Abstract
Summary
Among women ≥ 50 years with fracture, 76% had not received osteoporosis diagnosis or treatment at 6 months and only 14% underwent a DXA scan. Nearly half of all and 90% of hip fracture patients required surgery. Fractures cause substantial clinical burden and are not linked to osteoporosis diagnosis or treatment.
Purpose
Osteoporosis (OP) and OP-related fractures are a major public health concern, associated with significant economic burden. This study describes management patterns following a nontraumatic fracture for commercially insured patients.
Methods
This retrospective cohort study identified women aged ≥ 50 years having their first nontraumatic index fracture (IF) between January 1, 2015 and June 30, 2019, from IQVIA’s PharMetrics® Plus claims database. Medical management patterns at month 6 and medication use patterns at months 6, 12, and 24 following the IF were described.
Results
Among 48,939 women (mean (SD) age: 62.7 (9.5) years), the most common fracture types were vertebral (30.6%), radius/ulna (24.9%), and hip (HF; 12.1%). By month 6, 76% of patients had not received an OP diagnosis or treatment, 13.6% underwent a DXA scan, and 11.2% received any OP treatment. Surgery was required in 43.1% of all patients and 90.0% of HF patients on or within 6 months of the fracture date. Among HF patients, 41.4% were admitted to a skilled nursing facility, 96.7% were hospitalized an average of 5.5 days, and 38.1% required durable medical equipment use. The 30-day all-cause readmission rate was 14.3% among those hospitalized for the IF. Overall, 7.4%, 9.9%, and 13.2% had a subsequent fracture at months 6, 12, and 24, respectively.
Conclusion
Our findings provide an overview of post-fracture management patterns using real-world data. OP was remarkably underdiagnosed and undertreated following the initial fracture. Nontraumatic fracture, particularly HF, resulted in substantial ongoing clinical burden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Osteoporosis (OP) and OP-related fractures are a major public health problem in the USA, which reduce quality of life (QoL), increase psycho-social impairment, and increase financial expenditures [1, 2]. Fracture is associated with an increased rate of hospital admissions, utilization of nursing home and rehabilitation facilities, and an annual societal cost including both direct medical costs and indirect costs of approximately 57 billion USD in 2018, which is projected to increase to over $95 billion in 2040 with a growing aging US population [3,4,5].
In women, the lifetime risk of sustaining a nontraumatic fracture has been estimated around 40 to 50% [4, 6]. Risk factors for OP-related fractures include history of falls and fracture, smoking and alcohol use, some specific diseases, low calcium intake, and the use of certain classes of medications [4]. Patients with a history of fracture are 80% more likely to experience a subsequent fracture compared to those without prior fracture history, which increases the medical costs by 2–6 times [7,8,9]. Early diagnosis of OP and initiation of pharmacotherapy play a significant role in reducing fracture rate and relevant costs [10, 11]. The American Association of Clinical Endocrinologists (AACE) guidelines recommend pharmacotherapy for the patients with OP considered “high” or “very high” risk of fracture [12]. While those who experience a nontraumatic fracture are considered to be at very high risk of fracture, most patients presenting with incident nontraumatic fractures are neither assessed nor treated for osteoporosis to reduce their risk of subsequent fractures, despite the availability of effective treatments [13]. Recent reports indicate that only about 20% of patients with a fracture receive treatment to reduce the risk of subsequent fractures [14, 15]. Effective management of these fractures requires appropriate management of the underlying osteoporosis along with acute treatment for fractures [13].
Management patterns of nontraumatic fracture have been explored to some extent in the real-world setting, mostly among patients enrolled in public health plans [16,17,18]. One analysis in fee-for-service Medicare patients reported post-acute care utilization measures such as home health, outpatient visits, and rehabilitation, but outpatient pharmacy utilization was not assessed [17]. Another inpatient analysis of Medicare patients with hip fracture reported the type of inpatient treatment (e.g. fixation, arthroplasty, etc.) as well as inpatient rehabilitation measures [18]. However, this analysis was not extended to report medical or pharmacy utilization in the outpatient setting among the 73.2% of patients who were ultimately discharged.
