Abstract
Objective
To assess efficacy of Chinese medicine (CM) on insomnia considering characteristics of treatment based on syndrome differentiation.
Methods
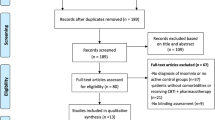
A total of 116 participants aged 18 to 65 years with moderate and severe primary insomnia were randomized to the placebo (n=20) or the CM group (n=96) for a 4-week treatment and a 4-week follow-up. Three CM clinicians independently prescribed treatments for each patient based on syndromes differentiation. The primary outcome was change in total sleep time (TST) from baseline. Secondary endpoints included sleep onset latency (SOL), wake time after sleep onset (WASO), sleep efficiency, Pittsburgh Sleep Quality Index (PSQI) and CM symptoms.
Results
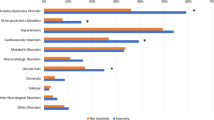
The CM group had an average 0.6 h more (95% confidence interval (CI): 0.3–0.9, P<0.001) TST and 34.1% (10.3%–58.0%, P=0.005) more patients beyond 0.5 h TST increment than that of the placebo group. PSQI was changed −3.3 (−3.8 to −2.7) in the CM group, a −2.0 (−3.2 to −0.8, P<0.001) difference from the placebo group. The CM symptom score in the CM group decreased −2.0 (−3.3 to −0.7, P=0.003) more than the placebo group. SOL and WASO changes were not significantly different between groups. The analysis of prescriptions by these clinicians revealed blood deficiency and Liver stagnation as the most common syndromes. Prescriptions for these clinicians displayed relative stability, while the herbs varied. All adverse events were mild and were not related to study treatment.
Conclusion
CM treatment based on syndrome differentiation can increase TST and improve sleep quality of primary insomnia. It is effective and safe for primary insomnia. In future studies, the long-term efficacy validation and the exploratory of eutherapeutic clinicians’ fixed herb formulas should be addressed (Registration No. NCT01613183).
Similar content being viewed by others
References
Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD, Clinical Guidelines Committee of the American College of Physicians. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians management of chronic insomnia disorder in adults. Ann Intern Med 2016;165:125–133.
Morin CM, Jarrin DC. Epidemiology of insomnia: prevalence, course, risk factors, and public health burden. Sleep Med Clin 2022;17:173–191.
Hasan F, Tu YK, Yang CM, James Gordon C, Wu D, Lee HC, et al. Comparative efficacy of digital cognitive behavioral therapy for insomnia: a systematic review and network meta-analysis. Sleep Med Rev 2022;61:101567.
Zweerde T, Bisdounis L, Kyle SD, Lancee J, van Straten A. Cognitive behavioral therapy for insomnia: a meta-analysis of long-term effects in controlled studies. Sleep Med Rev 2019;48:101208.
Alimoradi Z, Jafari E, Broström A, Ohayon MM, Lin CY, Griffths MD, et al. Effects of cognitive behavioral therapy for insomnia (CBT-I) on quality of life: a systematic review and meta-analysis. Sleep Med Rev 2022;64:101646.
Cheung JMY, Jarrin DC, Ballot O, Bharwani AA, Morin CM. A systematic review of cognitive behavioral therapy for insomnia implemented in primary care and community settings. Sleep Med Rev 2019;44:23–36.
Manber R, Trockel M, Batdorf W, Siebern AT, Taylor CB, Gimeno J. Lessons learned from the national dissemination of cognitive behavioral therapy for insomnia in the Veterans Health Administration: impact of training on therapists’ self-efficacy and attitudes. Sleep Med Clinics 2013;8:399–405.
Madari S, Golebiowski R, Mansukhani MP, Kolla BP. Pharmacological management of insomnia. Neurotherapeutics 2021;18:44–52.
Everitt H, Baldwin DS, Stuart B, Lipinska G, Mayers A, Malizia AL, et al. Antidepressants for insomnia in adults. Cochrane Database Syst Rev 2018;14;5:CD010753.
Misra AK, Sharma PK. Pharmacotherapy of insomnia and current updates. J Assoc Physicians India 2017;65:30–32.
Morin CM, Leblanc M, Daley M, Gregoire JP, Mérette C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med 2006;7:123–130.
Ng JY, Parakh ND. A systematic review and quality assessment of complementary and alternative medicine recommendations in insomnia clinical practice guidelines. BMC Complement Med Ther 2021;8;21:54.
Lee KH, Tsai YT, Lai JN, SK Lin. Concurrent use of hypnotic drugs and Chinese herbal medicine therapies among Taiwanese adults with insomnia symptoms: a population-based study. Evid Based Complement Alternat Med 2013;22:987862.
Ell J, Schmid SR, Benz F, Spille L. Complementary and alternative treatments for insomnia disorder: a systematic umbrella review. J Sleep Res 2023;32:e13979.
Cheng B, Liu Y, Tian J, Gao R, Liu Y. Complementary and alternative medicine for the treatment of insomnia: an overview of scientific evidence from 2008 to 2018. Curr Vasc Pharmacol 2020;18:307–321.
