Abstract
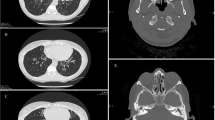
Primary ciliary dyskinesia (PCD) is a highly heterogeneous recessive inherited disorder. FAP54, the homolog of CFAP54 in Chlamydomonas reinhardtii, was previously demonstrated as the C1d projection of the central microtubule apparatus of flagella. A Cfap54 knockout mouse model was then reported to have PCD-relevant phenotypes. Through whole-exome sequencing, compound heterozygous variants c.2649_2657delinC (p. E883Dfs*47) and c.7312_7313insCGCAGGCTGAATTCTTGG (p. T2438delinsTQAEFLA) in a new suspected PCD-relevant gene, CFAP54, were identified in an individual with PCD. Two missense variants, c.4112A>C (p. E1371A) and c.6559C>T (p. P2187S), in CFAP54 were detected in another unrelated patient. In this study, a minigene assay was conducted on the frameshift mutation showing a reduction in mRNA expression. In addition, a CFAP54 in-frame variant knock-in mouse model was established, which recapitulated the typical symptoms of PCD, including hydrocephalus, infertility, and mucus accumulation in nasal sinuses. Correspondingly, two missense variants were deleterious, with a dramatic reduction in mRNA abundance from bronchial tissue and sperm. The identification of PCD-causing variants of CFAP54 in two unrelated patients with PCD for the first time provides strong supportive evidence that CFAP54 is a new PCD-causing gene. This study further helps expand the disease-associated gene spectrum and improve genetic testing for PCD diagnosis in the future.
Similar content being viewed by others
References
Mirra V, Werner C, Santamaria F. Primary ciliary dyskinesia: an update on clinical aspects, genetics, diagnosis, and future treatment strategies. Front Pediatr 2017; 5: 135
Zariwala MA, Knowles MR, Leigh MW. Primary Ciliary Dyskinesia. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Stephens K, Amemiya A. GeneReviews. Seattle (WA): University of Washington, 1993
Kurkowiak M, Zietkiewicz E, Witt M. Recent advances in primary ciliary dyskinesia genetics. J Med Genet 2015; 52(1): 1–9
Yoshiba S, Shiratori H, Kuo IY, Kawasumi A, Shinohara K, Nonaka S, Asai Y, Sasaki G, Belo JA, Sasaki H, Nakai J, Dworniczak B, Ehrlich BE, Pennekamp P, Hamada H. Cilia at the node of mouse embryos sense fluid flow for left-right determination via Pkd2. Science 2012; 338(6104): 226–231
Knowles MR, Zariwala M, Leigh M. Primary ciliary dyskinesia. Clin Chest Med 2016; 37(3): 449–461
Lucas JS, Davis SD, Omran H, Shoemark A. Primary ciliary dyskinesia in the genomics age. Lancet Respir Med 2020; 8(2): 202–216
Horani A, Ferkol TW. Understanding primary ciliary dyskinesia and other ciliopathies. J Pediatr 2021; 230: 15–22.e1
Brown JM, Dipetrillo CG, Smith EF, Witman GBA. A FAP46 mutant provides new insights into the function and assembly of the C1d complex of the ciliary central apparatus. J Cell Sci 2012; 125 (Pt 16): 3904–3913
Takeuchi K, Kitano M, Ishinaga H, Kobayashi M, Ogawa S, Nakatani K, Masuda S, Nagao M, Fujisawa T. Recent advances in primary ciliary dyskinesia. Auris Nasus Larynx 2016; 43(3): 229–236
Mitchell DR, Smith B. Analysis of the central pair microtubule complex in Chlamydomonas reinhardtii. Methods Cell Biol 2009; 92: 197–213
Pazour GJ, Agrin N, Leszyk J, Witman GB. Proteomic analysis of a eukaryotic cilium. J Cell Biol 2005; 170(1): 103–113
DiPetrillo CG, Smith EF. Pcdp1 is a central apparatus protein that binds Ca2+-calmodulin and regulates ciliary motility. J Cell Biol 2010; 189(3): 601–612
McKenzie CW, Craige B, Kroeger TV, Finn R, Wyatt TA, Sisson JH, Pavlik JA, Strittmatter L, Hendricks GM, Witman GB, Lee L. CFAP54 is required for proper ciliary motility and assembly of the central pair apparatus in mice. Mol Biol Cell 2015; 26(18): 3140–3149
