Abstract
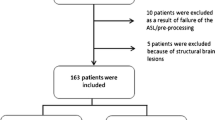
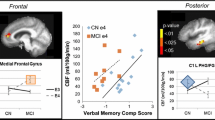
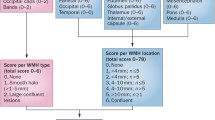
The prevalence of Alzheimer’s disease is projected to reach 13 million in the U.S. by 2050. Although major efforts have been made to avoid this outcome, so far there are no treatments that can stop or reverse the progressive cognitive decline that defines Alzheimer’s disease. The utilization of preventative treatment before significant cognitive decline has occurred may ultimately be the solution, necessitating a reliable biomarker of preclinical/prodromal disease stages to determine which older adults are most at risk. Quantitative cerebral blood flow is a promising potential early biomarker for Alzheimer’s disease, but the spatiotemporal patterns of altered cerebral blood flow in Alzheimer’s disease are not fully understood. The current systematic review compiles the findings of 81 original studies that compared resting gray matter cerebral blood flow in older adults with mild cognitive impairment or Alzheimer’s disease and that of cognitively normal older adults and/or assessed the relationship between cerebral blood flow and objective cognitive function. Individuals with Alzheimer’s disease had relatively decreased cerebral blood flow in all brain regions investigated, especially the temporoparietal and posterior cingulate, while individuals with mild cognitive impairment had consistent results of decreased cerebral blood flow in the posterior cingulate but more mixed results in other regions, especially the frontal lobe. Most papers reported a positive correlation between regional cerebral blood flow and cognitive function. This review highlights the need for more studies assessing cerebral blood flow changes both spatially and temporally over the course of Alzheimer’s disease, as well as the importance of including potential confounding factors in these analyses.


Similar content being viewed by others
Data Availability
We did not analyze or generate datasets because this work involved the compilation and synthesis of previously published results, all of which are cited and available to view.
Abbreviations
- AD:
-
Alzheimer’s disease
- ADAS:
-
Alzheimer’s Disease Assessment Scale
- ASL:
-
Arterial spin labeled
- APOE :
-
Apolipoprotein E
- CAMCOG:
-
Cambridge Cognition Examination
- CANTAB:
-
Cambridge Neuropsychological Test Automated Battery
- CBF:
-
Cerebral blood flow
- CN:
-
Cognitively normal
- DCE:
-
Dynamic contrast enhanced
- DSC:
-
Dynamic susceptibility contrast
- GRADE:
-
Grading of Recommendations Assessment Development and Education
- MCI:
-
Mild cognitive impairment
- MeSH:
-
Medical Subject Headings
- MMSE:
-
Mini-Mental State Examination
- MRI:
-
Magnetic resonance imaging
- PET:
-
Positron emission tomography
- PICO:
-
Population intervention comparison and outcomes
- SCD:
-
Subjective cognitive decline
- SD:
-
Standard deviation
- SPECT:
-
Single-photon emission computerized tomography
References
Alzheimer’s disease facts and Fig. (2021).Alzheimers Dement, 17(3),327–406. https://doi.org/10.1002/alz.12328
Albrecht, D., Isenberg, A. L., Stradford, J., Monreal, T., Sagare, A., Pachicano, M., Sweeney, M., Toga, A., Zlokovic, B., Chui, H., Joe, E., Schneider, L., Conti, P., Jann, K., & Pa, J. (2020). Associations between vascular function and tau PET are Associated with global cognition and amyloid. Journal Of Neuroscience, 40(44), 8573–8586. https://doi.org/10.1523/JNEUROSCI.1230-20.2020.
Alegret, M., Vinyes-Junqué, G., Boada, M., Martínez-Lage, P., Cuberas, G., Espinosa, A., Roca, I., Hernández, I., Valero, S., Rosende-Roca, M., Mauleón, A., Becker, J., & Tárraga, L. (2010). Brain perfusion correlates of visuoperceptual deficits in mild cognitive impairment and mild Alzheimer’s disease. Journal Of Alzheimer’S Disease, 21(2), 557–567. https://doi.org/10.3233/jad-2010-091069.
Alegret, M., Cuberas-Borros, G., Vinyes-Junque, G., Espinosa, A., Valero, S., Hernandez, I., Roca, I., Ruiz, A., Rosende-Roca, M., Mauleon, A., Becker, J. T., Castell-Conesa, J., Tarraga, L., & Boada, M. (2012). A two-year follow-up of cognitive deficits and brain perfusion in mild cognitive impairment and mild Alzheimer’s disease. Journal Of Alzheimer’S Disease, 30(1), 109–120. https://doi.org/10.3233/JAD-2012-111850.
Alfini, A. J., Weiss, L. R., Nielson, K. A., Verber, M. D., & Smith, J. C. (2019). Resting cerebral blood Flow after Exercise training in mild cognitive impairment. Journal Of Alzheimer’S Disease, 67(2), 671–684. https://doi.org/10.3233/JAD-180728.
Ashford, J. W., Shih, W. J., Coupal, J., Shetty, R., Schneider, A., Cool, C., Aleem, A., Kiefer, V. H., Mendiondo, M. S., & Schmitt, F. A. (2000). Single SPECT measures of cerebral cortical perfusion reflect time-index estimation of dementia severity in Alzheimer’s disease. Journal Of Nuclear Medicine, 41(1), 57–64. https://www.ncbi.nlm.nih.gov/pubmed/10647605.
Bangen, K. J., Restom, K., Liu, T. T., Wierenga, C. E., Jak, A. J., Salmon, D. P., & Bondi, M. W. (2012). Assessment of Alzheimer’s disease risk with functional magnetic resonance imaging: an arterial spin labeling study. Journal Of Alzheimer’S Disease, 31(Suppl 3), S59–74. https://doi.org/10.3233/JAD-2012-120292.
Benoit, M., Koulibaly, P. M., Migneco, O., Darcourt, J., Pringuey, D. J., & Robert, P. H. (2002). Brain perfusion in Alzheimer’s disease with and without apathy: a SPECT study with statistical parametric mapping analysis. Psychiatry Research, 114(2), 103–111. https://doi.org/10.1016/s0925-4927(02)00003-3.
Blennow, K., & Zetterberg, H. (2018). The past and the future of Alzheimer’s Disease Fluid biomarkers. Journal Of Alzheimer’S Disease, 62(3), 1125–1140. https://doi.org/10.3233/JAD-170773.
Brayet, P., Petit, D., Baril, A. A., Gosselin, N., Gagnon, J. F., Soucy, J. P., Gauthier, S., Kergoat, M. J., Carrier, J., Rouleau, I., & Montplaisir, J. (2017). Brain perfusion during rapid-eye-movement sleep successfully identifies amnestic mild cognitive impairment. Sleep Medicine, 34, 134–140. https://doi.org/10.1016/j.sleep.2017.01.025.
Brown, D. R., Hunter, R., Wyper, D. J., Patterson, J., Kelly, R. C., Montaldi, D., & McCullouch, J. (1996). Longitudinal changes in cognitive function and regional cerebral function in Alzheimer’s disease: a SPECT blood flow study. Journal Of Psychiatric Research, 30(2), 109–126. https://doi.org/10.1016/0022-3956(95)00032-1.
