Abstract
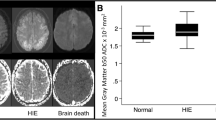
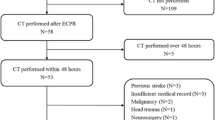
The aim of this study was to use dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) and diffusion-weighted magnetic resonance imaging (DWI) to measure changes in blood–brain barrier (BBB) permeability and cerebral edema over time in a rat model of asphyxial cardiac arrest (ACA). ACA was established by endotracheal tube clamping. Male rats were randomized into a sham group (n = 5) and three ACA groups (n = 18). After return of spontaneous circulation (ROSC), the rats were randomized to perform DWI and DCE-MRI exam in the 6 h, 24 h and 72 h timepoint (ROSC + 6 h, ROSC + 24 h, and ROSC + 72 h). Results shows that fifteen of 18 animals achieved successful resuscitation in the ACA groups. The average apparent diffusion coefficient(ADC) value of the whole brain in ROSC + 6 h was markedly lower than those of the sham, ROSC + 24 h, and ROSC + 72 h. The aquaporin-4(AQP4) score in ROSC + 6 h was significantly higher than those in the other groups, which were negatively correlated with the ADC values. The ratio of whole brain to masseter muscle of volume transfer constant (rKtrans), tissue interstitium-to-plasma rate constant(rKep), and fractional extra-cellular space volume(rVe) in ROSC + 6 h were all significantly higher than those in the sham, ROSC + 24 h, and ROSC + 72 h. The transforming growth factor β1(TGF-β1) and vascular endothelial growth factor A(VEGF-a) scores in ROSC + 6 h were significantly higher than those in the other groups, which were all positively correlated with rKtrans and rKep. In conclusions, brain injury is a frequent complication after CA and resuscitation. DWI and DCE-MRI can quantitatively evaluate brain injury in term of cerebral edema and BBB permeability after successful CPR.





Similar content being viewed by others
Data availability
Data available on request from the corresponding author.
Abbreviations
- ACA:
-
Asphyxial cardiac arrest
- ROSC:
-
Return of spontaneous circulation
- CPR:
-
Cardiopulmonary resuscitation
- BBB:
-
Blood–brain barrier
- DWI:
-
Diffusion-weighted magnetic resonance imaging
- MRS:
-
Magnetic resonance spectroscopy
- DCE-MRI:
-
Dynamic contrast-enhanced magnetic resonance imaging6
- QMR:
-
Quantitative MR
- NDS:
-
Neurology deficit score
- PC:
-
Precordial compression.
References
Aksoy, D., Bammer, R., Mlynash, M., et al. (2013). Magnetic resonance imaging profile of blood-brain barrier injury in patients with acute intracerebral hemorrhage. J Am Heart Assoc, 2, e000161.
Chalkias, A., & Xanthos, T. (2012). Post-cardiac arrest brain injury: Pathophysiology and treatment. Journal of the Neurological Sciences, 315, 1–8.
Drabek, T., Foley, L. M., Janata, A., et al. (2014). Global and regional differences in cerebral blood flow after asphyxial versus ventricular fibrillation cardiac arrest in rats using asl-mri. Resuscitation, 85, 964–971.
Fink, E. L., Panigrahy, A., Clark, R. S., et al. (2013). Regional brain injury on conventional and diffusion weighted mri is associated with outcome after pediatric cardiac arrest. Neurocritical Care, 19, 31–40.
Gong, P., Zhao, S., Wang, J., et al. (2015). Mild hypothermia preserves cerebral cortex microcirculation after resuscitation in a rat model of cardiac arrest. Resuscitation, 97, 109–114.
Hendrickx, H. H., Rao, G. R., Safar, P., et al. (1984). Asphyxia, cardiac arrest and resuscitation in rats. I. Short term recovery. Resuscitation, 12, 97–116.
Nagaraja, T. N., Karki, K., Ewing, J. R., et al. (2010). The MRI-measured arterial input function resulting from a bolus injection of Gd-DTPA in a rat model of stroke slightly underestimates that of Gd-[14C]DTPA and marginally overestimates the blood-to-brain influx rate constant determined by Patlak plots. Magnetic Resonance in Medicine, 63, 1502–1509.
Heye, A. K., Thrippleton, M. J., Armitage, P. A., et al. (2016). Tracer kinetic modelling for dce-mri quantification of subtle blood-brain barrier permeability. NeuroImage, 125, 446–455.
