Abstract
Background
The Prime Time Sister Circles®, a randomized controlled trial (PTSC-RCT), assessed the impact of a community-based peer support program on hypertension management among African American women 40–75 years of age. While the PTSC-RCT was designed to evaluate changes in blood pressure control, subsequent sub-analyses revealed a high proportion of self-reported depressive symptoms in our sample. Accordingly, we conducted an ancillary investigation of the PTSC intervention on depression to ascertain its impact on reduced depressive symptoms in the study population.
Method
Depressive symptoms were measured using an adapted version of the Center for Epidemiologic Studies Depression Scale Revised (CES-D-10). We used unadjusted and adjusted fixed effect models. Data for this study came from the PTSC-RCT. We collected data between 2017 and 2018 in Washington, DC. We used a balanced analytical sample of 172 African American, English-speaking women between 40 to 75 years old with uncontrolled hypertension.
Intervention
The intervention group participated in a 2-h, peer-based support group once a week for 13 weeks. A trained PTSC facilitator facilitated sessions with experts who delivered content on various topics, including psychosocial wellness (e.g., stress, depressive symptoms, anxiety management, and self-esteem), physical health (e.g., hypertension, inflammation, and heart disease), physical activity, and healthy nutrition.
Results
Results from the fixed-effects models indicated that participants in the PTSC program exhibited a greater reduction in CES-D-10 score at three months (Coeff: -1.99, 95% CI: -3.49, -0.49) and at 15 months (Coeff: -2.38, 95% CI: -3.94, -0.83), as compared to those in the control group.
Conclusions
Evidence suggests that the Prime Time Sister Circles® intervention reduced depressive symptoms among African American women with low socioeconomic status and hypertension.
Trial Registration
NCT04371614.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Approximately 18.5% of adults aged 18 and over have reported experiencing any symptoms of depression in 2019,1 with higher prevalence observed among low-income African American (AA) women.2,3,4,5,6 Several factors have been proposed as contributors to this phenomenon, including residence in environments with higher poverty,7 lower access to healthy foods,8 lower access to mental health providers due to lack of health insurance,9,10,11 higher prevalence of comorbidities,12,13,14 and a lower rate of social supports.15 The promotion and adherence to cultural beliefs such as the “strong Black woman” trope16,17,18 may limit some AA women’s emotional capacity to employ healthy coping strategies that are supportive of their mental health, including seeking care for psychological issues or availing themselves of support from members of their social networks.19,20,21 AA women are more likely than women of other races to face a unique constellation of stressors that can create and sustain depressive symptoms; these stressors include racism, sexism, poverty, and discrimination. AA women's depressive symptoms often differ from White women's, including increased appetite and weight, irritability and persistent physical symptoms.19 The COVID-19 pandemic and its impact on the mental health of African Americans at large confers urgency to this pressing issue.20
Older AA women have higher rates of depressive symptoms than their White peers.21 The association between depressive symptomology and the occurrence of other health conditions is well established: Germain reports that AA women with high depressive symptoms have higher prevalence of functional impairment.22 Other studies have reported the co-occurrence of depression and poor cardiovascular health among AA women. Burroughs et al. (2019) reported that AA women were more likely to have high Cumulative Psychosocial Stress (CPS) scores (172.5 ± 54.9) and experience low ideal cardiovascular health (ICH).23
The association between depression and many chronic diseases, including but not limited to hypertension,24 obesity,25 cardio-metabolic disorder syndrome,26,27 and cardiovascular diseases (CVD),28 can result in higher mortality rates and lower quality of life in AA women, especially those with lower incomes.29 Research has shown that AA women with low-income status and hypertension suffer from depressive symptoms, which implies that this is a particularly vulnerable group.14 Yet, despite indication suggesting a strong link between high blood pressure and depression,30,31 AA women whose health care entails ongoing monitoring of their blood pressure may not be receiving adequate care for their depression;32 indeed, only a third of AA adults experiencing mental illness received services in 2019.33
While community-based interventions that address the unique behavioral, cultural, emotional, and social needs of low-income AA may be difficult to access due to comorbidities, scheduling, and various social risk factors,33 they are a necessary strategy to combat intransigent disparities observed in this population. The Oh Happy Day Class is an example of a culturally adapted intervention for African American adults, which reduced depressive symptoms in participants by 6.6 points from baseline to 3-month follow-up.34 The Prime Time Sister Circles® (PTSC) Program is another promising intervention. The PTSC Program incorporates peer support and didactic training that focuses on psychosocial health and well-being to: (1) address the sociocultural risk factors that mid- to late-life AA women with uncontrolled hypertension experience and (2) promote the adoption of primary and secondary prevention strategies to control their blood pressure and engagement in strategies geared toward psychosocial health.33
We leveraged a randomized controlled trial evaluating the impact of the PTSC intervention on hypertension control to explore its effect on reducing depressive symptoms among mid-life, low-income AA women with uncontrolled hypertension. This was achieved through a secondary analysis of data collected between 2017 and 2018 as a part of this trial. We report on the impact of the PTSC intervention on participants’ depressive symptoms.