Brown, D. R., Wyper, D. J., Owens, J., Patterson, J., Kelly, R. C., Hunter, R., & McCulloch, J. (1997). 123Iodo-MK-801: a spect agent for imaging the pattern and extent of glutamate (NMDA) receptor activation in Alzheimer’s disease. Journal Of Psychiatric Research, 31(6), 605–619. https://doi.org/10.1016/s0022-3956(97)00031-9.
Brugnolo, A., Morbelli, S., Dessi, B., Girtler, N., Mazzei, D., Fama, F., Barbieri, P., Cabassi, G., Koulibaly, P. M., Sambuceti, G., Rodriguez, G., & Nobili, F. (2010). The reversed clock drawing test phenomenon in Alzheimer’s disease: a perfusion SPECT study. Dementia And Geriatric Cognitive Disorders, 29(1), 1–10. https://doi.org/10.1159/000270898.
Camargo, A., Wang, Z., & Neuroimaging, A. D., I (2021). Longitudinal cerebral blood Flow Changes in normal aging and the Alzheimer’s Disease Continuum identified by arterial spin labeling MRI. Journal Of Alzheimer’S Disease, 81(4), 1727–1735. https://doi.org/10.3233/JAD-210116.
Chaudhary, S., Scouten, A., Schwindt, G., Janik, R., Lee, W., Sled, J. G., Black, S. E., & Stefanovic, B. (2013). Hemodynamic effects of cholinesterase inhibition in mild Alzheimer’s disease. Journal Of Magnetic Resonance Imaging, 38(1), 26–35. https://doi.org/10.1002/jmri.23967.
Claus, J. J., van Harskamp, F., Breteler, M. M., Krenning, E. P., van der Cammen, T. J., Hofman, A., & Hasan, D. (1994). Assessment of cerebral perfusion with single-photon emission tomography in normal subjects and in patients with Alzheimer’s disease: effects of region of interest selection. European Journal Of Nuclear Medicine, 21(10), 1044–1051. https://doi.org/10.1007/bf00181058.
Colloby, S. J., Fenwick, J. D., Williams, E. D., Paling, S. M., Lobotesis, K., Ballard, C., McKeith, I., & O’Brien, J. T. (2002). A comparison of (99m)Tc-HMPAO SPET changes in dementia with Lewy bodies and Alzheimer’s disease using statistical parametric mapping. European Journal Of Nuclear Medicine And Molecular Imaging, 29(5), 615–622. https://doi.org/10.1007/s00259-002-0778-5.
Colloby, S. J., Field, R. H., Wyper, D. J., O’Brien, J. T., & Taylor, J. P. (2016). A spatial covariance (123)I-5IA-85380 SPECT study of alpha4beta2 nicotinic receptors in Alzheimer’s disease. Neurobiology Of Aging, 47, 83–90. https://doi.org/10.1016/j.neurobiolaging.2016.07.017.
Counts, S. E., Ikonomovic, M. D., Mercado, N., Vega, I. E., & Mufson, E. J. (2017). Biomarkers for the early detection and progression of Alzheimer’s Disease. Neurotherapeutics, 14(1), 35–53. https://doi.org/10.1007/s13311-016-0481-z.
Culpepper, L., Lam, R. W., & McIntyre, R. S. (2017). Cognitive impairment in patients with Depression: awareness, Assessment, and management. Journal Of Clinical Psychiatry, 78(9), 1383–1394. https://doi.org/10.4088/JCP.tk16043ah5c.
Dai, W., Lopez, O. L., Carmichael, O. T., Becker, J. T., Kuller, L. H., & Gach, H. M. (2009). Mild cognitive impairment and alzheimer disease: patterns of altered cerebral blood flow at MR imaging. Radiology, 250(3), 856–866. https://doi.org/10.1148/radiol.2503080751.
DeKosky, S. T., Shih, W. J., Schmitt, F. A., Coupal, J., & Kirkpatrick, C. (1990). Assessing utility of single photon emission computed tomography (SPECT) scan in Alzheimer disease: correlation with cognitive severity. Alzheimer Disease And Associated Disorders, 4(1), 14–23. https://doi.org/10.1097/00002093-199040100-00002.
Deo, A. K., Borson, S., Link, J. M., Domino, K., Eary, J. F., Ke, B., Richards, T. L., Mankoff, D. A., Minoshima, S., O’Sullivan, F., Eyal, S., Hsiao, P., Maravilla, K., & Unadkat, J. D. (2014). Activity of P-Glycoprotein, a beta-amyloid transporter at the blood-brain barrier, is compromised in patients with mild Alzheimer Disease. Journal Of Nuclear Medicine, 55(7), 1106–1111. https://doi.org/10.2967/jnumed.113.130161.
Detre, J. A., Rao, H., Wang, D. J., Chen, Y. F., & Wang, Z. (2012). Applications of arterial spin labeled MRI in the brain. Journal Of Magnetic Resonance Imaging, 35(5), 1026–1037. https://doi.org/10.1002/jmri.23581.
Ding, B., Ling, H. W., Zhang, Y., Huang, J., Zhang, H., Wang, T., & Yan, F. H. (2014). Pattern of cerebral hyperperfusion in Alzheimer’s disease and amnestic mild cognitive impairment using voxel-based analysis of 3D arterial spin-labeling imaging: initial experience. Clinical Interventions In Aging, 9, 493–500. https://doi.org/10.2147/cia.S58879.
Duan, W., Sehrawat, P., Balachandrasekaran, A., Bhumkar, A. B., Boraste, P. B., Becker, J. T., Kuller, L. H., Lopez, O. L., Gach, H. M., & Dai, W. (2020). Cerebral blood Flow is Associated with Diagnostic Class and Cognitive decline in Alzheimer’s Disease. Journal Of Alzheimer’S Disease, 76(3), 1103–1120. https://doi.org/10.3233/JAD-200034.
Duan, W., Zhou, G. D., Balachandrasekaran, A., Bhumkar, A. B., Boraste, P. B., Becker, J. T., Kuller, L. H., Lopez, O. L., Gach, H. M., & Dai, W. (2021). Cerebral blood Flow predicts Conversion of mild cognitive impairment into Alzheimer’s Disease and Cognitive decline: an arterial spin labeling follow-up study. Journal Of Alzheimer’S Disease, 82(1), 293–305. https://doi.org/10.3233/JAD-210199.
Duran, F. L., Zampieri, F. G., Bottino, C. C., Buchpiguel, C. A., & Busatto, G. F. (2007). Voxel-based investigations of regional cerebral blood flow abnormalities in Alzheimer’s disease using a single-detector SPECT system. Clinics (Sao Paulo), 62(4), 377–384. https://doi.org/10.1590/s1807-59322007000400002.
Edelman, R. R., Mattle, H. P., Atkinson, D. J., Hill, T., Finn, J. P., Mayman, C., Ronthal, M., Hoogewoud, H. M., & Kleefield, J. (1990). Cerebral blood flow: assessment with dynamic contrast-enhanced T2*-weighted MR imaging at 1.5 T. Radiology, 176(1), 211–220. https://doi.org/10.1148/radiology.176.1.2353094.
