG, et al. Long-term follow-up after bariatric surgery: a systematic review. J Am Med Assoc. 2014;312(9):934–42.
Ribaric G, Buchwald JN, McGlennon TW. Diabetes and weight in comparative studies of bariatric surgery vs conventional medical therapy: a systematic review and meta-analysis. Obes Surg. 2014;24(3):437–55.
Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5.
Vidal P, Ramón JM, Goday A, et al. Lack of adherence to follow-up visits after bariatric surgery: reasons and outcome. Obes Surg. 2014;24(2):179–83.
Acknowledgments
This study was supported by grants from scientific research funds of the Shanghai Jiao Tong University Affiliated Sixth People’s Hospital (1642), the Chinese Society of Endocrinology, Key Program of the Shanghai Municipality for Basic Research (11 JC1409600), 973 program (2011 CB504001), and the National Major Scientific and Technological Special Project for “Significant New Drugs Development” (2011 ZX09307–001–02).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
For this type of study, formal consent is not required.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Hongwei Zhang and Xiaodong Han contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhang, H., Han, X., Yu, H. et al. Effect of Roux-en-Y Gastric Bypass on Remission of T2D: Medium-Term Follow-up in Chinese Patients with Different BMI Obesity Class. OBES SURG 27, 134–142 (2017). https://doi.org/10.1007/s11695-016-2262-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-016-2262-5