Abstract
Background
Hospital admissions involving substance use disorders are increasing and represent an opportunity to engage patients in substance use treatment. Addiction medicine consultation services improve access to medications for opioid use disorder (MOUD) and patient outcomes. However, as hospitals continue to adopt addiction medicine consultation services it is important to identify where disparities may emerge in the process of care.
Objective
To describe addiction medicine consultation service use by race and ethnicity as well as substance to identify opportunities to reduce substance use treatment disparities.
Design
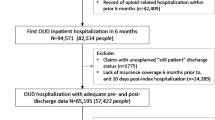
Retrospective cohort study using 2016–2021 Electronic Health Record data from a large Midwest safety-net hospital.
Participants
Hospitalized adults aged 18 or older, with one or more substance use disorders.
Main Measures
Consultation orders placed, patient seen by consult provider, and receipt of MOUD by self-reported race.
Key Results
Between 2016 and 2021, we identified 16,895 hospitalized patients with a substance use disorder. Consultation orders were placed for 6344 patients and 2789 were seen by the consult provider. Black patients were less likely (aOR = 0.58; 95% CI: 0.53–0.63) to have an addiction medicine consultation order placed and, among patients with a consultation order, were less likely (aOR = 0.74; 95% CI: 0.65–0.85) to be seen by the consult provider than White patients. Overall, Black patients with OUD were also less likely to receive MOUD in the hospital (aOR = 0.63; 95% CI: 0.50–0.79) compared to White patients. However, there were no differences in MOUD receipt among Black and White patients seen by the consult provider.
Conclusions
Using Electronic Health Record data, we identified racial and ethnic disparities at multiple points in the inpatient addiction medicine consultation process. Addressing these disparities may support more equitable access to MOUD and other substance use treatment in the hospital setting.
Similar content being viewed by others
References
Lindsay AR, Shearer RD, Bart G, Winkelman TNA. Trends in substance use disorder-related admissions at a safety-net hospital, 2008-2020. Journal of Addiction Medicine. Published online Under Review 2021.
Winkelman TNA, Admon LK, Jennings L, Shippee ND, Richardson CR, Bart G. Evaluation of Amphetamine-Related Hospitalizations and Associated Clinical Outcomes and Costs in the United States. JAMA Netw Open. 2018;1(6):e183758. https://doi.org/10.1001/jamanetworkopen.2018.3758
Fingar KR, Owens PL. Opioid-Related and Stimulant-Related Adult Inpatient Stays, 2012–2018: Statistical Brief #271. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality (US); 2021. Accessed June 14, 2021. http://www.ncbi.nlm.nih.gov/books/NBK568393/
Walley AY, Paasche-Orlow M, Lee EC, et al. Acute care hospital utilization among medical inpatients discharged with a substance use disorder diagnosis. J Addict Med. 2012;6(1):50-56. https://doi.org/10.1097/ADM.0b013e318231de51
Englander H, Jones A, Krawczyk N, et al. A Taxonomy of Hospital-Based Addiction Care Models: a Scoping Review and Key Informant Interviews. J GEN INTERN MED. Published online May 9, 2022. https://doi.org/10.1007/s11606-022-07618-x
Priest KC, McCarty D. The Role of the Hospital in the 21st Century Opioid Overdose Epidemic: The Addiction Medicine Consult Service. J Addict Med. 2019;13(2):104-112. https://doi.org/10.1097/ADM.0000000000000496
Englander H, Dobbertin K, Lind BK, et al. Inpatient Addiction Medicine Consultation and Post-Hospital Substance Use Disorder Treatment Engagement: a Propensity-Matched Analysis. J GEN INTERN MED. 2019;34(12):2796-2803. https://doi.org/10.1007/s11606-019-05251-9
Kleinman RA, Brothers TD, Morris NP. Retiring the “Against Medical Advice” Discharge. Ann Intern Med. 2022;175(12):1761-1762. https://doi.org/10.7326/M22-2964
Marks LR, Munigala S, Warren DK, Liang SY, Schwarz ES, Durkin MJ. Addiction Medicine Consultations Reduce Readmission Rates for Patients With Serious Infections From Opioid Use Disorder. Clin Infect Dis. 2019;68(11):1935-1937. https://doi.org/10.1093/cid/ciy924