Li H, Durbin R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 2009; 25(14): 1754–1760
Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, Homer N, Marth G, Abecasis G, Durbin R; 1000 Genome Project Data Processing Subgroup. The Sequence Alignment/Map format and SAMtools. Bioinformatics 2009; 25(16): 2078–2079
1000 Genomes Project Consortium; Auton A, Brooks LD, Durbin RM, Garrison EP, Kang HM, Korbel JO, Marchini JL, McCarthy S, McVean GA, Abecasis GR. A global reference for human genetic variation. Nature 2015; 526(7571): 68–74
Karczewski KJ, Francioli LC, Tiao G, Cummings BB, Alföldi J, Wang Q, Collins RL, Laricchia KM, Ganna A, Birnbaum DP, Gauthier LD, Brand H, Solomonson M, Watts NA, Rhodes D, Singer-Berk M, England EM, Seaby EG, Kosmicki JA, Walters RK, Tashman K, Farjoun Y, Banks E, Poterba T, Wang A, Seed C, Whiffin N, Chong JX, Samocha KE, Pierce-Hoffman E, Zappala Z, O’Donnell-Luria AH, Minikel EV, Weisburd B, Lek M, Ware JS, Vittal C, Armean IM, Bergelson L, Cibulskis K, Connolly KM, Covarrubias M, Donnelly S, Ferriera S, Gabriel S, Gentry J, Gupta N, Jeandet T, Kaplan D, Llanwarne C, Munshi R, Novod S, Petrillo N, Roazen D, Ruano-Rubio V, Saltzman A, Schleicher M, Soto J, Tibbetts K, Tolonen C, Wade G, Talkowski ME; Genome Aggregation Database Consortium; Neale BM, Daly MJ, MacArthur DG. The mutational constraint spectrum quantified from variation in 141 456 humans. Nature 2020; 581(7809): 434–443
Fu W, O’Connor TD, Jun G, Kang HM, Abecasis G, Leal SM, Gabriel S, Rieder MJ, Altshuler D, Shendure J, Nickerson DA, Bamshad MJ; NHLBI Exome Sequencing Project; Akey JM. Analysis of 6515 exomes reveals the recent origin of most human protein-coding variants. Nature 2013; 493(7431): 216–220
Wang K, Li M, Hakonarson H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res 2010; 38(16): e164
Kumar P, Henikoff S, Ng PC. Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat Protoc 2009; 4(7): 1073–1081
Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P, Kondrashov AS, Sunyaev SR. A method and server for predicting damaging missense mutations. Nat Methods 2010; 7(4): 248–249
Schwarz JM, Rödelsperger C, Schuelke M, Seelow D. MutationTaster evaluates disease-causing potential of sequence alterations. Nat Methods 2010; 7(8): 575–576
Kircher M, Witten DM, Jain P, O’Roak BJ, Cooper GM, Shendure J. A general framework for estimating the relative pathogenicity of human genetic variants. Nat Genet 2014; 46(3): 310–315
Amberger JS, Hamosh A. Searching Online Mendelian Inheritance in Man (OMIM): a knowledgebase of human genes and genetic phenotypes. Curr Protoc Bioinformatics 2017; 58: 1.2.1–1.2.12
Kanehisa M, Goto S. KEGG: kyoto encyclopedia of genes and genomes. Nucleic Acids Res 2000; 28(1): 27–30
Landrum MJ, Lee JM, Benson M, Brown G, Chao C, Chitipiralla S, Gu B, Hart J, Hoffman D, Hoover J, Jang W, Katz K, Ovetsky M, Riley G, Sethi A, Tully R, Villamarin-Salomon R, Rubinstein W, Maglott DR. ClinVar: public archive of interpretations of clinically relevant variants. Nucleic Acids Res 2016; 44(D1): D862–D868
Schaefer CF, Anthony K, Krupa S, Buchoff J, Day M, Hannay T, Buetow KH. PID: the pathway interaction database. Nucleic Acids Res 2009; 37(Database issue suppl_1): D674–D679
Stenson PD, Mort M, Ball EV, Evans K, Hayden M, Heywood S, Hussain M, Phillips AD, Cooper DN. The Human Gene Mutation Database: towards a comprehensive repository of inherited mutation data for medical research, genetic diagnosis and next-generation sequencing studies. Hum Genet 2017; 136(6): 665–677