Encinas, M., De Juan, R., Marcos, A., Gil, P., Barabash, A., Fernández, C., De Ugarte, C., & Cabranes, J. A. (2003). Regional cerebral blood flow assessed with 99mTc-ECD SPET as a marker of progression of mild cognitive impairment to Alzheimer’s disease. European Journal Of Nuclear Medicine And Molecular Imaging, 30(11), 1473–1480. https://doi.org/10.1007/s00259-003-1277-z.
Firbank, M. J., Colloby, S. J., Burn, D. J., McKeith, I. G., & O’Brien, J. T. (2003). Regional cerebral blood flow in Parkinson’s disease with and without dementia. Neuroimage, 20(2), 1309–1319. https://doi.org/10.1016/S1053-8119(03)00364-1.
Firbank, M. J., He, J., Blamire, A. M., Singh, B., Danson, P., Kalaria, R. N., & O’Brien, J. T. (2011). Cerebral blood flow by arterial spin labeling in poststroke dementia. Neurology, 76(17), 1478–1484. https://doi.org/10.1212/WNL.0b013e318217e76a.
German, F., Andres, D., Leandro, U., Nicolas, N., Graciela, L., Yanina, B., Patricio, C., Adriana, Q., Cecilia, B., Ismael, C., Ismael, C., de Leon, M. P., Valeria, C., Feuerstein, V., Sergio, D., Ricardo, A., Henry, E., & Silvia, V. (2021). Connectivity and patterns of Regional Cerebral Blood Flow, cerebral glucose uptake, and abeta-amyloid deposition in Alzheimer’s Disease (early and Late-Onset) compared to normal ageing. Current Alzheimer Research, 18(8), 646–655. https://doi.org/10.2174/1567205018666211116095035.
Habert, M. O., Horn, J. F., Sarazin, M., Lotterie, J. A., Puel, M., Onen, F., Zanca, M., Portet, F., Touchon, J., Verny, M., Mahieux, F., Giron, A., Fertil, B., & Dubois, B. (2011). Brain perfusion SPECT with an automated quantitative tool can identify prodromal Alzheimer’s disease among patients with mild cognitive impairment. Neurobiology Of Aging, 32(1), 15–23. https://doi.org/10.1016/j.neurobiolaging.2009.01.013.
Haji, M., Kimura, N., Hanaoka, T., Aso, Y., Takemaru, M., Hirano, T., & Matsubara, E. (2015). Evaluation of regional cerebral blood flow in Alzheimer’s disease patients with subclinical hypothyroidism. Dementia And Geriatric Cognitive Disorders, 39(5–6), 360–367. https://doi.org/10.1159/000375298.
Hanyu, H., Shimuzu, T., Tanaka, Y., Takasaki, M., Koizumi, K., & Abe, K. (2003). Effect of age on regional cerebral blood flow patterns in Alzheimer’s disease patients. Journal Of The Neurological Sciences, 209(1–2), 25–30. https://doi.org/10.1016/s0022-510x(02)00456-2.
Hanyu, H., Shimizu, T., Tanaka, Y., Takasaki, M., Koizumi, K., & Abe, K. (2003). Regional cerebral blood flow patterns and response to donepezil treatment in patients with Alzheimer’s disease. Dementia And Geriatric Cognitive Disorders, 15(4), 177–182. https://doi.org/10.1159/000068785.
Hanyu, H., Shimizu, S., Tanaka, Y., Takasaki, M., Koizumi, K., & Abe, K. (2004). Differences in regional cerebral blood flow patterns in male versus female patients with Alzheimer disease. Ajnr. American Journal Of Neuroradiology, 25(7), 1199–1204.
Hanyu, H., Sakurai, H., Hirao, K., Sato, T., & Iwamoto, T. (2008). Difference in practice effects depending on cerebral perfusion pattern in mild cognitive impairment. International Journal Of Geriatric Psychiatry, 23(1), 111–112. https://doi.org/10.1002/gps.1834.
Hanyu, H., Sato, T., Shimizu, S., Kanetaka, H., Iwamoto, T., & Koizumi, K. (2008). The effect of education on rCBF changes in Alzheimer’s disease: a longitudinal SPECT study. European Journal Of Nuclear Medicine And Molecular Imaging, 35(12), 2182–2190. https://doi.org/10.1007/s00259-008-0848-4.
Hanyu, H., Sato, T., Hirao, K., Kanetaka, H., Iwamoto, T., & Koizumi, K. (2010). The progression of cognitive deterioration and regional cerebral blood flow patterns in Alzheimer’s disease: a longitudinal SPECT study. Journal Of The Neurological Sciences, 290(1–2), 96–101. https://doi.org/10.1016/j.jns.2009.10.022.
Hardy, J. A., & Higgins, G. A. (1992). Alzheimer’s disease: the amyloid cascade hypothesis. Science, 256(5054), 184–185. https://doi.org/10.1126/science.1566067.
Harris, G. J., Links, J. M., Pearlson, G. D., & Camargo, E. E. (1991). Cortical circumferential profile of SPECT cerebral perfusion in Alzheimer’s disease. Psychiatry Research, 40(3), 167–180. https://doi.org/10.1016/0925-4927(91)90008-e.
Harris, G. J., Lewis, R. F., Satlin, A., English, C. D., Scott, T. M., Yurgelun-Todd, D. A., & Renshaw, P. F. (1998). Dynamic susceptibility contrast MR imaging of regional cerebral blood volume in Alzheimer disease: a promising alternative to nuclear medicine. Ajnr. American Journal Of Neuroradiology, 19(9), 1727–1732. https://www.ncbi.nlm.nih.gov/pubmed/9802497.
Hayashi, A., Nomura, H., Mochizuki, R., Ohnuma, A., Kimpara, T., Ootomo, K., Hosokai, Y., Ishioka, T., Suzuki, K., & Mori, E. (2011). Neural substrates for writing impairments in japanese patients with mild Alzheimer’s disease: a SPECT study. Neuropsychologia, 49(7), 1962–1968. https://doi.org/10.1016/j.neuropsychologia.2011.03.024.
Hayashi, H., Kobayashi, R., Kawakatsu, S., Ohba, M., Morioka, D., & Otani, K. (2021). Comparison of the decreases in regional cerebral blood flow in the posterior cingulate cortex, precuneus, and parietal lobe between suspected non-alzheimer’s disease pathophysiology and Alzheimer’s disease. Psychogeriatrics, 21(5), 716–721. https://doi.org/10.1111/psyg.12729.
Houston, A. S., Kemp, P. M., Macleod, M. A., Francis, J. R., Colohan, H. A., & Matthews, H. P. (1998). Use of significance image to determine patterns of cortical blood flow abnormality in pathological and at-risk groups. Journal Of Nuclear Medicine, 39(3), 425–430. https://www.ncbi.nlm.nih.gov/pubmed/9529286.
Hoyer, S. (1991). Abnormalities of glucose metabolism in Alzheimer’s disease. Annals Of The New York Academy Of Sciences, 640, 53–58. https://doi.org/10.1111/j.1749-6632.1991.tb00190.x.