Liu et al. previously assessed the clinical and economic burden of osteoporotic fracture among elderly female Medicare beneficiaries and found that less than 30% of the fracture cohort had osteoporosis medication use in the first year of follow-up [19]. These prior studies focused on Medicare beneficiaries; data are lacking for the medical management patterns following a nontraumatic fracture for commercially insured patients. This study addresses this knowledge gap and helps develop a holistic understanding of nontraumatic fracture management by analyzing real-world management patterns.
Methods
Study design and databases
This was a retrospective cohort study using IQVIA PharMetrics® Plus health plan claims database. The aggregated IQVIA PharMetrics Plus database is a nationally representative commercial claims database which comprises adjudicated medical and pharmacy claims of patients in the USA and is sourced directly from the commercial payers [20]. In addition to those with other commercial health plans (HMO, PPO etc.), the database also includes patients eligible for Medicare Advantage plans and does not include those eligible for Medicare fee-for-service, with or without Medigap Part B coverage. The overall study period was from January 1, 2014 to December 31, 2019. The index period was from January 1, 2015 to June 30, 2019, to allow for 1-year pre-index and a minimum of 6-month post-index period, with the index date defined as the first occurrence of hip, vertebral, or non-hip non-vertebral (NHNV) fracture in the inpatient or outpatient setting during the index period. NHNV fracture included fracture of ankle, clavicle, femur, humerus, pelvis, radius/ulna, and tibia/fibula. Patients’ demographic and baseline clinical characteristics were assessed during the 1-year pre-index period. The medical management patterns were described at month 6 and treatment patterns were reported at months 6, 12, and 24 following the index nontraumatic fracture.
Inclusion and exclusion criteria
Patients eligible for inclusion were women aged 50 years and older with a hip, vertebral, or NHNV fracture in the inpatient or outpatient settings between January 1, 2015 and June 30, 2019 (Fig. 1). Patients were required to be continuously enrolled with both medical and outpatient pharmacy benefits during the 1-year period prior to the index fracture date and for at least 6-month post-index. Patients with trauma diagnosis on the same day as index fracture, or with pre-index nontraumatic fracture or with a diagnosis of Paget’s disease of bone, osteitis deformans, known primary bone diseases other than postmenopausal OP, or metabolic bone diseases, or with a pre-index diagnosis of cancer (excluding non-melanoma skin cancer) during the study period were excluded from the study.
The fracture identification algorithm identified nontraumatic fractures and employed a combination of ICD-9-CM or ICD-10-CM diagnosis codes and Current Procedural Terminology (CPT) codes and required at least one claim with a relevant ICD-9-CM or ICD-10-CM diagnosis code in either the inpatient or outpatient setting. For outpatient claims, additionally, a corresponding procedure code for fracture treatment at the same anatomic site was also required; with the exception being vertebral fracture, where a corresponding diagnosis code with CPT codes for outpatient physician evaluation and management was sufficient. If there were two or more fractures on the same index date, index fracture was assigned according to the following hierarchy: hip, femur, pelvis, vertebral, humerus, radius/ulna, tibia/fibula, ankle, and clavicle [21]. Subsequent fractures occurring after the index fracture were considered a new fracture if they occurred at a new anatomical site or at the same site as a previous fracture and occurring more than 90-days from the original fracture.
Baseline patient characteristics
Patients’ demographics including age, geographic region, payer type, and clinical characteristics (pre-index claim(s) for DXA scan, pre-index history of fall, pre-index OP diagnosis, pre-index orthopedic surgery, pre-index use of OP medications, pre-index history of smoking, corticosteroid use, Charlson comorbidity index (CCI), and other comorbidities of interest (e.g., osteoarthritis, rheumatoid arthritis, Alzheimer/dementia, depression, ischemic stroke, and other cardiovascular diseases including myocardial infarction) were reported during the 1-year pre-index period.
Study outcomes
Medical management patterns including index fracture hospitalization, post index OP diagnosis, DXA scan, orthopedic surgery, rehabilitation, and all-cause readmission within 30 days post discharge of the hospitalization for index fracture were described at 6 months following the index nontraumatic fracture. Treatment patterns including use of OP medications, discontinuation, and re-initiation of the first OP agent (anabolic agents (teriparatide, abaloparatide, romosozumab) or antiresorptive agents (bisphosphonates, denosumab, selective estrogen receptor modulators SERMs, calcitonin)) following the index nontraumatic fracture, and total months on OP treatment (not including treatment gaps) were described at 6, 12, and 24 months following the index nontraumatic fracture. In addition, occurrence of new subsequent fractures was also evaluated at 6, 12, and 24 months following the index nontraumatic fracture. Discontinuation was defined as an observation of a gap of > 60 days between the end of days of supply and the next fill of the first OP drug class that was initiated following the index fracture event. The last day of medication supply was defined as the discontinuation date. Re-initiation was defined as starting the same drug class after discontinuation (discontinuation and re-initiation were defined at drug class level.)
