Abstract
Background
Healthcare systems are increasingly screening and referring patients for unmet social needs (e.g., food insecurity). Little is known about the intensity of support necessary to address unmet needs, how this support may vary by circumstance or time (duration), or the factors that may contribute to this variation.
Objective
Describe health navigator services and the effort required to support patients with complex needs at a community health center in East Oakland, CA.
Design
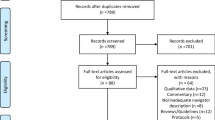
Retrospective analysis of de-identified patient contact notes (e.g., progress notes).
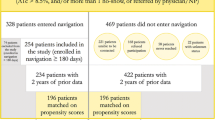
Participants
Convenience sample of patients (n = 27) enrolled in diabetes education and referred to health navigators.
Interventions
Navigators provide education on managing conditions (e.g., diabetes), initiate and track medical and social needs referrals, and navigate patients to medical and social care organizations.
Main Measures
Descriptive statistics for prevalence, mean, median, and range values of patient contacts and navigation services. We described patterns and variation in navigation utilization (both contacts and navigation services) based on types of need.
Key Results
We identified 811 unmet social and medical needs that occurred over 710 contacts with health navigators; 722 navigation services were used to address these needs. Patients were supported by navigators for a median of 9 months; approximately 25% of patients received support for > 1 year. We categorized patients into 3 different levels of social risk, accounting for patient complexity and resource needs. The top tertile (n = 9; 33%) accounted for the majority of resource utilization, based on health navigator contacts (68%) and navigation services (75%).
Conclusions
The required intensity and support given to meet patients’ medical and social needs is substantial and has significant variation. Meeting the needs of complex patients will require considerable investments in human capital, and a risk stratification system to help identify those most in need of services.



Similar content being viewed by others
Data Availability
Data is potentially available upon request from the author team.
References
Alderwick H, Gottlieb LM. Meanings and Misunderstandings: A Social Determinants of Health Lexicon for Health Care Systems. Milbank Q. 2019;97(2):407-419. https://doi.org/10.1111/1468-0009.12390.
National Academies of Sciences, Engineering, and Medicine. 2019. Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health. Washington, DC: The National Academies Press. https://doi.org/10.17226/25467.
Addressing Social Determinants to Improve Patient Care and Promote Health Equity: An American College of Physicians Position Paper. Daniel H, Bornstein SS, Kane GC for the Health and Public Policy Committee of the American College of Physicians. Ann Intern Med. 2018;168:577–578. https://doi.org/10.7326/M17-2441
Shah NR, Rogers AJ, Kanter MH. Health care that targets unmet social needs. NEJM Catalyst. 2016;13:2(2). https://doi.org/10.1056/CAT.16.0864.
Saulsberry L, Gunter KE, O'Neal Y, Tanumihardjo J, Gauthier R, Chin MH, Peek ME. “Everything in One Place”: Stakeholder Perceptions of Integrated Medical and Social Care for Diabetes Patients in Western Maryland. J Gen Intern Med. 2023;38(Suppl 1):25-32. https://doi.org/10.1007/s11606-022-07919-1.
Kannarkat JT, Hartle JE, Parekh N. Need for payer-provider partnerships in addressing social determinants of health. J Manag Care Spec Pharm. 2021;27(6):791-796. https://doi.org/10.18553/jmcp.2021.27.6.791.
Gunter KE, Peek ME, Tanumihardjo JP, Carbrey E, Crespo RD, Johnson TW, Rueda-Yamashita B, Schwartz EI, Sol C, Wilkinson CM, Wilson JO, Loehmer E, Chin MH. Population Health Innovations and Payment to Address Social Needs Among Patients and Communities With Diabetes. Milbank Q. 2021;99(4):928-973. https://doi.org/10.1111/1468-0009.12522.
Redlining: The history of Berkeley’s segregated neighborhoods. Berkeleyside Newspaper. 9/20/18. Available at https://www.berkeleyside.org/2018/09/20/redlining-the-history-of-berkeleys-segregated-neighborhoods. Accessed 4/12/22.
Oakland Equity Indicators. https://cao-94612.s3.amazonaws.com/documents/2018-Equity-Indicators-Full-Report.pdf. 2018. Accessed 29 March 2022.