Fabregat A, Jupe S, Matthews L, Sidiropoulos K, Gillespie M, Garapati P, Haw R, Jassal B, Korninger F, May B, Milacic M, Roca CD, Rothfels K, Sevilla C, Shamovsky V, Shorser S, Varusai T, Viteri G, Weiser J, Wu G, Stein L, Hermjakob H, D’Eustachio P. The Reactome Pathway Knowledgebase. Nucleic Acids Res 2018; 46(D1): D649–D655
Kim W, Han TH, Kim HJ, Park MY, Kim KS, Park RW. An automated measurement of ciliary beating frequency using a combined optical flow and peak detection. Healthc Inform Res 2011; 17(2): 111–119
Smith CM, Djakow J, Free RC, Djakow P, Lonnen R, Williams G, Pohunek P, Hirst RA, Easton AJ, Andrew PW, O’Callaghan C. ciliaFA: a research tool for automated, high-throughput measurement of ciliary beat frequency using freely available software. Cilia 2012; 1(1): 14
Sampaio P, da Silva MF, Vale I, Roxo-Rosa M, Pinto A, Constant C, Pereira L, Quintão CM, Lopes SS. CiliarMove: new software for evaluating ciliary beat frequency helps find novel mutations by a Portuguese multidisciplinary team on primary ciliary dyskinesia. ERJ Open Res 2021; 7(1): 00792–2020
Yi WJ, Park KS, Min YG, Sung MW. Distribution mapping of ciliary beat frequencies of respiratory epithelium cells using image processing. Med Biol Eng Comput 1997; 35(6): 595–599
Sisson JH, Stoner JA, Ammons BA, Wyatt TA. All-digital image capture and whole-field analysis of ciliary beat frequency. J Microsc 2003; 211(2): 103–111
Shapiro AJ, Davis SD, Polineni D, Manion M, Rosenfeld M, Dell SD, Chilvers MA, Ferkol TW, Zariwala MA, Sagel SD, Josephson M, Morgan L, Yilmaz O, Olivier KN, Milla C, Pittman JE, Daniels MLA, Jones MH, Janahi IA, Ware SM, Daniel SJ, Cooper ML, Nogee LM, Anton B, Eastvold T, Ehrne L, Guadagno E, Knowles MR, Leigh MW, Lavergne V; American Thoracic Society Assembly on Pediatrics. Diagnosis of primary ciliary dyskinesia. An official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med 2018; 197(12): e24–e39
Teves ME, Nagarkatti-Gude DR, Zhang Z, Strauss JF 3rd. Mammalian axoneme central pair complex proteins: Broader roles revealed by gene knockout phenotypes. Cytoskeleton (Hoboken) 2016; 73(1): 3–22
Collins SA, Gove K, Walker W, Lucas JSA. Nasal nitric oxide screening for primary ciliary dyskinesia: systematic review and meta-analysis. Eur Respir J 2014; 44(6): 1589–1599
Kott E, Legendre M, Copin B, Papon JF, Dastot-Le Moal F, Montantin G, Duquesnoy P, Piterboth W, Amram D, Bassinet L, Beucher J, Beydon N, Deneuville E, Houdouin V, Journel H, Just J, Nathan N, Tamalet A, Collot N, Jeanson L, Le Gouez M, Vallette B, Vojtek AM, Epaud R, Coste A, Clement A, Housset B, Louis B, Escudier E, Amselem S. Loss-of-function mutations in RSPH1 cause primary ciliary dyskinesia with central-complex and radial-spoke defects. Am J Hum Genet 2013; 93(3): 561–570
Knowles MR, Ostrowski LE, Leigh MW, Sears PR, Davis SD, Wolf WE, Hazucha MJ, Carson JL, Olivier KN, Sagel SD, Rosenfeld M, Ferkol TW, Dell SD, Milla CE, Randell SH, Yin W, Sannuti A, Metjian HM, Noone PG, Noone PJ, Olson CA, Patrone MV, Dang H, Lee HS, Hurd TW, Gee HY, Otto EA, Halbritter J, Kohl S, Kircher M, Krischer J, Bamshad MJ, Nickerson DA, Hildebrandt F, Shendure J, Zariwala MA. Mutations in RSPH1 cause primary ciliary dyskinesia with a unique clinical and ciliary phenotype. Am J Respir Crit Care Med 2014; 189(6): 707–717
Ibanez-Tallon I, Gorokhova S, Heintz N. Loss of function of axonemal dynein Mdnah5 causes primary ciliary dyskinesia and hydrocephalus. Hum Mol Genet 2002; 11(6): 715–721