This retrospective study used only existing de-identified aggregate claims data, therefore informed consent, ethics committee approval, or institutional review board approval were not required. The study complied with all applicable laws regarding patient privacy, using HIPAA-compliant de-identified retrospective data sources.
Statistical analysis
Analyses were conducted using SAS version 9.3 (SAS Institute, Cary, NC, USA). The study was descriptive in nature and formal statistical tests were not conducted. Mean and standard deviation (SD) were generated as measures of central tendency and variance for continuous variables. Frequencies and percentages were calculated for categorical variables.
Results
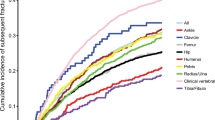
Of the 48,939 women (mean (SD) age: 62.7 (9.5) years) included in the analysis, 13,539 (27.7%) were ≥ 65 years old (Table 1). The most common index fracture type was vertebral (30.6%), followed by radius/ulna (24.9%) and hip (12.1%) (Fig. 2). The inpatient setting was reported for 34.8% of the index fractures. Among all women with incident nontraumatic fractures, 10.8% had OP diagnosis prior to index fracture; 9.7% had DXA scan and 7.3% received OP treatment in the 12-month pre-index period (Table 2).
Management patterns
By month 6 post index nontraumatic fracture, 76% of the patients had not received an OP diagnosis or any treatment for OP, 13.6% underwent a DXA scan, 12.4% of the patients were admitted to a skilled nursing facility (SNF), and 17.1% required DME use within 6 month from the index fracture event. Among the patients who received OP treatment prior to index fracture, the post index DXA scan rate was 15.9% and 40.0% had orthopedic surgery within 6 months from the index fracture. Among the patients with a hip fracture, 90.0% had orthopedic surgery within 6 months of the index fracture, 41.4% were admitted to a SNF, 96.7% were hospitalized for an average of 5.5 days, and 38.1% required durable medical equipment (DME) use within 6 months from the index fracture. The all-cause hospital readmission rate following discharge from the index hospitalization was 14.3% for overall patients and 15.1% for the patients with index hip fracture (Table 3).
Treatment patterns
Overall, 11.2%, 14.3%, and 17.6% of the fracture patients received OP medications within 6, 12, and 24 months post index fracture regardless of their pre-index OP medication use status. Post-index OP medication utilization rate was 68.9–80.8% within 6–24 months following index fracture among the subgroup of patients with pre-index OP medication use. Among patients who were treated post fracture, only 6.3% (6.8%) received anabolic agents, and 93.7% (93.2%) received antiresorptive agents within 6 (12) months following index fracture. In the OP treatment-naïve group, which initiated OP medication within 6 months after fracture, the mean time to OP treatment initiation was 69 days and over 50% of these treatment-naïve patients initiated OP treatment more than 60 days after fracture (Table 4).
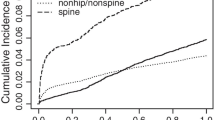
Occurrence of new subsequent fracture
Overall, 7.4%, 9.9%, and 13.2% of the population had a new fracture at months 6, 12, and 24 following the index fracture, respectively (Table 4). In patients with an index vertebral fracture, occurrence of a subsequent fracture within months 6, 12, and 24 was 12.5%, 17.7%, and 23.5%, respectively (Table 5).
Discussion
This study, to our knowledge, is the first to assess relevant OP-related post fracture management patterns among a nationally representative US sample of commercially insured women. Our findings show that the rates for diagnosis and treatment of OP remained low in commercially insured women with nontraumatic fractures, although an increase was noted in OP diagnosis, treatment and DXA scan following the index nontraumatic fracture remained low, which is consistent with previous finding among commercially insured women [22, 23]. Although the post index OP medication utilization rate among the subgroup of patients with pre-index OP treatment or OP diagnosis is higher, it is still suboptimal. In a previous study, it was also found that discontinuation of OP medications is high in clinical practice due to non-compliance and adverse effects, especially gastrointestinal adverse events [24].