Jiang L, Liu B, Xie Q, Yang S, He L, Zhang R, et al. Investigation into the influence of physician for treatment based on syndrome differentiation. Evid Based Complement Alternat Med 2013; doi: https://doi.org/10.1155/2013/587234.
Yan S, Zhang R, Zhou X, Peng L, He L, Liu B. Exploring effective core drug patterns in primary insomnia treatment with Chinese herbal medicine: study protocol for a randomized controlled trial. Trials 2013;14:1–7.
American Psychiatric Association. DSM-IV-TR: diagnostic and statistical manual of mental disorders, text revision. Washington, DC: American Psychiatric Association; 2000:75.
Spiegel R: Sleep and sleeplessness in advanced age: advances in sleep research. 5th ed. Lancaster UK: MTP Press; 1981:1–272.
Hao J, Wang Y, Wang Y, Zhang J, Gao J, Kang L, et al. Analysis of influencing factors on quality of life in patients with chronic kidney disease undergoing maintenance haemodialysis. Heliyon 2024 3;10:e25817.
Smarr KL, Keefer AL. Measures of depression and depressive symptoms: Beck Depression Inventory-2 (BDI-2), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire-9 (PHQ-9). Arthritis Care Res (Hoboken) 2011;63 Suppl 11:S454–S466.
Zhou X, Poon J, Kwan P, Zhang R, Wang Y, Poon S, et al. Novel two-stage analytic approach in extraction of strong herb-herb interactions in TCM clinical treatment of insomnia. ICMB 2010;6165:258–267.
Sleep Disorders Institution on Sleep Diary. New York: Accessed Sep 11, 2017, Avallable at https://www.sleepny.com/sleepdiary
Alessi C, Martin JL, Fiorentino L, Fung CH, Dzierzewski JM, Rodriguez Tapia JC, et al. Cognitive behavioral therapy for insomnia in older veterans using nonclinician sleep coaches: randomized controlled trial. J Am Geriatr Soc 2016;64:1830–1838.
Tsai PS, Wang SY, Wang MY, Wang MY, Su CT, Yang TT et al. Psychometric evaluation of the Chinese version of the Pittsburgh sleep quality index (CPSQI) in primary insomnia and control subjects. Qual Life Res 2005;14:1943–1952.
Sun YN, Yu CH, Yuan YH, Zhou XZ, Liu Y, Yan SY, et al. Cohort study of evaluating the outcomes of insomnia treated by TCM patterns differentiation among different TCM physicians. J Liaoning Univ Tradit Chin Med (Chin) 2017;19(9):73–77.
Fleming TR, Harrington DP, O’Brien PC. Designs for group sequential tests. Control Clin Trials 1984;5:348–361.
Espie CA, Kyle SD, Williams C, Ong JC, Douglas NJ, Hames P. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep 2012;35:769–781.
Singh A, Zhao K. Treatment of insomnia with traditional Chinese herbal medicine. Int Rev Neurobiol 2017;135:97–115.
Ni X, Shergis JL, Guo X, Zhang AL, Li Y, Lu C, et al. Updated clinical evidence of Chinese herbal medicine for insomnia: a systematic review and meta-analysis of randomized controlled trials. Sleep Med 2015;16:1462–1481.
Birling Y, Jia M, Li G, Sarris J, Bensoussan A, Zhu X. Zao Ren An Shen for insomnia: a systematic review with metaanalysis. Sleep Med 2020;69:41–50.
Yang XQ, Liu L, Ming SP, Fang J, Wu DN. Tian Wang Bu Xin Dan for insomnia: a systematic review of efficacy and safety. Evid Based Complement Alternat Med 2019; 24;2019:4260801.
Acknowledement
We appreciate and acknowledge the clinicians Xu BY, Li QY, and Zhang BL from Xiyuan Hospital, China Academy of Chinese Medical Sciences.
Author information
Authors and Affiliations
Contributions
Yan SY, He LY, and Liu BY led the design of the trial. Liu YJ and Zhu JG treated patients with CM. Zhang RS charged of the randomization through a central randomization system. Li P recruited the participants and collected data. Yan SY, Lu Y, Xiong ZY, and Zhou XZ developed the statistical analysis plan and undertook the analyses. Yan SY and Xiong ZY drafted the paper, with critical input from all other authors. Lu Y acted as guarantors. All authors have read and approved the final draft. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding authors
Ethics declarations
The authors declare that there is no conflict of interest. The funder of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Additional information
Supported by the National Natural Science Foundation of China (No. 81973713 and No. 81303149)
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Xiong, Zy., Lu, Y., He, Ly. et al. Efficacy of Chinese Medicine Treatment Based on Syndrome Differentiation for Primary Insomnia: A Randomized Placebo Controlled Triple-Blinded Trial. Chin. J. Integr. Med. (2024). https://doi.org/10.1007/s11655-024-3661-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s11655-024-3661-4