Hirsch, K. G., Mlynash, M., Jansen, S., et al. (2015). Prognostic value of a qualitative brain mri scoring system after cardiac arrest. Journal of Neuroimaging, 25, 430–437.
Iwai, M., Cao, G., Chen, J., et al. (2007). Erythropoietin promotes neuronal replacement through revascularization and neurogenesis after neonatal hypoxia/ischemia in rats. Stroke, 38, 2795–2803.
Jarnum, H., Knutsson, L., Rundgren, M., et al. (2009). Diffusion and perfusion mri of the brain in comatose patients treated with mild hypothermia after cardiac arrest: A prospective observational study. Resuscitation, 80, 425–430.
Laver, S., Farrow, C., Turner, D., et al. (2004). Mode of death after admission to an intensive care unit following cardiac arrest. Intensive Care Medicine, 30, 2126–2128.
Luyt, C. E., Galanaud, D., Perlbarg, V., et al. (2012). Diffusion tensor imaging to predict long-term outcome after cardiac arrest: A bicentric pilot study. Anesthesiology, 117, 1311–1321.
McMillin, M. A., Frampton, G. A., Seiwell, A. P., et al. (2015). Tgfbeta1 exacerbates blood-brain barrier permeability in a mouse model of hepatic encephalopathy via upregulation of mmp9 and downregulation of claudin-5. Laboratory Investigation, 95, 903–913.
Memar, M., Geara, S. J., Hjalmarsson, P., et al. (2018). Long-term mortality and morbidity among 30-day survivors after in-hospital cardiac arrests - a swedish cohort study. Resuscitation, 124, 76–79.
Moler, F. W., Silverstein, F. S., Holubkov, R., et al. (2017). Therapeutic hypothermia after in-hospital cardiac arrest in children. New England Journal of Medicine, 376, 318–329.
Moon, H. K., Jang, J., Park, K. N., et al. (2018). Quantitative analysis of relative volume of low apparent diffusion coefficient value can predict neurologic outcome after cardiac arrest. Resuscitation, 126, 36–42.
Nolan, J. P., Neumar, R. W., Adrie, C., et al. (2008). Post-cardiac arrest syndrome: Epidemiology, pathophysiology, treatment, and prognostication. A scientific statement from the international liaison committee on resuscitation; the american heart association emergency cardiovascular care committee; the council on cardiovascular surgery and anesthesia; the council on cardiopulmonary, perioperative, and critical care; the council on clinical cardiology; the council on stroke. Resuscitation, 79, 350–379.
Pan, A., Kumar, R., Macey, P. M., et al. (2013). Visual assessment of brain magnetic resonance imaging detects injury to cognitive regulatory sites in patients with heart failure. Journal of Cardiac Failure, 19, 94–100.
Pillai, D. R., Dittmar, M. S., Baldaranov, D., et al. (2009). Cerebral ischemia-reperfusion injury in rats–a 3 t mri study on biphasic blood-brain barrier opening and the dynamics of edema formation. Journal of Cerebral Blood Flow and Metabolism, 29, 1846–1855.
Pluta, R., Lossinsky, A. S., Wisniewski, H. M., et al. (1994). Early blood-brain barrier changes in the rat following transient complete cerebral ischemia induced by cardiac arrest. Brain Research, 633, 41–52.
Ramont, L., Thoannes, H., Volondat, A., et al. (2005). Effects of hemolysis and storage condition on neuron-specific enolase (nse) in cerebrospinal fluid and serum: Implications in clinical practice. Clinical Chemistry and Laboratory Medicine, 43, 1215–1217.
Rossetti, A. O., Rabinstein, A. A., & Oddo, M. (2016). Neurological prognostication of outcome in patients in coma after cardiac arrest. Lancet Neurology, 15, 597–609.
Ryoo, S. M., Jeon, S. B., Sohn, C. H., et al. (2015). Predicting outcome with diffusion-weighted imaging in cardiac arrest patients receiving hypothermia therapy: Multicenter retrospective cohort study. Critical Care Medicine, 43, 2370–2377.
Samaniego, E. A., Mlynash, M., Caulfield, A. F., et al. (2011). Sedation confounds outcome prediction in cardiac arrest survivors treated with hypothermia. Neurocritical Care, 15, 113–119.
Sharma, H. S., Miclescu, A., & Wiklund, L. (2011). Cardiac arrest-induced regional blood-brain barrier breakdown, edema formation and brain pathology: A light and electron microscopic study on a new model for neurodegeneration and neuroprotection in porcine brain. Journal of Neural Transmission (Vienna), 118, 87–114.
