Abstract
Summary
This study aimed to identify risk factors for the collapse of osteoporotic vertebral fractures (OVFs). We analyzed data from conventional radiography and computed tomography in patients with OVFs and found that older age and two radiological measurements were predictive for vertebral collapse. These factors can be useful for clinical practice.
Purpose
To identify risk factors for collapse of osteoporotic vertebral fractures (OVF) on computed tomography (CT) and conventional radiography (CR).
Methods
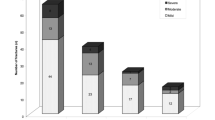
This is a retrospective case–control study including a series of patients with OVF diagnosed at the emergency department of our institution from January to September 2019. Inclusion criteria were to have standing CR and supine CT within 2 weeks after the diagnosis of OVF and a follow-up CR at 6 months or later. We evaluated different imaging measurements at the initial diagnostic examinations, including vertebral height loss, local kyphosis, vertebral density, and fracture type according to the grading systems of Genant, Sugita, Association of Osteosynthesis (AO) Spine, and the German Society for Orthopaedics and Trauma. Vertebral collapse was defined as loss of ≥ 50% of vertebral area or height. Cases and controls were defined as OVFs which collapse and do not collapse, respectively, on follow-up.
Results
Fifty-six patients were included in the study, with a mean age of 72.6 ± 1.2 years, including 48 women. Twenty-five (44.6%) OVFs developed collapse on follow-up. None of the fracture classification systems were found to be predictive of collapse. Multivariate analysis showed that older age, increased density ratio (≥ 2) between the fractured and non-fractured vertebral bodies, and a ≥ 6% difference in posterior vertebral height (PVH) loss between standing CR and supine CT exhibited 88% discriminative power in predicting vertebral collapse.
Conclusions
Age over 72.5 years, a density ratio ≥ 2 between the fractured and non-fractured vertebral bodies, and a difference equal to or higher than 6% in PVH loss between standing CR and supine CT, are risk factors for developing vertebral collapse after OVF.





Similar content being viewed by others
Data Availability
All data used in this work are available upon reasonable request to the corresponding author.
References
Diacinti D, Guglielmi G (2019) How to define an osteoporotic vertebral fracture? Quant Imaging Med Surg 9(9):1485–1494. https://doi.org/10.21037/qims.2019.09.10
LeBoff MS, Greenspan SL, Insogna KL, Lewiecki EM, Saag KG, Singer AJ, Siris ES (2022) The clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 33(10):2049–2102. https://doi.org/10.1007/s00198-021-05900-y
Wáng YXJ, Santiago FR, Deng M, Nogueira-Barbosa MH (2017) Identifying osteoporotic vertebral endplate and cortex fractures. Quant Imaging Med Surg 7:555–591. https://doi.org/10.21037/QIMS.2017.10.05
Le Huec JC, Thompson W, Mohsinaly Y et al (2019) Sagittal balance of the spine. Eur Spine J 28:1889–1905. https://doi.org/10.1007/S00586-019-06083-1
Oei L, Rivadeneira F, Ly F et al (2013) Review of radiological scoring methods of osteoporotic vertebral fractures for clinical and research settings. Eur Radiol 23:476–486. https://doi.org/10.1007/s00330-012-2622-z
Karul M, Bannas P, Schoennagel BP, Hoffmann A, Wedegaertner U, Adam G, Yamamura J (2013) Fractures of the thoracic spine in patients with minor trauma: comparison of diagnostic accuracy and dose of biplane radiography and MDCT. Eur J Radiol 82(8):1273–1277. https://doi.org/10.1016/j.ejrad.2013.01.016
Jung CW, Lee J, Ham DW, Kang H, Chang DG, Kim YB, Ahn YJ, Shim JH, Song KS (2022) Forward bending in supine test: diagnostic accuracy for acute vertebral fragility fracture. Healthcare (Basel) 10(7):1215. https://doi.org/10.3390/healthcare10071215
Lentle B, Trollip J, Lian K (2016) The radiology of osteoporotic vertebral fractures redux. J Clin Densitom 19:40–47. https://doi.org/10.1016/J.JOCD.2015.08.009
Pickhardt PJ, Lee LJ, Muñoz Del Rio A et al (2011) Simultaneous screening for osteoporosis at CT colonography: bone mineral density assessment using MDCT attenuation techniques compared with the DXA reference standard. J Bone Miner Res 26:2194–2203. https://doi.org/10.1002/JBMR.428
Pickhardt PJ, Pooler BD, Lauder T et al (2013) Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann Intern Med 158:588–595. https://doi.org/10.7326/0003-4819-158-8-201304160-00003
Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG (2011) Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am 93(11):1057–1063. https://doi.org/10.2106/JBJS.J.00160