Hoyer, S., Nitsch, R., & Oesterreich, K. (1991). Predominant abnormality in cerebral glucose utilization in late-onset dementia of the Alzheimer type: a cross-sectional comparison against advanced late-onset and incipient early-onset cases. J Neural Transm Park Dis Dement Sect, 3(1), 1–14. https://doi.org/10.1007/BF02251132.
Hoyer, S. (1993). Intermediary metabolism disturbance in AD/SDAT and its relation to molecular events. Progress In Neuropsychopharmacology And Biological Psychiatry, 17(2), 199–228. https://doi.org/10.1016/0278-5846(93)90043-r.
Iadecola, C., & Gottesman, R. F. (2019). Neurovascular and cognitive dysfunction in hypertension. Circ Res, 124(7), 1025–1044. https://doi.org/10.1161/CIRCRESAHA.118.313260.
Iizuka, T., & Kameyama, M. (2017). Cholinergic enhancement increases regional cerebral blood flow to the posterior cingulate cortex in mild Alzheimer’s disease. Geriatrics & Gerontology International, 17(6), 951–958. https://doi.org/10.1111/ggi.12818.
Imran, M. B., Kawashima, R., Awata, S., Sato, K., Kinomura, S., Ito, H., Ono, S., Yoshioka, S., Sato, M., & Fukuda, H. (1998). Use of automated image registration to generate mean brain SPECT image of Alzheimer’s patients. Annals Of Nuclear Medicine, 12(3), 127–132. https://doi.org/10.1007/BF03164776.
Ishii, K., Sasaki, M., Sakamoto, S., Yamaji, S., Kitagaki, H., & Mori, E. (1999). Tc-99m ethyl cysteinate dimer SPECT and 2-[F-18]fluoro-2-deoxy-D-glucose PET in Alzheimer’s disease. Comparison of perfusion and metabolic patterns. Clinical Nuclear Medicine, 24(8), 572–575. https://doi.org/10.1097/00003072-199908000-00005.
Ishiwata, A., Sakayori, O., Minoshima, S., Mizumura, S., Kitamura, S., & Katayama, Y. (2006). Preclinical evidence of Alzheimer changes in progressive mild cognitive impairment: a qualitative and quantitative SPECT study. Acta Neurologica Scandinavica, 114(2), 91–96. https://doi.org/10.1111/j.1600-0404.2006.00661.x.
Ito, K., Mori, E., Fukuyama, H., Ishii, K., Washimi, Y., Asada, T., Mori, S., Meguro, K., Kitamura, S., Hanyu, H., Nakano, S., Matsuda, H., Kuwabara, Y., Hashikawa, K., Momose, T., Uchida, Y., Hatazawa, J., Minoshima, S., Kosaka, K., Yamada, T., Yonekura, Y., & Group, J. C. S. (2013). Prediction of outcomes in MCI with (123)I-IMP-CBF SPECT: a multicenter prospective cohort study. Annals Of Nuclear Medicine, 27(10), 898–906. https://doi.org/10.1007/s12149-013-0768-7.
Jagust, W. J., Budinger, T. F., & Reed, B. R. (1987). The diagnosis of dementia with single photon emission computed tomography. Archives Of Neurology, 44(3), 258–262. https://doi.org/10.1001/archneur.1987.00520150014011.
Jessen, F., Amariglio, R. E., van Boxtel, M., Breteler, M., Ceccaldi, M., Chetelat, G., Dubois, B., Dufouil, C., Ellis, K. A., van der Flier, W. M., Glodzik, L., van Harten, A. C., de Leon, M. J., McHugh, P., Mielke, M. M., Molinuevo, J. L., Mosconi, L., Osorio, R. S., Perrotin, A., Petersen, R. C., Rabin, L. A., Rami, L., Reisberg, B., Rentz, D. M., Sachdev, P. S., de la Sayette, V., Saykin, A. J., Scheltens, P., Shulman, M. B., Slavin, M. J., Sperling, R. A., Stewart, R., Uspenskaya, O., Vellas, B., Visser, P. J., & Wagner, M. (2014). A conceptual framework for research on subjective cognitive decline in preclinical Alzheimer’s disease. Alzheimers Dement, 10(6), 844–852. https://doi.org/10.1016/j.jalz.2014.01.001. Subjective Cognitive Decline Initiative Working, G.
Jessen, F., Amariglio, R. E., Buckley, R. F., van der Flier, W. M., Han, Y., Molinuevo, J. L., Rabin, L., Rentz, D. M., Rodriguez-Gomez, O., Saykin, A. J., Sikkes, S. A. M., Smart, C. M., Wolfsgruber, S., & Wagner, M. (2020). The characterisation of subjective cognitive decline. Lancet Neurology, 19(3), 271–278. https://doi.org/10.1016/S1474-4422(19)30368-0.
Johnson, K. A., Holman, B. L., Mueller, S. P., Rosen, T. J., English, R., Nagel, J. S., & Growdon, J. H. (1988). Single photon emission computed tomography in Alzheimer’s disease. Abnormal iofetamine I 123 uptake reflects dementia severity. Archives Of Neurology, 45(4), 392–396. https://doi.org/10.1001/archneur.1988.00520280038013.
Johnson, K. A., Moran, E. K., Becker, J. A., Blacker, D., Fischman, A. J., & Albert, M. S. (2007). Single photon emission computed tomography perfusion differences in mild cognitive impairment. Journal Of Neurology, Neurosurgery And Psychiatry, 78(3), 240–247. https://doi.org/10.1136/jnnp.2006.096800.
Jones, T., Chesler, D. A., & Ter-Pogossian, M. M. (1976). The continuous inhalation of oxygen-15 for assessing regional oxygen extraction in the brain of man. British Journal Of Radiology, 49(580), 339–343. https://doi.org/10.1259/0007-1285-49-580-339.
Kaneta, T., Katsuse, O., Hirano, T., Ogawa, M., Shihikura-Hino, A., Yoshida, K., Odawara, T., Hirayasu, Y., & Inoue, T. (2017). Voxel-wise correlations between cognition and cerebral blood flow using arterial spin-labeled perfusion MRI in patients with Alzheimer’s disease: a cross-sectional study. Bmc Neurology, 17(1), 91. https://doi.org/10.1186/s12883-017-0870-x.
Kawamura, J., Meyer, J. S., Terayama, Y., & Weathers, S. (1991). Cerebral white matter perfusion in dementia of Alzheimer type. Alzheimer Disease And Associated Disorders, 5(4), 231–239. https://doi.org/10.1097/00002093-199100540-00002.
Keller, C., Kadir, A., Forsberg, A., Porras, O., & Nordberg, A. (2011). Long-term effects of galantamine treatment on brain functional activities as measured by PET in Alzheimer’s disease patients. Journal Of Alzheimer’S Disease, 24(1), 109–123. https://doi.org/10.3233/JAD-2010-101290.
Kety, S. S., & Schmidt, C. F. (1948). The Nitrous Oxide Method for the quantitative determination of cerebral blood Flow in Man: Theory, Procedure and normal values. J Clin Invest, 27(4), 476–483. https://doi.org/10.1172/JCI101994.