McNeely J, Troxel AB, Kunins HV, et al. Study protocol for a pragmatic trial of the Consult for Addiction Treatment and Care in Hospitals (CATCH) model for engaging patients in opioid use disorder treatment. Addiction Science & Clinical Practice. 2019;14(1):5. https://doi.org/10.1186/s13722-019-0135-7
Ober AJ, Murray-Krezan C, Page K, et al. The Substance Use Treatment and Recovery Team (START) study: protocol for a multi-site randomized controlled trial evaluating an intervention to improve initiation of medication and linkage to post-discharge care for hospitalized patients with opioid use disorder. Addiction Science & Clinical Practice. 2022;17(1):39. https://doi.org/10.1186/s13722-022-00320-7
Calcaterra SL, McBeth L, Keniston AM, Burden M. The Development and Implementation of a Hospitalist-Directed Addiction Medicine Consultation Service to Address a Treatment Gap. J GEN INTERN MED. 2022;37(5):1065-1072. https://doi.org/10.1007/s11606-021-06849-8
Wakeman SE, Kane M, Powell E, et al. A hospital-wide initiative to redesign substance use disorder care: Impact on pharmacotherapy initiation. Substance Abuse. 2021;42(4):767-774. https://doi.org/10.1080/08897077.2020.1846664
Nordeck CD, Welsh C, Schwartz RP, et al. Rehospitalization and substance use disorder (SUD) treatment entry among patients seen by a hospital SUD consultation-liaison service. Drug and Alcohol Dependence. 2018;186:23-28. https://doi.org/10.1016/j.drugalcdep.2017.12.043
Martin M, Snyder HR, Coffa D, et al. Time to ACT: launching an Addiction Care Team (ACT) in an urban safety-net health system. BMJ Open Qual. 2021;10(1):e001111. https://doi.org/10.1136/bmjoq-2020-001111
D’Amico MJ, Walley AY, Cheng DM, et al. Which patients receive an Addiction Consult? A preliminary analysis of the INREACH (INpatient REadmission post-Addiction Consult Help) Study. J Subst Abuse Treat. 2019;106:35-42. https://doi.org/10.1016/j.jsat.2019.08.013
Thompson HM, Hill K, Jadhav R, Webb TA, Pollack M, Karnik N. The Substance Use Intervention Team: A Preliminary Analysis of a Population-level Strategy to Address the Opioid Crisis at an Academic Health Center. J Addict Med. 2019;13(6):460-463. https://doi.org/10.1097/ADM.0000000000000520
Vickery KD, Shippee ND, Bodurtha P, et al. Identifying homeless medicaid enrollees using enrollment addresses. Health Services Research. 2018;53(3):1992-2004. https://doi.org/10.1111/1475-6773.12738
Owens PL, Fingar KR, McDermott KW, Muhuri PK, Heslin KC. Inpatient Stays Involving Mental and Substance Use Disorders, 2016.; 2019. Accessed February 14, 2021. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb249-Mental-Substance-Use-Disorder-Hospital-Stays-2016.jsp
Shearer RD, Shippee ND, Winkelman TNA. Characterizing trends in methamphetamine-related health care use when there is no ICD code for “methamphetamine use disorder.” Journal of Substance Abuse Treatment. 2021;127:108369. https://doi.org/10.1016/j.jsat.2021.108369
Andraka-Christou B. Addressing Racial And Ethnic Disparities In The Use Of Medications For Opioid Use Disorder. Health Affairs. 2021;40(6):920-927.
Hansen H, Roberts SK. Two tiers of biomedicalization: METHADONE buprenorphine and the racial politics of addiction treatment. In: Netherland J, ed. Critical Perspectives on Addiction. Advances in Medical Sociology. ; 2012:79-102. https://doi.org/10.1108/S1057-6290(2012)0000014008
Han B, Cotto J, Etz K, Einstein EB, Compton WM, Volkow ND. Methamphetamine Overdose Deaths in the US by Sex and Race and Ethnicity. JAMA Psychiatry. Published online January 20, 2021. https://doi.org/10.1001/jamapsychiatry.2020.4321
Kariisa M, Seth P, Scholl L, Wilson N, Davis NL. Drug overdose deaths involving cocaine and psychostimulants with abuse potential among racial and ethnic groups – United States, 2004–2019. Drug and Alcohol Dependence. 2021;227:109001. https://doi.org/10.1016/j.drugalcdep.2021.109001
Ciccarone D, Shoptaw S. Understanding Stimulant Use and Use Disorders in a New Era. Medical Clinics of North America. 2022;106(1):81-97. https://doi.org/10.1016/j.mcna.2021.08.010
DeLaquil M. Differences in Rates of Drug Overdose Deaths by Race. Minnesota Department of Health; 2020:17.