Zou D, Ye K, Tian Y et al (2020) Characteristics of vertebral CT Hounsfield units in elderly patients with acute vertebral fragility fractures. Eur Spine J 29:1092–1097. https://doi.org/10.1007/S00586-020-06363-1
Tsujio T, Nakamura H, Terai H et al (2011) Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion: a prospective multicenter study. Spine (Phila Pa 1976) 36:1229–1235. https://doi.org/10.1097/BRS.0B013E3181F29E8D
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148. https://doi.org/10.1002/JBMR.5650080915
Sugita M, Watanabe N, Mikami Y et al (2005) Classification of vertebral compression fractures in the osteoporotic spine. J Spinal Disord Tech 18:376–381. https://doi.org/10.1097/01.BSD.0000168716.23440.61
Schnake KJ, Blattert TR, Hahn P et al (2018) Classification of osteoporotic thoracolumbar spine fractures: recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Glob spine J 8:46S-49S. https://doi.org/10.1177/2192568217717972
Blattert TR, Schnake KJ, Gonschorek O et al (2018) Nonsurgical and surgical management of osteoporotic vertebral body fractures: recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Glob Spine J 8:50S-55S. https://doi.org/10.1177/2192568217745823
Palmowski Y, Balmer S, Hu Z et al (2022) Relationship between the OF classification and radiological outcome of osteoporotic vertebral fractures after kyphoplasty. Glob Spine J 12:646–653. https://doi.org/10.1177/2192568220964051
Yaman O, Zileli M, Şentürk S et al (2021) Kyphosis after thoracolumbar spine fractures: WFNS Spine Committee Recommendations. Neurospine 18:681–692. https://doi.org/10.14245/NS.2142340.170
Curfs I, Grimm B, van der Linde M et al (2016) Radiological prediction of posttraumatic kyphosis after thoracolumbar fracture. Open Orthop J 10:135–142. https://doi.org/10.2174/1874325001610010135
Viswanathan VK, Shetty AP, Sindhiya N et al (2022) Prospective study to identify the clinical and radiologic factors predictive of pseudarthrosis development in patients with osteoporotic vertebral fractures. World Neurosurg 167:e350–e359. https://doi.org/10.1016/J.WNEU.2022.08.011
Inose H, Kato T, Ichimura S, Nakamura H, Hoshino M, Togawa D, Hirano T, Tokuhashi Y, Ohba T, Haro H, Tsuji T, Sato K, Sasao Y, Takahata M, Otani K, Momoshima S, Yuasa M, Hirai T, Yoshii T, Okawa A (2020) Risk factors of nonunion after acute osteoporotic vertebral fractures: a prospective multicenter cohort study. Spine (Phila Pa 1976) 45(13):895–902. https://doi.org/10.1097/BRS.0000000000003413
Wakao N, Sakai Y, Watanabe T, Osada N, Sugiura T, Iida H, Ozawa Y, Murotani K (2023) Spinal pseudoarthrosis following osteoporotic vertebral fracture: prevalence, risk factors, and influence on patients’ activities of daily living 1 year after injury. Arch Osteoporos 18(1):45. https://doi.org/10.1007/s11657-023-01236-8
Vaccaro AR, Oner C, Kepler CK et al (2013) AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976) 38:2028–2037. https://doi.org/10.1097/BRS.0B013E3182A8A381
Santiago FR, Muñoz PT, Sánchez EM et al (2016) Classifying thoracolumbar fractures: role of quantitative imaging. Quant Imaging Med Surg 6:772–784. https://doi.org/10.21037/QIMS.2016.12.04
von Elm E, Altman DG, Egger M et al (2008) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61:344–349. https://doi.org/10.1016/J.JCLINEPI.2007.11.008
Ha KY, Kim YH (2013) Risk factors affecting progressive collapse of acute osteoporotic spinal fractures. Osteoporos Int 24:1207–1213. https://doi.org/10.1007/S00198-012-2065-Z
Hinde K, Maingard J, Hirsch JA et al (2020) Mortality outcomes of vertebral augmentation (vertebroplasty and/or balloon kyphoplasty) for osteoporotic vertebral compression fractures: a systematic review and meta-analysis. Radiology 295:96–103. https://doi.org/10.1148/RADIOL.2020191294
Pishnamaz M, Curfs I, Balosu S et al (2015) Two-nation comparison of classification and treatment of thoracolumbar fractures: an Internet-based multicenter study among spine surgeons. Spine (Phila Pa 1976) 40:1749–1756. https://doi.org/10.1097/BRS.0000000000001143
Firanescu CE, de Vries J, Lodder P et al (2019) Percutaneous Vertebroplasty is no Risk Factor for New Vertebral Fractures and Protects Against Further Height Loss (VERTOS IV). Cardiovasc Intervent Radiol 42:991–1000. https://doi.org/10.1007/s00270-019-02205-w
Farrokhi MR, Alibai E, Maghami Z (2011) Randomized controlled trial of percutaneous vertebroplasty versus optimal medical management for the relief of pain and disability in acute osteoporotic vertebral compression fractures. J Neurosurg Spine 14:561–569. https://doi.org/10.3171/2010.12.SPINE10286