Kimura, N., Kumamoto, T., Masuda, H., Hanaoka, T., Hazama, Y., Okazaki, T., & Arakawa, R. (2011). Relationship between thyroid hormone levels and regional cerebral blood flow in Alzheimer disease. Alzheimer Disease And Associated Disorders, 25(2), 138–143. https://doi.org/10.1097/WAD.0b013e3181f9aff2.
Kimura, N., Kumamoto, T., Masuda, T., Hanaoka, T., Okazaki, T., & Arakawa, R. (2012). Evaluation of the regional cerebral blood flow changes during long-term donepezil therapy in patients with Alzheimer’s disease using 3DSRT. Journal Of Neuroimaging, 22(3), 299–304. https://doi.org/10.1111/j.1552-6569.2011.00612.x.
Knapp, W. H., Dannenberg, C., Marschall, B., Zedlick, D., Loschmann, K., Bettin, S., Barthel, H., & Seese, A. (1996). Changes in local cerebral blood flow by neuroactivation and vasoactivation in patients with impaired cognitive function. European Journal Of Nuclear Medicine, 23(8), 878–888. https://doi.org/10.1007/BF01084360.
Komatani, A., Yamaguchi, K., Sugai, Y., Takanashi, T., Kera, M., Shinohara, M., & Kawakatsu, S. (1988). Assessment of demented patients by dynamic SPECT of inhaled xenon-133. Journal Of Nuclear Medicine, 29(10), 1621–1626. https://www.ncbi.nlm.nih.gov/pubmed/3262723.
Lacalle-Aurioles, M., Alemán-Gómez, Y., Guzmán-De-Villoria, J. A., Cruz-Orduña, I., Olazarán, J., Mateos-Pérez, J. M., Martino, M. E., & Desco, M. (2013). Is the cerebellum the optimal reference region for intensity normalization of perfusion MR studies in early Alzheimer’s disease? PLoS One, 8(12), e81548. https://doi.org/10.1371/journal.pone.0081548.
Lacalle-Aurioles, M., Mateos-Perez, J. M., Guzman-De-Villoria, J. A., Olazaran, J., Cruz-Orduna, I., Aleman-Gomez, Y., Martino, M. E., & Desco, M. (2014). Cerebral blood flow is an earlier indicator of perfusion abnormalities than cerebral blood volume in Alzheimer’s disease. Journal Of Cerebral Blood Flow And Metabolism, 34(4), 654–659. https://doi.org/10.1038/jcbfm.2013.241.
Lajoie, I., Nugent, S., Debacker, C., Dyson, K., Tancredi, F. B., Badhwar, A., Belleville, S., Deschaintre, Y., Bellec, P., Doyon, J., Bocti, C., Gauthier, S., Arnold, D., Kergoat, M. J., Chertkow, H., Monchi, O., & Hoge, R. D. (2017). Application of calibrated fMRI in Alzheimer’s disease. Neuroimage Clin, 15, 348–358. https://doi.org/10.1016/j.nicl.2017.05.009.
Lassen, N. A., & Ingvar, D. H. (1961). The blood flow of the cerebral cortex determined by radioactive krypton. Experientia, 17, 42–43. https://doi.org/10.1007/BF02157946.
Lassen, N. A., Hoedt-Rasmussen, K., Sorensen, S. C., Skinhoj, E., Cronquist, S., Bodforss, B., & Ingvar, D. H. (1963). Regional Cerebral Blood Flow in Man determined by Krypton. Neurology, 13, 719–727. https://doi.org/10.1212/wnl.13.9.719.
Lee, Y. C., Liu, R. S., Liao, Y. C., Sun, C. M., Wang, P. S., Wang, P. N., & Liu, H. C. (2003). Statistical parametric mapping of brain SPECT perfusion abnormalities in patients with Alzheimer’s disease. European Neurology, 49(3), 142–145. https://doi.org/10.1159/000069086.
Liu, Y., Zeng, X., Wang, Z., Zhang, N., Fan, D., & Yuan, H. (2015). Different post label delay cerebral blood flow measurements in patients with Alzheimer’s disease using 3D arterial spin labeling. Magnetic Resonance Imaging, 33(9), 1019–1025. https://doi.org/10.1016/j.mri.2015.05.001.
Lobotesis, K., Fenwick, J. D., Phipps, A., Ryman, A., Swann, A., Ballard, C., McKeith, I. G., & O’Brien, J. T. (2001). Occipital hypoperfusion on SPECT in dementia with Lewy bodies but not AD. Neurology, 56(5), 643–649. https://doi.org/10.1212/wnl.56.5.643.
Lovblad, K. O., Montandon, M. L., Viallon, M., Rodriguez, C., Toma, S., Golay, X., Giannakopoulos, P., & Haller, S. (2015). Arterial spin-labeling parameters influence Signal Variability and estimated Regional relative cerebral blood Flow in normal aging and mild cognitive impairment: FAIR versus PICORE techniques. Ajnr. American Journal Of Neuroradiology, 36(7), 1231–1236. https://doi.org/10.3174/ajnr.A4291.
Maeda, M., Itoh, S., Kimura, H., Iwasaki, T., Hayashi, N., Yamamoto, K., Ishii, Y., & Kubota, T. (1993). Tumor vascularity in the brain: evaluation with dynamic susceptibility-contrast MR imaging. Radiology, 189(1), 233–238. https://doi.org/10.1148/radiology.189.1.8372199.
Matsuda, H. (2001). Cerebral blood flow and metabolic abnormalities in Alzheimer’s disease. Annals Of Nuclear Medicine, 15(2), 85–92. https://doi.org/10.1007/BF02988596.
Mattsson, N., Tosun, D., Insel, P. S., Simonson, A., Jack, C. R. Jr., Beckett, L. A., Donohue, M., Jagust, W., Schuff, N., & Weiner, M. W. (2014). & Alzheimer’s Disease Neuroimaging, I. Association of brain amyloid-beta with cerebral perfusion and structure in Alzheimer’s disease and mild cognitive impairment. Brain, 137(Pt 5), 1550–1561. https://doi.org/10.1093/brain/awu043
Mielke, R., Pietrzyk, U., Jacobs, A., Fink, G. R., Ichimiya, A., Kessler, J., Herholz, K., & Heiss, W. D. (1994). HMPAO SPET and FDG PET in Alzheimer’s disease and vascular dementia: comparison of perfusion and metabolic pattern. European Journal Of Nuclear Medicine, 21(10), 1052–1060. https://doi.org/10.1007/BF00181059.
Mitsumoto, T., Ohya, N., Ichimiya, A., Sakaguchi, Y., Kiyota, A., Abe, K., Morishita, J., & Sasaki, M. (2009). Diagnostic performance of Tc-99m HMPAO SPECT for early and late onset Alzheimer’s disease: a clinical evaluation of linearization correction. Annals Of Nuclear Medicine, 23(5), 487–495. https://doi.org/10.1007/s12149-009-0266-0.
Mortel, K. F., Pavol, M. A., Wood, S., Meyer, J. S., Terayama, Y., Rexer, J. L., & Herod, B. (1994). Prospective studies of cerebral perfusion and cognitive testing among elderly normal volunteers and patients with ischemic vascular dementia and Alzheimer’s disease. Angiology, 45(3), 171–180. https://doi.org/10.1177/000331979404500301.