Becker-Heck A, Zohn IE, Okabe N, Pollock A, Lenhart KB, Sullivan-Brown J, McSheene J, Loges NT, Olbrich H, Haeffner K, Fliegauf M, Horvath J, Reinhardt R, Nielsen KG, Marthin JK, Baktai G, Anderson KV, Geisler R, Niswander L, Omran H, Burdine RD. The coiled-coil domain containing protein CCDC40 is essential for motile cilia function and left-right axis formation. Nat Genet 2011; 43(1): 79–84
Zou W, Lv Y, Liu ZI, Xia P, Li H, Jiao J. Loss of Rsph9 causes neonatal hydrocephalus with abnormal development of motile cilia in mice. Sci Rep 2020; 10(1): 12435
Kempeneers C, Seaton C, Garcia Espinosa B, Chilvers MA. Ciliary functional analysis: beating a path towards standardization. Pediatr Pulmonol 2019; 54(10): 1627–1638
Bustamante-Marin XM, Yin WN, Sears PR, Werner ME, Brotslaw EJ, Mitchell BJ, Jania CM, Zeman KL, Rogers TD, Herring LE, Refabért L, Thomas L, Amselem S, Escudier E, Legendre M, Grubb BR, Knowles MR, Zariwala MA, Ostrowski LE. Lack of GAS2L2 causes PCD by impairing cilia orientation and mucociliary clearance. Am J Hum Genet 2019; 104(2): 229–245
Parrilla E, Armengot M, Mata M, Cortijo J, Riera J, Hueso JL, Moratal D. Optical flow method in phase-contrast microscopy images for the diagnosis of primary ciliary dyskinesia through measurement of ciliary beat frequency. Preliminary results. 2012 9th IEEE International Symposium on Biomedical Imaging (ISBI), Barcelona, Spain, 2012, 1655–1658
Petriman NA, Lorentzen E. Structural insights into the architecture and assembly of eukaryotic flagella. Microb Cell 2020; 7(11): 289–299
Ishikawa T. 3D structure of eukaryotic flagella/cilia by cryo-electron tomography. Biophysics (Nagoya-Shi) 2013; 9(0): 141–148
Olbrich H, Cremers C, Loges NT, Werner C, Nielsen KG, Marthin JK, Philipsen M, Wallmeier J, Pennekamp P, Menchen T, Edelbusch C, Dougherty GW, Schwartz O, Thiele H, Altmüller J, Rommelmann F, Omran H. Loss-of-function GAS8 mutations cause primary ciliary dyskinesia and disrupt the nexin-dynein regulatory complex. Am J Hum Genet 2015; 97(4): 546–554
Wirschell M, Olbrich H, Werner C, Tritschler D, Bower R, Sale WS, Loges NT, Pennekamp P, Lindberg S, Stenram U, Carlén B, Horak E, Köhler G, Nürnberg P, Nürnberg G, Porter ME, Omran H. The nexin-dynein regulatory complex subunit DRC1 is essential for motile cilia function in algae and humans. Nat Genet 2013; 45(3): 262–268
Horani A, Brody SL, Ferkol TW, Shoseyov D, Wasserman MG, Ta-shma A, Wilson KS, Bayly PV, Amirav I, Cohen-Cymberknoh M, Dutcher SK, Elpeleg O, Kerem E. CCDC65 mutation causes primary ciliary dyskinesia with normal ultrastructure and hyperkinetic cilia. PLoS One 2013; 8(8): e72299
Lucas JS, Barbato A, Collins SA, Goutaki M, Behan L, Caudri D, Dell S, Eber E, Escudier E, Hirst RA, Hogg C, Jorissen M, Latzin P, Legendre M, Leigh MW, Midulla F, Nielsen KG, Omran H, Papon JF, Pohunek P, Redfern B, Rigau D, Rindlisbacher B, Santamaria F, Shoemark A, Snijders D, Tonia T, Titieni A, Walker WT, Werner C, Bush A, Kuehni CE. European Respiratory Society guidelines for the diagnosis of primary ciliary dyskinesia. Eur Respir J 2017; 49(1): 1601090
Horani A, Ferkol TW, Dutcher SK, Brody SL. Genetics and biology of primary ciliary dyskinesia. Paediatr Respir Rev 2016; 18: 18–24
Han L, Rao Q, Yang R, Wang Y, Chai P, Xiong Y, Zhang K. Cryo-EM structure of an active central apparatus. Nat Struct Mol Biol 2022; 29(5): 472–482
Gui M, Wang X, Dutcher SK, Brown A, Zhang R. Ciliary central apparatus structure reveals mechanisms of microtubule patterning. Nat Struct Mol Biol 2022; 29(5): 483–492
DiPetrillo CG, Smith EF. The Pcdp1 complex coordinates the activity of dynein isoforms to produce wild-type ciliary motility. Mol Biol Cell 2011; 22(23): 4527–4538