Among patients with OP medication use, a majority of the patients received antiresorptive agents, while only a very small proportion of the patients received anabolic agents. Although AACE guidelines recommended anabolic treatments for very high-risk patients or patients with prior fracture, the use of anabolic treatment is still low in real world setting [12].
Overall, the diagnostic and treatment trend in this study were not in agreement with the current treatment guidelines [12], which strongly recommend that postmenopausal women aged 50 years and older with prior fracture should be treated with pharmacotherapy. This observation is similar to findings from earlier studies on OP management, including studies which showed that only 16% of women aged ≥ 55 and 30% of US Medicare beneficiaries (age > 65) received treatment following a fracture episode [25,26,27]. There are many factors that may contribute to underdiagnosis and undertreatment of OP in the USA. One potential reason is that patients and physicians do not recognize that osteoporosis and the underlying fragility of bone require screening and treatment. In addition, the OP treatment rate may be lower in working aged commercially insured women compared to Medicare patients due to the misperception that working-aged women are not affected by OP. On the other hand, limited coordination in post-fracture care programs or a lack of coordinated secondary fracture prevention programs may also play a role [28].
The rate of subsequent fracture was 7.4%, 9.9%, and 13.2% within 6, 12, and 24 months following the index fracture. A similar rate of subsequent fracture was observed in previous study of US Medicare and commercially insured beneficiaries 50 and older, which reported 11.6% of the commercially insured beneficiaries experienced a subsequent fracture within 1 year following the index fracture [6]. In this analysis, it was also noted that among those with index vertebral fracture, the subsequent fracture rate is higher than all other types of fracture. Subsequent fracture was reported to be associated with higher medical costs [29], therefore appropriate treatment for OP is needed to further prevent subsequent fracture, reduce the economic burden and individual human suffering.
For the patients with index hip fracture, the orthopedic surgery rate was 90.0% within 6 months on or after the index-fracture, admission rate to a SNF was 96.7%, DME use was 38.1%, and all cause readmission rate within 30 days post discharge of the index fracture hospitalization was 15.1%, which indicates that hip fracture patients require more intensive post fracture care. The length of stay in the SNF and the total number of occupational and physical therapy minutes may be further investigated in future research.
Limitations
This study has some limitations. Misclassification of patients due to miscoding or misdiagnosis may exist in claims data since these data are mainly for billing and reimbursement purposes, some the medical conditions and outcomes may be documented incorrectly. Secondly, the information of over-the-counter (OTC) treatments such as calcium and vitamin D supplements is lacking in claims data and cannot be captured in this study. Outpatient prescription claims at the health plan level do not necessarily reflect the true utilization of medications. Lastly, underestimation of the subsequent fracture data may exist, given that the requirement of the 90-day gap in the identification of subsequent fractures may not allow inclusion of patients who had a second incident fracture within that time duration. Classification of subsequent vertebral fracture may be overestimated due to the inability in claims data to fully distinguish between the index and subsequent fractures as continuing or separate events. Vertebral fracture is a more chronic condition compared with the more acute fractures such as hip, wrist etc. As the subsequent fracture definition is based on the observation of a subsequent medical claim for a given condition, vertebral fracture was expected to have a higher subsequent fracture (medical claim) rate. While DXA scan orders were captured, DXA values were not available in claims data. Additionally, the number of years from the onset of menopause is unknown, thus an assumption of 50 years old was made for the onset of menopause.
Conclusion
Findings from this study provide an overview of the post fracture management patterns using real-world data. In this younger (≥ 50 years) patient population (compared with a publicly insured population), OP diagnosis was low which may be due to the very low rate of DXA scans. It was also remarkable that even following a nontraumatic fracture, the rate of osteoporosis treatment was lower than 1 in 8. Nontraumatic fracture, particularly hip fracture, resulted in substantial clinical burden during the post-index period. These data suggest that underdiagnosis and undertreatment exist in a younger commercially insured female population, including women under age 65, even lower than in an older, Medicare fee-for-service population [19]. Therefore, improving osteoporosis management (i.e., screening, diagnosis, and treatment) in younger patients is warranted to reduce fragility fracture among this population.