Joaquim AF, Daubs MD, Lawrence BD et al (2013) Retrospective evaluation of the validity of the Thoracolumbar Injury Classification System in 458 consecutively treated patients. Spine J 13:1760–1765. https://doi.org/10.1016/J.SPINEE.2013.03.014
Wáng YXJ (2022) An update of our understanding of radiographic diagnostics for prevalent osteoporotic vertebral fracture in elderly women. Quant Imaging Med Surg 12(7):3495–3514. https://doi.org/10.21037/qims-22-360
Kanchiku T, Imajo Y, Suzuki H, et al (2014) Usefulness of an early MRI-based classification system for predicting vertebral collapse and pseudoarthrosis after osteoporotic vertebral fractures. J Spinal Disord Tech 27 https://doi.org/10.1097/BSD.0B013E318292B509
Kim DY, Lee SH, Jang JS et al (2004) Intravertebral vacuum phenomenon in osteoporotic compression fracture: report of 67 cases with quantitative evaluation of intravertebral instability. J Neurosurg 100:24–31. https://doi.org/10.3171/SPI.2004.100.1.0024
Peh WCG, Gelbart MS, Gilula LA, Peck DD (2003) Percutaneous vertebroplasty: treatment of painful vertebral compression fractures with intraosseous vacuum phenomena. AJR Am J Roentgenol 180:1411–1417. https://doi.org/10.2214/AJR.180.5.1801411
Kaneda K, Asano S, Hashimoto T et al (1992) The treatment of osteoporotic-posttraumatic vertebral collapse using the Kaneda device and a bioactive ceramic vertebral prosthesis. Spine (Phila Pa 1976) 17:295–303. https://doi.org/10.1097/00007632-199208001-00015
Baba H, Maezawa Y, Kamitani K et al (1995) Osteoporotic vertebral collapse with late neurological complications. Paraplegia 33:281–289. https://doi.org/10.1038/SC.1995.64
Cho JH, Shin SI, Lee JH et al (2013) Usefulness of prone cross-table lateral radiographs in vertebral compression fractures. Clin Orthop Surg 5:195–201. https://doi.org/10.4055/CIOS.2013.5.3.195
McKiernan F, Jensen R, Faciszewski T (2003) The dynamic mobility of vertebral compression fractures. J Bone Miner Res 18:24–29. https://doi.org/10.1359/JBMR.2003.18.1.24
Hoshino M, Tsujio T, Terai H, Namikawa T, Kato M, Matsumura A, Suzuki A, Takayama K, Takaoka K, Nakamura H (2013) Impact of initial conservative treatment interventions on the outcomes of patients with osteoporotic vertebral fractures. Spine (Phila Pa 1976) 38(11):E641-8. https://doi.org/10.1097/BRS.0b013e31828ced9d
Lee SJ, Binkley N, Lubner MG et al (2016) Opportunistic screening for osteoporosis using the sagittal reconstruction from routine abdominal CT for combined assessment of vertebral fractures and density. Osteoporos Int 27:1131–1136. https://doi.org/10.1007/S00198-015-3318-4
Lee H, Park S, Kwack KS et al (2023) CT and MR for bone mineral density and trabecular bone score assessment in osteoporosis evaluation. Sci Rep 13(1):16574. https://doi.org/10.1038/s41598-023-43850-z
Emohare O, Cagan A, Morgan R et al (2014) The use of computed tomography attenuation to evaluate osteoporosis following acute fractures of the thoracic and lumbar vertebra. Geriatr Orthop Surg Rehabil 5:50–55. https://doi.org/10.1177/2151458514525042
Fink HA, Litwack-Harrison S, Ensrud KE, Shen J, Schousboe JT, Cawthon PM, Cauley JA, Lane NE, Taylor BC, Barrett-Connor E, Kado DM, Cummings SR, Marshall LM, Osteoporotic Fractures in Men (MrOS) Study Group (2017) Association of incident, clinically undiagnosed radiographic vertebral fractures with follow-up back pain symptoms in older men: the Osteoporotic Fractures in Men (MrOS) Study. J Bone Miner Res 32(11):2263–2268. https://doi.org/10.1002/jbmr.3215
Sawicki P, Tałałaj M, Życińska K, Zgliczyński WS, Bogołowska-Stieblich A, Krakowiak J, Wierzba W (2021) Characteristics of osteoporotic vertebral fractures in association with symptomatic status in postmenopausal women - a retrospective study of a single centre in Poland. Ann Agric Environ Med 28(4):654–658. https://doi.org/10.26444/aaem/133230
de Klerk G, Hegeman JH, Bronkhorst P, van der Palen J, van der Velde D, Duis HJ (2012) The (a)-symptomatic vertebral fracture: a frequently discovered entity with clinical relevance in fracture patients screened on osteoporosis. Geriatr Orthop Surg Rehabil 3(2):74–78. https://doi.org/10.1177/2151458512449833
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ruiz Santiago, F., Láinez Ramos-Bossini, A.J. & Moraleda-Cabrera, B. Factors influencing vertebral collapse in osteoporotic vertebral fractures: a case–control study of symptomatic patients attended in the emergency department. Arch Osteoporos 19, 6 (2024). https://doi.org/10.1007/s11657-023-01365-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-023-01365-0