Mubrin, Z., Knezevic, S., Spilich, G., Risberg, J., Gubarev, N., Wannenmacher, W., & Vucinic, G. (1989). Normalization of rCBF pattern in senile dementia of the Alzheimer’s type. Psychiatry Research, 29(3), 303–306. https://doi.org/10.1016/0165-1781(89)90072-3.
Murray, M. E., Graff-Radford, N. R., Ross, O. A., Petersen, R. C., Duara, R., & Dickson, D. W. (2011). Neuropathologically defined subtypes of Alzheimer’s disease with distinct clinical characteristics: a retrospective study. Lancet Neurology, 10(9), 785–796. https://doi.org/10.1016/S1474-4422(11)70156-9.
Nagahama, Y., Nabatame, H., Okina, T., Yamauchi, H., Narita, M., Fujimoto, N., Murakami, M., Fukuyama, H., & Matsuda, M. (2003). Cerebral correlates of the progression rate of the cognitive decline in probable Alzheimer’s disease. European Neurology, 50(1), 1–9. https://doi.org/10.1159/000070851.
Nobili, F., Brugnolo, A., Calvini, P., Copello, F., De Leo, C., Girtler, N., Morbelli, S., Piccardo, A., Vitali, P., & Rodriguez, G. (2005). Resting SPECT-neuropsychology correlation in very mild Alzheimer’s disease. Clinical Neurophysiology, 116(2), 364–375. https://doi.org/10.1016/j.clinph.2004.09.001.
Obara, K., Meyer, J. S., Mortel, K. F., & Muramatsu, K. (1994). Cognitive declines correlate with decreased cortical volume and perfusion in dementia of Alzheimer type. Journal Of The Neurological Sciences, 127(1), 96–102. https://doi.org/10.1016/0022-510x(94)90141-4.
O’Mahony, D., Coffey, J., Murphy, J., O’Hare, N., Hamilton, D., Rowan, M., Freyne, P., Walsh, J. B., & Coakley, D. (1996). Event-related potential prolongation in Alzheimer’s disease signifies frontal lobe impairment: evidence from SPECT imaging. Journals Of Gerontology. Series A, Biological Sciences And Medical Sciences, 51(3), M102–107. https://doi.org/10.1093/gerona/51a.3.m102.
Ottoy, J., Verhaeghe, J., Niemantsverdriet, E., De Roeck, E., Wyffels, L., Ceyssens, S., Van Broeckhoven, C., Engelborghs, S., Stroobants, S., & Staelens, S. (2019). 18)F-FDG PET, the early phases and the delivery rate of (18)F-AV45 PET as proxies of cerebral blood flow in Alzheimer’s disease: validation against (15)O-H2O PET. Alzheimers Dement, 15(9), 1172–1182. https://doi.org/10.1016/j.jalz.2019.05.010.
Pappata, S., Varrone, A., Vicidomini, C., Milan, G., De Falco, C., Sansone, V., Iavarone, A., Comerci, M., Lore, E., Panico, M. R., Quarantelli, M., Postiglione, A., & Salvatore, M. (2010). SPECT imaging of GABA(A)/benzodiazepine receptors and cerebral perfusion in mild cognitive impairment. European Journal Of Nuclear Medicine And Molecular Imaging, 37(6), 1156–1163. https://doi.org/10.1007/s00259-010-1409-1.
Pearlson, G. D., Harris, G. J., Powers, R. E., Barta, P. E., Camargo, E. E., Chase, G. A., Noga, J. T., & Tune, L. E. (1992). Quantitative changes in mesial temporal volume, regional cerebral blood flow, and cognition in Alzheimer’s disease. Archives Of General Psychiatry, 49(5), 402–408. https://doi.org/10.1001/archpsyc.1992.01820050066012.
Petersen, R. C., Smith, G. E., Waring, S. C., Ivnik, R. J., Tangalos, E. G., & Kokmen, E. (1999). Mild cognitive impairment: clinical characterization and outcome. Archives Of Neurology, 56(3), 303–308. https://doi.org/10.1001/archneur.56.3.303.
Petersen, R. C. (2016). Mild cognitive impairment. Continuum (Minneap Minn), 22(2 Dementia), 404–418. https://doi.org/10.1212/CON.0000000000000313.
Prohovnik, I., Smith, G., Sackeim, H. A., Mayeux, R., & Stern, Y. (1989). Gray-matter degeneration in presenile Alzheimer’s disease. Annals Of Neurology, 25(2), 117–124. https://doi.org/10.1002/ana.410250203.
Quattrini, G., Marizzoni, M., Pizzini, F. B., Galazzo, I. B., Aiello, M., Didic, M., Soricelli, A., Albani, D., Romano, M., Blin, O., Forloni, G., Golay, X., Jovicich, J., Nathan, P. J., Richardson, J. C., Salvatore, M., Frisoni, G. B., Pievani, M., & PharmaCog, C. (2021). Convergent and discriminant validity of default Mode Network and Limbic Network Perfusion in Amnestic mild cognitive impairment patients. Journal Of Alzheimer’S Disease, 82(4), 1797–1808. https://doi.org/10.3233/JAD-210531.
Rane, S., Koh, N., Boord, P., Madhyastha, T., Askren, M. K., Jayadev, S., Cholerton, B., Larson, E., & Grabowski, T. J. (2018). Quantitative cerebrovascular pathology in a community-based cohort of older adults. Neurobiology Of Aging, 65, 77–85. https://doi.org/10.1016/j.neurobiolaging.2018.01.006.
Rempp, K. A., Brix, G., Wenz, F., Becker, C. R., Guckel, F., & Lorenz, W. J. (1994). Quantification of regional cerebral blood flow and volume with dynamic susceptibility contrast-enhanced MR imaging. Radiology, 193(3), 637–641. https://doi.org/10.1148/radiology.193.3.7972800.
Richardson, W. S., Wilson, M. C., Nishikawa, J., & Hayward, R. S. (1995). The well-built clinical question: a key to evidence-based decisions. Acp Journal Club, 123(3), A12–13. https://www.ncbi.nlm.nih.gov/pubmed/7582737.
Rubinski, A., Tosun, D., Franzmeier, N., Neitzel, J., Frontzkowski, L., Weiner, M., & Ewers, M. (2021). Lower cerebral perfusion is associated with tau-PET in the entorhinal cortex across the Alzheimer’s continuum. Neurobiology Of Aging, 102, 111–118. https://doi.org/10.1016/j.neurobiolaging.2021.02.003.
Sakai, M., Hanyu, H., Kume, K., Sato, T., Hirao, K., Kanetaka, H., Abe, S., Kanaya, K., Sakurai, H., & Iwamoto, T. (2013). Rate of progression of Alzheimer’s disease in younger versus older patients: a longitudinal single photon emission computed tomography study. Geriatrics & Gerontology International, 13(3), 555–562. https://doi.org/10.1111/j.1447-0594.2012.00934.x.