Tierney HR, Rowe CL, Coffa DA, Sarnaik S, Coffin PO, Snyder HR. Inpatient Opioid Use Disorder Treatment by Generalists is Associated With Linkage to Opioid Treatment Programs After Discharge. J Addict Med. 2022;16(2):169-176. https://doi.org/10.1097/ADM.0000000000000851
Jo Y, Nosal R, Vittori A, et al. Effect of initiation of medications for opioid use disorder on hospitalization outcomes for endocarditis and osteomyelitis in a large private hospital system in the United States, 2014–18. Addiction. 2021;116(8):2127-2134. https://doi.org/10.1111/add.15393
Priest KC, Lovejoy TI, Englander H, Shull S, McCarty D. Opioid Agonist Therapy During Hospitalization Within the Veterans Health Administration: a Pragmatic Retrospective Cohort Analysis. J Gen Intern Med. 2020;35(8):2365-2374. https://doi.org/10.1007/s11606-020-05815-0
Hall OT, Jordan A, Teater J, et al. Experiences of racial discrimination in the medical setting and associations with medical mistrust and expectations of care among black patients seeking addiction treatment. Journal of Substance Abuse Treatment. 2022;133:108551. https://doi.org/10.1016/j.jsat.2021.108551
Bassuk EL, Hanson J, Greene RN, Richard M, Laudet A. Peer-Delivered Recovery Support Services for Addictions in the United States: A Systematic Review. Journal of Substance Abuse Treatment. 2016;63:1-9. https://doi.org/10.1016/j.jsat.2016.01.003
Englander H, Gregg J, Gullickson J, et al. Recommendations for integrating peer mentors in hospital-based addiction care. Substance Abuse. 2020;41(4):419-424. https://doi.org/10.1080/08897077.2019.1635968
Collins D, Alla J, Nicolaidis C, et al. “If It Wasn’t for Him, I Wouldn’t Have Talked to Them”: Qualitative Study of Addiction Peer Mentorship in the Hospital. J GEN INTERN MED. Published online December 12, 2019. https://doi.org/10.1007/s11606-019-05311-0
Paluck EL, Porat R, Clark CS, Green DP. Prejudice Reduction: Progress and Challenges. Annual Review of Psychology. 2021;72(1):533-560. https://doi.org/10.1146/annurev-psych-071620-030619
Priest KC, King CA, Englander H, Lovejoy TI, McCarty D. Differences in the delivery of medications for opioid use disorder during hospitalization by racial categories: A retrospective cohort analysis. Substance Abuse. 2022;43(1):1251-1259. https://doi.org/10.1080/08897077.2022.2074601
Howell BA, Abel EA, Park D, Edmond SN, Leisch LJ, Becker WC. Validity of Incident Opioid Use Disorder (OUD) Diagnoses in Administrative Data: a Chart Verification Study. J GEN INTERN MED. 2021;36(5):1264-1270. https://doi.org/10.1007/s11606-020-06339-3
Lagisetty P, Garpestad C, Larkin A, et al. Identifying individuals with opioid use disorder: Validity of International Classification of Diseases diagnostic codes for opioid use, dependence and abuse. Drug Alcohol Depend. 2021;221:108583. https://doi.org/10.1016/j.drugalcdep.2021.108583
Acknowledgements:
This research was supported by the National Institutes of Health’s National Center for Advancing Translational Sciences, grant UL1TR002494. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health’s National Center for Advancing Translational Sciences. Riley Shearer was supported by NIH MSTP grant T32 GM008244.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 20 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lindsay, A.R., Winkelman, T.N.A., Bart, G. et al. Hospital Addiction Medicine Consultation Service Orders and Outcomes by Patient Race and Ethnicity in an Urban, Safety-Net Hospital. J GEN INTERN MED 39, 168–175 (2024). https://doi.org/10.1007/s11606-023-08356-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08356-4