References
Kerr C, Bottomley C, Shingler S, Giangregorio L, de Freitas HM, Patel C, Randall S, Gold DT (2017) The importance of physical function to people with osteoporosis. Osteoporos Int 28(5):1597–1607. https://doi.org/10.1007/s00198-017-3911-9
Marinho BC, Guerra LP, Drummond JB, Silva BC, Soares MM (2014) The burden of osteoporosis in Brazil. Arq Bras Endocrinol Metabol 58(5):434–443. https://doi.org/10.1590/0004-2730000003203
Hansen D, Bazell C, Pelizzari P, Pyenson B (2019) Milliman research report: medicare cost of osteoporotic fractures. The clinical and cost burden of an important consequence of osteoporosis. National Osteoporosis Foundation
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R, National Osteoporosis F (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25(10):2359–2381. https://doi.org/10.1007/s00198-014-2794-2
Zimmerman S, Chandler JM, Hawkes W, Sloane PD, Hebel JR, Magaziner J, Martin AR, Girman CJ (2002) Effect of fracture on the health care use of nursing home residents. Arch Intern Med 162(13):1502–1508. https://doi.org/10.1001/archinte.162.13.1502
Weaver J, Sajjan S, Lewiecki EM, Harris ST, Marvos P (2017) Prevalence and cost of subsequent fractures among U.S. patients with an incident fracture. J Manag Care Spec Pharm 23 (4):461–471. https://doi.org/10.18553/jmcp.2017.23.4.461
Johnell O, Kanis J (2005) Epidemiology of osteoporotic fractures. Osteoporos Int 16(Suppl 2):S3-7. https://doi.org/10.1007/s00198-004-1702-614
Pietri M, Lucarini S (2007) The orthopaedic treatment of fragility fractures. Clin Cases Miner Bone Metab 4(2):108–116
Budhia S, Mikyas Y, Tang M, Badamgarav E (2012) Osteoporotic fractures: a systematic review of U.S. healthcare costs and resource utilization. Pharmacoeconomics 30 (2):147–170. https://doi.org/10.2165/11596880-000000000-00000.
Pisani P, Renna MD, Conversano F, Casciaro E, Di Paola M, Quarta E, Muratore M, Casciaro S (2016) Major osteoporotic fragility fractures: risk factor updates and societal impact. World J Orthop 7(3):171–181. https://doi.org/10.5312/wjo.v7.i3.171
Osteoporosis: risk assessment, management and prevention. https://www.nursingtimesnet/clinical-archive/orthopaedics/osteoporosis-risk-assessment-management-and-prevention-01-02-2019/. Accessed Feb 2019
Camacho PM, Petak SM, Binkley N, Diab DL, Eldeiry LS, Farooki A, Harris ST, Hurley DL, Kelly J, Lewiecki EM, Pessah-Pollack R, McClung M, Wimalawansa SJ, Watts NB (2020) American Association of Clinical Endocrinologists/American College of Endocrinology Clinical Practice Guidelines for the diagnosis and treatment of postmenopausal osteoporosis-2020 update. Endocr Pract 26(Suppl 1):1–46. https://doi.org/10.4158/GL-2020-0524SUPPL
Khan AZ, Rames RD, Miller AN (2018) Clinical management of osteoporotic fractures. Curr Osteoporos Rep 16(3):299–311
Iconaru L, Smeys C, Baleanu F, Kinnard V, Moreau M, Cappelle S, Surquin M, Rubinstein M, Rozenberg S, Paesmans M, Karmali R, Bergmann P, Body JJ (2020) Osteoporosis treatment gap in a prospective cohort of volunteer women. Osteoporos Int 31(7):1377–1382. https://doi.org/10.1007/s00198-020-05339-7
Murphy-Menezes M (2016) The osteoporosis clinical care gap: an opportunity for impact by the clinical pharmacist. Journal of Bone Reports & Recommendations. https://doi.org/10.4172/2469-6684.100017
Budhia S, Mikyas Y, Tang M, Badamgarav E (2012) Osteoporotic fractures. Pharmacoeconomics 30(2):147–170
Becker DJ, Yun H, Kilgore ML et al (2010) Health services utilization after fractures: evidence from Medicare. J Gerontol A Biol Sci Med Sci 65(9):1012–1020
Kumar A, Rahman M, Trivedi AN, Resnik L, Gozalo P, Mor V (2018) Comparing post-acute rehabilitation use, length of stay, and outcomes experienced by Medicare fee-for-service and Medicare Advantage beneficiaries with hip fracture in the United States: a secondary analysis of administrative data. PLoS Med 15(6):e1002592
