Abstract
Background
There is a paucity of literature demonstrating which factors are associated with signs of elbow instability on magnetic resonance imaging (MRI) following simple elbow dislocations (SED).
Objectives
This study aimed to evaluate demographic variables and MRI datasets to identify factors associated with elbow instability following SEDs.
Materials and methods
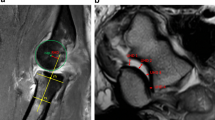
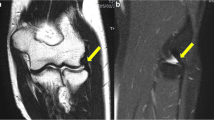
This retrospective multicenter MRI study included patients who had sustained SED and presented within 21 days of trauma. Measurements included ulnohumeral angle, drop sign, and radiocapitellar and ulnohumeral incongruity. The coronoid tip (Regan Morrey type I), lateral collateral ligament (LCL), common extensor origin (CEO), medial collateral ligament (MCL,) and common flexor origin (CFO) were assessed for injuries. Simple and multiple logistic regression analyses were performed to identify factors associated with signs of elbow instability (e.g., ulnohumeral incongruity > 1 mm) on MRI.
Results
A total of 147 patients (68 women, 79 men) with a mean age of 42.9 years (range, 17–85) were included. Of those, 62 patients (42.2%) demonstrated radiocapitellar (> 2 mm) and 36 patients (25.5%) demonstrated ulnohumeral incongruity (> 1 mm); 17 patients (11.6%) had a drop sign (≥ 4 mm). All patients with elbow instability on MRI had injury to the CEO and/or CFO. In multiple logistic regression, an ulnohumeral angle of ≤ 45° (p = 0.005; OR: 4.95), injury to the CEO (p < 0.001; OR: 10.45), CFO (p < 0.001; OR: 8.38), and coronoid tip (p = 0.002; OR: 5.32) were significantly associated with signs of elbow instability on MRI.
Conclusion
Injury to the CEO, CFO, and coronoid tip as well as an ulnohumeral angle of ≤ 45° are associated with signs of elbow instability on MRI following SEDs. If the CEO or CFO is injured, the odds for instability on MRI are increased by a factor of 10 and 8, respectively.
Zusammenfassung
Hintergrund
Wenige Untersuchungen beschäftigen sich mit der Frage, welche Faktoren mit Zeichen der Instabilität in der Magnetresonanztomographie (MRT) nach akuten, einfachen Ellenbogenluxationen vergesellschaftet sind.
Ziel der Arbeit
Ziel der Arbeit war es, demografische Daten und MRT-Datensätze auszuwerten, um Faktoren zu identifizieren, die mit einer Instabilität nach akuten, einfachen Ellenbogenluxationen einhergehen.
Material und Methoden
Patienten, die eine akute, einfache Ellenbogenluxationen erlitten und innerhalb von 21 Tagen mit MRT vorstellig wurden, wurden in diese retrospektive Multizenterstudie eingeschlossen. Der ulnohumerale Winkel, das „drop sign“, radiocapitellare und ulnohumerale Inkongruenz wurden gemessen. Die Koronoidspitze (Regan-Morrey-Typ I), das laterale (LCL) und mediale Kollateralband (MCL) sowie der Extensoren- (CEO) und Flexorenansatz (CFO) wurden auf Verletzungen geprüft. Einfache und multivariate logistische Regression wurden durchgeführt, um zu identifizieren, welche Variablen mit Ellenbogeninstabilität in der MRT (ulnohumerale Inkongruenz > 1 mm) einhergehen.
Ergebnisse
Insgesamt 147 Patienten (68 Frauen, 79 Männer) mit einem Durchschnittsalter von 42,9 Jahren (17–85 Jahre) wurden in die Auswertung einbezogen. Davon zeigten 62 Patienten (42,2 %) radiocapitellare Inkongruenz (> 2 mm), 36 Patienten (25,5 %) zeigten ulnohumerale Inkongruenz (> 1 mm) und 17 Patienten (11,6 %) wiesen ein „drop sign“ (≥ 4 mm) auf. Alle Patienten mit Ellenbogeninstabilität in der MRT hatten Verletzungen des CEO und/oder CFO. Variablen, die sich in der einfachen logistischen Regression als signifikant erwiesen, wurden in ein multivariates logistisches Modell übertragen. Hier blieben ein ulnohumeraler Winkel ≤ 45° (p = 0,005; Odds Ratio, OR: 4,95), Verletzungen des CEO (p < 0,001; OR: 10,45), CFO (p < 0,001; OR: 8,38) und der Koronoidspitze (p = 0,002; OR: 5,32) signifikant mit Zeichen von Ellenbogeninstabilität in der MRT vergesellschaftet.