Shim, J. W., & Madsen, J. R. (2018). Vegf signaling in neurological disorders. International Journalof Molecular Sciences, 19, 275.
Soslow, R. A., Dannenberg, A. J., Rush, D., et al. (2000). Cox-2 is expressed in human pulmonary, colonic, and mammary tumors. Cancer, 89, 2637–2645.
Stammet, P., Collignon, O., Hassager, C., et al. (2015). Neuron-specific enolase as a predictor of death or poor neurological outcome after out-of-hospital cardiac arrest and targeted temperature management at 33 degrees c and 36 degrees c. Journal of the American College of Cardiology, 65, 2104–2114.
Tang, Z. R., Li, C. S., Zhao, H., et al. (2013). Effects of hypothermia on brain injury assessed by magnetic resonance imaging after cardiopulmonary resuscitation in a porcine model of cardiac arrest. American Journal of Emergency Medicine, 31, 86–93.
Tjepkema-Cloostermans, M. C., Hofmeijer, J., Beishuizen, A., et al. (2017). Cerebral recovery index: Reliable help for prediction of neurologic outcome after cardiac arrest. Critical Care Medicine, 45, e789–e797.
Tress, E. E., Clark, R. S., Foley, L. M., et al. (2014). Blood brain barrier is impermeable to solutes and permeable to water after experimental pediatric cardiac arrest. Neuroscience Letters, 578, 17–21.
Vlachos, F., Tung, Y. S., & Konofagou, E. (2011). Permeability dependence study of the focused ultrasound-induced blood-brain barrier opening at distinct pressures and microbubble diameters using dce-mri. Magnetic Resonance in Medicine, 66, 821–830.
Wallin, E., Larsson, I. M., Kristofferzon, M. L., et al. (2018). Acute brain lesions on magnetic resonance imaging in relation to neurological outcome after cardiac arrest. Acta Anaesthesiologica Scandinavica, 62, 635–647.
Wang, P., Li, Y., Yang, Z., et al. (2018). Inhibition of dynamin-related protein 1 has neuroprotective effect comparable with therapeutic hypothermia in a rat model of cardiac arrest. Translational Research, 194, 68–78.
Wijman, C. A., Mlynash, M., Caulfield, A. F., et al. (2009). Prognostic value of brain diffusion-weighted imaging after cardiac arrest. Annals of Neurology, 65, 394–402.
Wissenberg, M., Lippert, F. K., Folke, F., et al. (2013). Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA, 310, 1377–1384.
Wormsbecker, A., Sekhon, M. S., Griesdale, D. E., et al. (2017). The association between anemia and neurological outcome in hypoxic ischemic brain injury after cardiac arrest. Resuscitation, 112, 11–16.
Wu, O., Sorensen, A. G., Benner, T., et al. (2009). Comatose patients with cardiac arrest: Predicting clinical outcome with diffusion-weighted mr imaging. Radiology, 252, 173–181.
Zhu, J., Li, X., Yin, J., et al. (2018). Glycocalyx degradation leads to blood-brain barrier dysfunction and brain edema after asphyxia cardiac arrest in rats. Journal of Cerebral Blood Flow and Metabolism, 38, 1979–1992.
Funding
This study was supported by the research grants from projects of Leading Talents in Pearl River Talent Plan of Guangdong Province (No. 81000-42020004), Guangzhou Science, Technology and Innovation Commission (CN) (No. 202102080580) and Natural Science Foundation of Guangdong Province (No. 2021A1515011433).
Author information
Authors and Affiliations
Contributions
Zhifeng Liu, Tangchun Liu and Jinhui Cai: Performed the experiments, data interpretation, wrote the manuscript.
Gongfa Wu, Gaungyi Wang, Yue Wang and Wanchun Tang: Performed the experiments, data interpretation.
Zhengfei Yang and Qingyu Liu: Study design, data interpretation, edited the manuscript.
All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
The animal experiments were approved by the Institutional Animal Care and Use Committee of the Tang Wanchun Laboratories of Emergency & Critical Care Medicine at Sun Yat-sen Memorial Hospital, Sun Yat-sen University (IACUC-SYSU -R17010).
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, Z., Liu, T., Cai, J. et al. Quantitative magnetic resonance imaging assessment of brain injury after successful cardiopulmonary resuscitation in a rat model of asphyxia cardiac arrest. Brain Imaging and Behavior 16, 270–280 (2022). https://doi.org/10.1007/s11682-021-00500-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-021-00500-0