Liu J, Gong T, Xu X, Fox KM, Oates M, Gandra SR (2022) Heavy clinical and economic burden of osteoporotic fracture among elderly female Medicare beneficiaries. Osteoporos Int 33(2):413–423
Lanteigne A, Sheu YH, Stürmer T, Pate V, Azrael D, Swanson SA, Miller M (2015) Serotonin-norepinephrine reuptake inhibitor and selective serotonin reuptake inhibitor use and risk of fractures: a new-user cohort study among US adults aged 50 years and older CNS drugs 29(3):245–52
Balasubramanian A, Zhang J, Chen L, Wenkert D, Daigle SG, Grauer A, Curtis JR (2019) Risk of subsequent fracture after prior fracture among older women. Osteoporos Int 30(1):79–92
Overman RA, Farley JF, Curtis JR, Zhang J, Gourlay ML, Deal CL (2015) DXA utilization between 2006 and 2012 in commercially insured younger postmenopausal women. J Clin Densitom 18(2):145–149
Weaver J, Sajjan S, Lewiecki EM, Harris ST (2017) Diagnosis and treatment of osteoporosis before and after fracture: a side-by-side analysis of commercially insured and Medicare advantage osteoporosis patients. J Manag Care Spec Pharm 23(7):735–744
Jakob F, Marin F, Martin-Mola E, Torgerson D, Fardellone P, Adami S, ... & Cooper C (2006) Characterization of patients with an inadequate clinical outcome from osteoporosis therapy: the Observational Study of Severe Osteoporosis (OSSO). J Assoc Phys 99(8):531-543
Boudreau DM, Yu O, Balasubramanian A, Wirtz H, Grauer A, Crittenden DB, Scholes D (2017) A survey of women’s awareness of and reasons for lack of postfracture osteoporotic care. J Am Geriatr Soc 65(8):1829–1835. https://doi.org/10.1111/jgs.14921
Yusuf AA, Matlon TJ, Grauer A, Barron R, Chandler D, Peng Y (2016) Utilization of osteoporosis medication after a fragility fracture among elderly Medicare beneficiaries. Arch Osteoporos 11(1):31. https://doi.org/10.1007/s11657-016-0285-0
Lewiecki EM, Ortendahl JD, Vanderpuye-Orgle J, Grauer A, Arellano J, Lemay J, Harmon AL, Broder MS, Singer AJ (2019) Healthcare policy changes in osteoporosis can improve outcomes and reduce costs in the United States. JBMR Plus 3(9):e10192. https://doi.org/10.1002/jbm4.10192
Keshishian A, Boytsov N, Burge R, Krohn K, Lombard L, Zhang X, Xie L, Baser O (2017) Examining the treatment gap and risk of subsequent fractures among females with a fragility fracture in the US Medicare population. Osteoporos Int 28(8):2485–2494. https://doi.org/10.1007/s00198-017-4072-6
Dane Hansen FSA, Pelizzari P, & Bruce Pyenson FSA (2021) Medicare cost of osteoporotic fractures–2021 updated report. The Clinical and Cost Burden of an Important Consequence of Osteoporosis. National Osteoporosis Foundation. Available at https://www.milliman.com/en/insight/-/media/milliman/pdfs/2021-articles/3- 30-21-Medicare-Cost-Osteoporotic-Fractures.ashx
Acknowledgements
The authors would like to thank Kainan Sun for her statistical and programming expertise.
Funding
Amgen and UCB.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Rolin L. Wade is an employee of IQVIA. Xin Wang and Timothy Hill were employees of IQVIA at the time of this research. IQVIA was contracted by Amgen to conduct this study. Mary Oates is an employee and stockholder of Amgen. Xiaoqing Xu was an employee of Amgen at the time of this research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, X., Xu, X., Oates, M. et al. Medical management patterns in a US commercial claims database following a nontraumatic fracture in postmenopausal women. Arch Osteoporos 17, 92 (2022). https://doi.org/10.1007/s11657-022-01135-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-022-01135-4