Schlussfolgerung
Verletzungen des CEO, CFO, der Koronoidspitze und ein ulnohumeraler Winkel von ≤ 45° sind signifikant mit Zeichen von Ellenbogeninstabilität in der MRT nach akuten, einfachen Ellenbogenluxationen vergesellschaftet. Ist der CEO oder CFO verletzt, so erhöht sich das Risiko für Instabilität in der MRT um den Faktor 10 bzw. 8.




Similar content being viewed by others
References
Acosta Batlle J, Cerezal L, López Parra MD et al (2019) The elbow: review of anatomy and common collateral ligament complex pathology using MRI. Insights Imaging 10:43
Adams JE (2020) Elbow instability: evaluation and treatment. Hand Clin 36:485–494
Adolfsson LE, Nestorson JO, Scheer JH (2017) Extensive soft tissue lesions in redislocated after simple elbow dislocations. J Shoulder Elbow Surg 26:1294–1297
Anakwe RE, Middleton SD, Jenkins PJ et al (2011) Patient-reported outcomes after simple dislocation of the elbow. J Bone Joint Surg Am 93:1220–1226
Buchanan TS, Delp SL, Solbeck JA (1998) Muscular resistance to varus and valgus loads at the elbow. J Biomech Eng 120:634–639
Cho CH, Kim BS, Yi J et al (2020) Common extensor complex is a predictor to determine the stability in simple posterolateral elbow dislocation: analysis of MR images of stable vs. Unstable dislocation. J Clin Med 9: https://doi.org/10.3390/jcm9103094
Coonrad RW, Roush TF, Major NM et al (2005) The drop sign, a radiographic warning sign of elbow instability. J Shoulder Elbow Surg 14:312–317
De Haan J, Schep NW, Tuinebreijer WE et al (2010) Simple elbow dislocations: a systematic review of the literature. Arch Orthop Trauma Surg 130:241–249
Demino C, Fowler JR (2020) Magnetic resonance imaging findings after elbow dislocation: a descriptive study. Hand. https://doi.org/10.1177/1558944720949961
Duckworth AD, Ring D, Kulijdian A et al (2008) Unstable elbow dislocations. J Shoulder Elbow Surg 17:281–286
Dunning CE, Zarzour ZD, Patterson SD et al (2001) Muscle forces and pronation stabilize the lateral ligament deficient elbow. Clin Orthop Relat Res 388:118–124
Dutto E, Artiaco S, Gallo A et al (2020) MRI in acute simple elbow dislocations: correlation of preoperative imaging and intraoperative findings of collateral ligaments and associated soft tissue injuries. Musculoskelet Surg. https://doi.org/10.1007/s12306-020-00678-4
Hackl M, Leschinger T, Müller LP et al (2016) Chronic ligamentous instability of the elbow. Orthopade 45:809–821
Hackl M, Wegmann K, Ries C et al (2015) Reliability of magnetic resonance imaging signs of posterolateral rotatory instability of the elbow. J Hand Surg Am 40:1428–1433
Hildebrand KA, Patterson SD, King GJ (1999) Acute elbow dislocations: simple and complex. Orthop Clin North Am 30:63–79
Josefsson PO, Johnell O, Gentz CF (1984) Long-term sequelae of simple dislocation of the elbow. J Bone Joint Surg Am 66:927–930
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Luokkala T, Temperley D, Basu S et al (2019) Analysis of magnetic resonance imaging-confirmed soft tissue injury pattern in simple elbow dislocations. J Shoulder Elbow Surg 28:341–348
Micic I, Kim SY, Park IH et al (2009) Surgical management of unstable elbow dislocation without intra-articular fracture. Int Orthop 33:1141–1147
Modi CS, Wasserstein D, Mayne IP et al (2015) The frequency and risk factors for subsequent surgery after a simple elbow dislocation. Injury 46:1156–1160
O’driscoll SW (1994) Elbow instability. Hand Clin 10:405–415
O’Driscoll SW, Morrey BF, Korinek S et al (1992) Elbow subluxation and dislocation. A spectrum of instability. Clin Orthop Relat Res 280:186–197