Sakurai, H., Hanyu, H., Sato, T., Kume, K., Hirao, K., Kanetaka, H., & Iwamoto, T. (2013). Effects of cilostazol on cognition and regional cerebral blood flow in patients with Alzheimer’s disease and cerebrovascular disease: a pilot study. Geriatrics & Gerontology International, 13(1), 90–97. https://doi.org/10.1111/j.1447-0594.2012.00866.x.
Sase, S., Yamamoto, H., Kawashima, E., Tan, X., & Sawa, Y. (2017). Discrimination between patients with Alzheimer Disease and healthy subjects using Layer Analysis of Cerebral Blood Flow and Xenon Solubility Coefficient in Xenon-Enhanced computed Tomography. Journal Of Computer Assisted Tomography, 41(3), 477–483. https://doi.org/10.1097/rct.0000000000000525.
Sase, S., Yamamoto, H., Kawashima, E., Tan, X., & Sawa, Y. (2018). Discrimination between patients with mild Alzheimer’s disease and healthy subjects based on cerebral blood flow images of the lateral views in xenon-enhanced computed tomography. Psychogeriatrics, 18(1), 3–12. https://doi.org/10.1111/psyg.12281.
Schuff, N., Matsumoto, S., Kmiecik, J., Studholme, C., Du, A., Ezekiel, F., Miller, B. L., Kramer, J. H., Jagust, W. J., Chui, H. C., & Weiner, M. W. (2009). Cerebral blood flow in ischemic vascular dementia and Alzheimer’s disease, measured by arterial spin-labeling magnetic resonance imaging. Alzheimers Dement, 5(6), 454–462. https://doi.org/10.1016/j.jalz.2009.04.1233.
Shimizu, S., Hanyu, H., Kanetaka, H., Iwamoto, T., Koizumi, K., & Abe, K. (2005). Differentiation of dementia with Lewy bodies from Alzheimer’s disease using brain SPECT. Dementia And Geriatric Cognitive Disorders, 20(1), 25–30. https://doi.org/10.1159/000085070.
Song, I. U., Chung, Y. A., Chung, S. W., & Jeong, J. (2014). Early diagnosis of Alzheimer’s disease and Parkinson’s disease associated with dementia using cerebral perfusion SPECT. Dementia And Geriatric Cognitive Disorders, 37(5–6), 276–285. https://doi.org/10.1159/000357128.
Sundström, T., Elgh, E., Larsson, A., Näsman, B., Nyberg, L., & Riklund, K. A. (2006). Memory-provoked rCBF-SPECT as a diagnostic tool in Alzheimer’s disease? European Journal Of Nuclear Medicine And Molecular Imaging, 33(1), 73–80. https://doi.org/10.1007/s00259-005-1874-0.
Takahashi, M., Tada, T., Nakamura, T., Koyama, K., & Momose, T. (2019). Efficacy and Limitations of rCBF-SPECT in the diagnosis of Alzheimer’s Disease with Amyloid-PET. Am J Alzheimers Dis Other Demen, 34(5), 314–321. https://doi.org/10.1177/1533317519841192.
Takano, Y., Mutoh, T., Tatewaki, Y., Seki, T., Yamamoto, S., Odagiri, H., Arai, H., & Taki, Y. (2020). Hypoperfusion in the posterior cingulate cortex is associated with lower bone mass density in elderly women with osteopenia and Alzheimer’s disease. Clinical And Experimental Pharmacology And Physiology, 47(3), 365–371. https://doi.org/10.1111/1440-1681.13217.
Takenoshita, S., Hayashi, S., Shinya, T., Miki, T., Yokota, O., Maki, Y., Hattori, H., Yamada, N., & Terada, S. (2020). Sally-Anne test and regional cerebral blood flow in Alzheimer’s disease dementia. Psychogeriatrics, 20(5), 549–556. https://doi.org/10.1111/psyg.12533.
Tanaka, M., Fukuyama, H., Yamauchi, H., Narita, M., Nabatame, H., Yokode, M., Fujimoto, N., Kita, T., & Murakami, M. (2002). Regional cerebral blood flow abnormalities in nondemented patients with memory impairment. Journal Of Neuroimaging, 12(2), 112–118. https://doi.org/10.1111/j.1552-6569.2002.tb00106.x.
Tang, T., Huang, L., Zhang, Y., Li, Z., & Liang, S. (2022). Aberrant pattern of regional cerebral blood flow in mild cognitive impairment: a meta-analysis of arterial spin labeling magnetic resonance imaging. Frontiers In Aging Neuroscience, 14, 961344. https://doi.org/10.3389/fnagi.2022.961344.
Tateno, M., Kobayashi, S., Shirasaka, T., Furukawa, Y., Fujii, K., Morii, H., Yasumura, S., Utsumi, K., & Saito, T. (2008). Comparison of the usefulness of brain perfusion SPECT and MIBG myocardial scintigraphy for the diagnosis of dementia with Lewy bodies. Dementia And Geriatric Cognitive Disorders, 26(5), 453–457. https://doi.org/10.1159/000165918.
Terada, S., Sato, S., Nagao, S., Ikeda, C., Shindo, A., Hayashi, S., Oshima, E., Yokota, O., & Uchitomi, Y. (2013). Trail making test B and brain perfusion imaging in mild cognitive impairment and mild Alzheimer’s disease. Psychiatry Research, 213(3), 249–255. https://doi.org/10.1016/j.pscychresns.2013.03.006.
Tokumitsu, K., Yasui-Furukori, N., Takeuchi, J., Yachimori, K., Sugawara, N., Terayama, Y., Tanaka, N., Naraoka, T., & Shimoda, K. (2021). The combination of MMSE with VSRAD and eZIS has greater accuracy for discriminating mild cognitive impairment from early Alzheimer’s disease than MMSE alone. PLoS One, 16(2), e0247427. https://doi.org/10.1371/journal.pone.0247427.
Tosun, D., Schuff, N., Jagust, W., & Weiner, M. W. (2016). & Alzheimer’’s Disease Neuroimaging, I. Discriminative Power of Arterial Spin Labeling Magnetic Resonance Imaging and 18F-Fluorodeoxyglucose Positron Emission Tomography Changes for Amyloid-beta-Positive Subjects in the Alzheimer’s Disease Continuum. Neurodegener Dis, 16(1–2), 87–94. https://doi.org/10.1159/000439257
Tu, M. C., Chung, H. W., Hsu, Y. H., Yang, J. J., & Wu, W. C. (2022). Stage-Dependent Cerebral Blood Flow and Leukoaraiosis Couplings in Subcortical Ischemic Vascular Disease and Alzheimer’s Disease. Journal Of Alzheimer’S Disease, 86(2), 729–739. https://doi.org/10.3233/JAD-215405.
van de Haar, H. J., Jansen, J. F. A., van Osch, M. J. P., van Buchem, M. A., Muller, M., Wong, S. M., Hofman, P. A. M., Burgmans, S., Verhey, F. R. J., & Backes, W. H. (2016). Neurovascular unit impairment in early Alzheimer’s disease measured with magnetic resonance imaging. Neurobiology Of Aging, 45, 190–196. https://doi.org/10.1016/j.neurobiolaging.2016.06.006.