Rebuilding Neighborhoods, Restoring Health: A Report on the Impact of Foreclosure on Public Health. Available at www.acphd.org/data-reports/reports-by-topic/social-andhealth-equity.aspx. 2010. Accessed 4/12/22.
Haan M, Kaplan GA, Camacho T. Poverty and health. Prospective evidence from the Alameda County Study. Am J Epidemiol. 1987;125:989–98.
Meyers B, Brown J, Cho S, Desautels A, Gaska K, Horsley K, et al. Life and death from unnatural causes: health and social inequity in Alameda County. Oakland (CA): Alameda County Public Health Department; 2008.
Healthy Alameda County. Available at https://www.healthyalamedacounty.org/indicators/index/view?indicatorId=8195&localeId=238. Accessed 12 April 2023.
Roots Community Health Center. Available at http://rootsclinic.org/history/. Accessed 12 April 2022.
Gunter KE, Tanumihardjo JP, O’Neal Y, Peek ME, Chin MH. Integrated interventions to bridge medical and social care for people living with diabetes. J Gen Intern Med. 2023;1-7. https://doi.org/10.1007/s11606-022-07926-2.
Morgan H. Conducting a qualitative document analysis. Qual Rep. 2022;27(1):64-77.
Thistoll T, Hooper V, Pauleen DJ. Acquiring and developing theoretical sensitivity through undertaking a grounded preliminary literature review. Quality & Quantity. 2016;50:619-36.
Riger ST, Sigurvinsdottir RA. Thematic analysis. in Handbook of methodological approaches to community-based research: qualitative, quantitative, and mixed methods. In: Jason LA, Glenwick DS, eds. Oxford Academic Press; 2015:33-41.
Shaw K, Killeen M, Sullivan E, Bowman P. Disparities in diabetes self-management education for uninsured and underinsured adults. The Diabetes Educ. 2011;37(6):813-819.
Butcher MK, Vanderwood KK, Hall TO, Gohdes D, Helgerson SD, Harwell TS. Capacity of Diabetes Education Programs to Provide Both Diabetes Self-management Education and to Implement Diabetes Prevention Services. J Public Health Manag Pract. 2011;17:242-247.
Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff. 2015;34(11):1830-9.
De Marchis EH, Torres JM, Benesch T, Fichtenberg C, Allen IE, Whitaker EM, Gottlieb LM. Interventions addressing food insecurity in health care settings: a systematic review. Annals Family Med. 2019;17(5):436-47.
Wood L, Wood NJ, Vallesi S, Stafford A, Davies A, et al. Hospital collaboration with a Housing First program to improve health outcomes for people experiencing homelessness. Housing, Care and Support. 2018;22(1):27-39.
Tinland A, Loubiere S, Boucekine M, Boyer L, Fond G, et al. Effectiveness of a housing support team intervention with a recovery-oriented approach on hospital and emergency department use by homeless people with severe mental illness: a randomised controlled trial. Epidemiol Psychiatr Sci. 2020;29:e169.
Fenelon A, Mayne P, Simon AE, Rossen LM, Helms V, et al. Housing Assistance Programs and Adult Health in the United States. Am J Public Health. 2017;107(4):571-578.
Moore E, Montojo N, Mauri N. Roots race & place: A history of racially exclusionary housing in the San Francisco Bay Area. Haas Institute: San Franscisco, CA. 2019.
Accountable Health Communities (AHC) Model Evaluation. Available at https://innovation.cms.gov/data-and-reports/2020/ahc-first-eval-rpt. 2020. Accessed 4/12/22.
Fraze T, Lewis VA, Rodriguez HP, Fisher ES. Housing, transportation, and food: how ACOs seek to improve population health by addressing nonmedical needs of patients. Health Aff. 2016;35(11):2109-15.
Funding
MP, YO, JT, KG, and RG acknowledge funding from the Merck Foundation’s initiative Bridging the Gap: Reducing Disparities in Diabetes Care. MP was supported in part by the Chicago Center for Diabetes Translation Research (NIDDK P30 DK092949).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Peek, M.E., Tanumihardjo, J.P., O’Neal, Y. et al. Intensity and Variation of Health Navigator Support: Addressing Medical and Social Needs of Diabetes Patients in East Oakland. J GEN INTERN MED (2024). https://doi.org/10.1007/s11606-023-08590-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11606-023-08590-w