Park MC, Ahmad CS (2004) Dynamic contributions of the flexor-pronator mass to elbow valgus stability. J Bone Joint Surg Am 86:2268–2274
Pataky TC, Robinson MA, Vanrenterghem J (2013) Vector field statistical analysis of kinematic and force trajectories. J Biomech 46:2394–2401
Pipicelli JG, King GJW (2020) Rehabilitation of Elbow Instability. Hand Clin 36:511–522
Regan W, Morrey B (1989) Fractures of the coronoid process of the ulna. J Bone Joint Surg Am 71:1348–1354
Ring D, Jupiter JB (2002) Fracture-dislocation of the elbow. Hand Clin 18:55–63
Robinson PM, Griffiths E, Watts AC (2017) Simple elbow dislocation. Shoulder Elbow 9:195–204
Safran MR, Baillargeon D (2005) Soft-tissue stabilizers of the elbow. J Shoulder Elbow Surg 14:179s–185s
Schnetzke M, Aytac S, Keil H et al (2017) Unstable simple elbow dislocations: medium-term results after non-surgical and surgical treatment. Knee Surg Sports Traumatol Arthrosc 25:2271–2279
Schnetzke M, Aytac S, Studier-Fischer S et al (2015) Initial joint stability affects the outcome after conservative treatment of simple elbow dislocations: a retrospective study. J Orthop Surg Res 10:128
Schnetzke M, Bergmann M, Wegmann K et al (2018) Determination of elbow laxity in a sequential soft-tissue injury model: a cadaveric study. J Bone Joint Surg Am 100:564–571
Schnetzke M, Ellwein A, Maier D et al (2020) Injury patterns following simple elbow dislocation: radiological analysis implies existence of a pure valgus dislocation mechanism. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03541-0
Schnetzke M, Schüler S, Hoffend J et al (2017) Interobserver and intraobserver agreement of ligamentous injuries on conventional MRI after simple elbow dislocation. BMC Musculoskelet Disord 18:85
Schreiber JJ, Potter HG, Warren RF et al (2014) Magnetic resonance imaging findings in acute elbow dislocation: insight into mechanism. J Hand Surg Am 39:199–205
Seiber K, Gupta R, Mcgarry MH et al (2009) The role of the elbow musculature, forearm rotation, and elbow flexion in elbow stability: an in vitro study. J Shoulder Elbow Surg 18:260–268
Tarallo L, Merolla G, Porcellini G et al (2020) Acute elbow dislocation: comparison between magnetic resonance imaging and intra-operative finding of ligament injury. Int Orthop 45:265–273. https://doi.org/10.1007/s00264-020-04875-5
Terada N, Yamada H, Toyama Y (2004) The appearance of the lateral ulnar collateral ligament on magnetic resonance imaging. J Shoulder Elbow Surg 13:214–216
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
P.-C. Nolte, D. Maier, F.C. Wagner, A. Ellwein, R.-O. DeyHazra, T. Guehring, K. Müller, P.-A. Grützner, and M. Schnetzke declare that they have no competing interests.
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee (Ethics Committee Rhineland-Palatinate, No. 837.084.14[9323-F]) and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Availability of data and material: data from this work are available upon reasonable request.

Scan QR code & read article online
Rights and permissions
About this article
Cite this article
Nolte, PC., Maier, D., Wagner, F.C. et al. Structural injuries correlate with radiographic signs of instability on MRI after simple elbow dislocations. Obere Extremität 16, 203–209 (2021). https://doi.org/10.1007/s11678-021-00651-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11678-021-00651-y
Keywords
- Joint instability
- Joint dislocations
- Medial collateral ligament
- Lateral collateral ligament
- Magnetic resonance imaging