Wang, H., Golob, E., Bert, A., Nie, K., Chu, Y., Dick, M. B., Mandelkern, M., & Su, M. Y. (2009). Alterations in regional brain volume and individual MRI-guided perfusion in normal control, stable mild cognitive impairment, and MCI-AD converter. J Geriatr Psychiatry Neurol, 22(1), 35–45. https://doi.org/10.1177/0891988708328212.
Warkentin, S., Ohlsson, M., Wollmer, P., Edenbrandt, L., & Minthon, L. (2004). Regional cerebral blood flow in Alzheimer’s disease: classification and analysis of heterogeneity. Dementia And Geriatric Cognitive Disorders, 17(3), 207–214. https://doi.org/10.1159/000076358.
Warwick, J. M. (2004). Imaging of brain function using SPECT. Metabolic Brain Disease, 19(1–2), 113–123. https://doi.org/10.1023/b:mebr.0000027422.48744.a3.
Xie, L., Dolui, S., Das, S. R., Stockbower, G. E., Daffner, M., Rao, H., Yushkevich, P. A., Detre, J. A., & Wolk, D. A. (2016). A brain stress test: cerebral perfusion during memory encoding in mild cognitive impairment. Neuroimage Clin, 11, 388–397. https://doi.org/10.1016/j.nicl.2016.03.002.
Yamaji, S., Ishii, K., Sasaki, M., Imamura, T., Kitagaki, H., Sakamoto, S., & Mori, E. (1997). Changes in cerebral blood flow and oxygen metabolism related to magnetic resonance imaging white matter hyperintensities in Alzheimer’s disease. Journal Of Nuclear Medicine, 38(9), 1471–1474. https://www.ncbi.nlm.nih.gov/pubmed/9293811.
Yamashita, K. I., Taniwaki, Y., Utsunomiya, H., & Taniwaki, T. (2014). Cerebral blood flow reduction associated with orientation for time in amnesic mild cognitive impairment and Alzheimer disease patients. Journal Of Neuroimaging, 24(6), 590–594. https://doi.org/10.1111/jon.12096.
Yew, B., & Nation, D. A. (2017). Cerebrovascular resistance: effects on cognitive decline, cortical atrophy, and progression to dementia. Brain, 140(7), 1987–2001. https://doi.org/10.1093/brain/awx112.
Yoshida, T., Kazui, H., Tokunaga, H., Kito, Y., Kubo, Y., Kimura, N., Morihara, T., Shimosegawa, E., Hatazawa, J., & Takeda, M. (2011). Protein synthesis in the posterior cingulate cortex in Alzheimer’s disease. Psychogeriatrics, 11(1), 40–45. https://doi.org/10.1111/j.1479-8301.2010.00350.x.
Yoshida, T., Mori, T., Shimizu, H., Yoshino, Y., Sonobe, N., Matsumoto, T., Kikuchi, K., Miyagawa, M., Iga, J., Mochizuki, T., & Ueno, S. I. (2017). Neural basis of visual perception and reasoning ability in Alzheimer’s disease: correlation between raven’s Colored Progressive Matrices test and (123) I-IMP SPECT imaging results. International Journal Of Geriatric Psychiatry, 32(4), 407–413. https://doi.org/10.1002/gps.4481.
Zhang, H., Wang, Y., Lyu, D., Li, Y., Li, W., Wang, Q., Li, Y., Qin, Q., Wang, X., Gong, M., Jiao, H., Liu, W., & Jia, J. (2021). Cerebral blood flow in mild cognitive impairment and Alzheimer’s disease: a systematic review and meta-analysis. Ageing Research Reviews, 71, 101450. https://doi.org/10.1016/j.arr.2021.101450.
Zhu, C. C., Fu, S. Y., Chen, Y. X., Li, L., Mao, R. L., Wang, J. Z., Liu, R., Liu, Y., & Wang, X. C. (2020). Advances in drug therapy for Alzheimer’s Disease. Curr Med Sci, 40(6), 999–1008. https://doi.org/10.1007/s11596-020-2281-2.
Zlokovic, B. V. (2011). Neurovascular pathways to neurodegeneration in Alzheimer’s disease and other disorders. Nature Reviews Neuroscience, 12(12), 723–738. https://doi.org/10.1038/nrn3114.
Zurynski, Y., Singer, A., Kraiuhin, C., Gordon, E., Dorsch, N., Landau, P., Howson, A., & Meares, R. (1989). Regional cerebral blood flow measurements in the diagnosis of dementia. Australian And New Zealand Journal Of Medicine, 19(5), 436–442. https://doi.org/10.1111/j.1445-5994.1989.tb00301.x.
Funding
Dr. Risacher receives support from the National Institute on Aging (K01 AG049050, R01 AG061788) and the New Vision Award. Dr. Wu receives support from the National Institute on Aging (R01 AG053993). Dr. Apostolova receives support from NIH, Alzheimer Association, AVID Pharmaceuticals, Life Molecular Imaging, and Roche Diagnostics. Dr. Saykin receives support from multiple NIH grants (P30 AG010133, P30 AG072976, R01 AG019771, R01 AG057739, U01 AG024904, R01 LM013463, R01 AG068193, T32 AG071444, and U01 AG068057 and U01 AG072177). He has also received support from Avid Radiopharmaceuticals, a subsidiary of Eli Lilly (in kind contribution of PET tracer precursor).
Author information
Authors and Affiliations
Contributions
Author contributions included conceptual and study design (CGS, SLR and AJS), literature search and selection of included publications (CGS, PJB), summarization, synthesis, and presentation of results (CGS, PJB), interpretations, conclusions, and overall messaging (all authors), and comments, revisions, and approval for final publication (all authors).
Corresponding author
Ethics declarations
Conflict of interest
Dr. Apostolova receives support in the form of consulting fees from Biogen, Two Labs, IQVIA, NIH, Florida Department of Health, NIH Biobank, Eli Lilly, GE Healthcare, and Eisai; in the form of payment for lectures, etc. from AAN, MillerMed, AiSM, and Health and Hospitality; and in the form of travel and meeting support from Alzheimer’s Association. She also participates on Data Safety Monitoring or Advisory boards for IQVIA, NIA R01 AG061111, UAB Nathan Shock Center, and New Mexico Exploratory ADRC; in leadership roles for Medical Science Council Alzheimer Association Greater IN Chapter, Alzheimer Association Science Program Committee, and FDA PCNS Advisory Committee; stock or stock options Cassava Neurosciences and Golden Seeds, and receipt of materials, etc. from AVID Pharmaceuticals, Life Molecular Imaging, and Roche Diagnostics. Dr. Saykin serves or served on the following: Bayer Oncology (Scientific Advisory Board), Eisai (Scientific Advisory Board), Siemens Medical Solutions USA, Inc. (Dementia Advisory Board), and Springer-Nature Publishing (Editorial Office Support as Editor-in-Chief, Brain Imaging and Behavior). All other authors report no disclosures.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Swinford, C.G., Risacher, S.L., Wu, YC. et al. Altered cerebral blood flow in older adults with Alzheimer’s disease: a systematic review. Brain Imaging and Behavior 17, 223–256 (2023). https://doi.org/10.1007/s11682-022-00750-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-022-00750-6