Lee L, Campagna DR, Pinkus JL, Mulhern H, Wyatt TA, Sisson JH, Pavlik JA, Pinkus GS, Fleming MD. Primary ciliary dyskinesia in mice lacking the novel ciliary protein Pcdp1. Mol Cell Biol 2008; 28(3): 949–957
Bustamante-Marin XM, Shapiro A, Sears PR, Charng WL, Conrad DF, Leigh MW, Knowles MR, Ostrowski LE, Zariwala MA. Identification of genetic variants in CFAP221 as a cause of primary ciliary dyskinesia. J Hum Genet 2020; 65(2): 175–180
Liu C, Tu C, Wang L, Wu H, Houston BJ, Mastrorosa FK, Zhang W, Shen Y, Wang J, Tian S, Meng L, Cong J, Yang S, Jiang Y, Tang S, Zeng Y, Lv M, Lin G, Li J, Saiyin H, He X, Jin L, Touré A, Ray PF, Veltman JA, Shi Q, O’Bryan MK, Cao Y, Tan YQ, Zhang F. Deleterious variants in X-linked CFAP47 induce asthenoteratozoospermia and primary male infertility. Am J Hum Genet 2021; 108(2): 309–323
Sha Y, Wei X, Ding L, Ji Z, Mei L, Huang X, Su Z, Wang W, Zhang X, Lin S. Biallelic mutations of CFAP74 may cause human primary ciliary dyskinesia and MMAF phenotype. J Hum Genet 2020; 65(11): 961–969
Thomas L, Bouhouche K, Whitfield M, Thouvenin G, Coste A, Louis B, Szymanski C, Bequignon E, Papon JF, Castelli M, Lemullois M, Dhalluin X, Drouin-Garraud V, Montantin G, Tissier S, Duquesnoy P, Copin B, Dastot F, Couvet S, Barbotin AL, Faucon C, Honore I, Maitre B, Beydon N, Tamalet A, Rives N, Koll F, Escudier E, Tassin AM, Touré A, Mitchell V, Amselem S, Legendre M. TTC12 loss-of-function mutations cause primary ciliary dyskinesia and unveil distinct dynein assembly mechanisms in motile cilia versus flagella. Am J Hum Genet 2020; 106(2): 153–169
Sironen A, Kotaja N, Mulhern H, Wyatt TA, Sisson JH, Pavlik JA, Miiluniemi M, Fleming MD, Lee L. Loss of SPEF2 function in mice results in spermatogenesis defects and primary ciliary dyskinesia. Biol Reprod 2011; 85(4): 690–701
Acknowledgements
The authors thank all the patients and other participants in this study. This study was supported by the National Key Research and Development Program of China (No. 2016YFC0901502 to Kai-Feng Xu; No. 2016YFC0905100 to Xue Zhang; No. 2017YFC1001201 to Yaping Liu), the National Natural Science Foundation of China (NSFC) (No. 81788101 to Xue Zhang; No. 31271345 to Yaping Liu), and the CAMS Initiative for Medical Sciences (CIFMS) (Nos. 2021-1-I2M-018 and 2016-I2M-1-002 to Xue Zhang and Yaping Liu; Nos. 2020-I2M-C&T-B-002 and 2018-I2M-1-003 to Xinlun Tian).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest Xinyue Zhao, Haijun Ge, Wenshuai Xu, Chongsheng Cheng, Wangji Zhou, Yan Xu, Junping Fan, Yaping Liu, and Xinlun Tian declare that they have no conflict of interest. Kai-Feng Xu and Xue Zhang are members of the Editorial Board of Frontiers of Medicine, who were excluded from the peer-review process and all editorial decisions related to the acceptance and publication of this article. Peer-review was handled independently by the other editors to minimise bias.
The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards, and it was approved by the Institutional Review Board committee at PUMCH. Informed consent was obtained from all patients for being included in the study. All institutional and national guidelines for the care and use of laboratory animals were followed.
Electronic supplementary material
Supplementary material, approximately 4.66 MB.
Supplementary material, approximately 6.63 MB.
Rights and permissions
About this article
Cite this article
Zhao, X., Ge, H., Xu, W. et al. Lack of CFAP54 causes primary ciliary dyskinesia in a mouse model and human patients. Front. Med. 17, 1236–1249 (2023). https://doi.org/10.1007/s11684-023-0997-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11684-023-0997-7