Methods
Trial design
This study is a secondary analysis of data collected as part of a larger randomized clinical trial that evaluates the effectiveness of the Prime Time Sister Circle® (PTSC) on a range of health, healthcare utilization, and behavioral outcomes. 33 Details of the PTSC-RCT are summarized elsewhere.27 In short, the PTSC-RCT’s primary outcome is hypertension control, and it was powered to assess the impact of exposure to the PTSC intervention on hypertension. The study’s secondary outcomes include health knowledge, self-efficacy, behaviors, and psychosocial health. For this analysis, we used data from the PTSC-RCT to study the impact of the PTSC intervention on depressive symptoms reported by our study population, low-income AA women with uncontrolled hypertension receiving care in a Federally Qualified Health Center (FQHC). We hypothesized that PTSC intervention would reduce the CESD-10 score in women who participated in the 13-week training session.
Participants
Data for this study came from the PTSC-RCT. The PTSC was a community-based intervention program targeting English-speaking AA women who were 40 to 75 years of age, had been diagnosed with uncontrolled hypertension (systolic blood pressure ≥ 140 mm Hg and diastolic blood pressure ≥ 90), resided in Washington, D.C., and were patients at Unity Health. Study participants were randomly assigned to the PTSC intervention or the control group, and both arms maintained their care at Unity. We collected data from 2017 to 2018.
Interventions
The main goals of the PTSC intervention were to help AA midlife women learn how to manage, lower, and control their high blood pressure; expand their repertoire of stress management techniques; increase their physical activity; and improve their nutrition. Study participants were assigned to cohorts of Sister Circles that met once a week, over a 13-week period, for 2 h at a time. The PTSC intervention curriculum included culturally competent modules designed to help AA women manage their stress, an underlying contributor to depression. To that end, two sessions were devoted to stress and depressive symptom management. They were conducted by midlife AA women with extensive mental health expertise (i.e., psychologists or licensed clinical social workers). Each participant was taught general stress-management techniques such as deep breathing, communication skills, and time management strategies. They also developed a stress-management plan. Sister Circle sessions were held in meeting rooms provided by three churches in Washington, D.C.
Measures
Outcomes
To identify participants with depressive symptoms, we employed the Center for Epidemiologic Studies Depression Scale Revised (CES-D-10), a widely used self-reported measure of depression symptoms. The CES-D-10 comprises ten items (8 positively worded and two negatively worded) and has exhibited strong internal consistency (Cronbach’s α = 0.86) and test–retest reliability (ICC = 0.85) among the general population.35,36 Further, the CES-D-10 is a reliable tool for measuring depression, with a value of the reliability coefficient of 0.7 (Cronbach’s alpha) and composite reliability of 0.72; 37 as such, the scale is an excellent measure to identify individuals at risk for clinical depression.38 Each item uses a 4-point Likert scale, with 0 indicating rarely or none of the time (less than one day per week) and 3 indicating all of the time (5‐7 days per week). Following the CES-D-10 guidelines, we reverse coded items 5 and 8 (two items that were negatively worded) and then calculated the total score by summing up scores of the ten items, resulting in a maximum scale score of 30 and a minimum scale score of 0.37
Control variables
In all models, we controlled for sociodemographic variables at baseline, including age and marital status, education, health insurance status, and health behavior status (smoking or alcohol consumption). We also controlled for several chronic conditions at baseline through a composite measure showing whether a participant had reported diabetes, high blood cholesterol, heart disease, cancer, stroke, and obesity).
Sample size
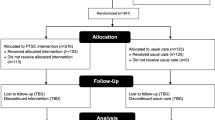
We recruited 341 AA women receiving care at a Health Care Center (‘facility’ in this text) in Washington, D.C., in 2017 and 2018. Eligible participants were English-speaking women between 40 to 75 years of age who self-identified as AA, received their primary care at a Unity practice, and had been diagnosed with uncontrolled hypertension (systolic blood pressure ≥ 140 mm Hg or diastolic blood pressure ≥ 90).2,25 Participants were randomly assigned to receive the PTSC intervention (n = 216) or to the control group and proceeded with their standard clinical care at Unity (n = 135). We designated participants randomized to the intervention group, who did not receive it as intended, as the Intent-to-Treat (ITT) group (see CONSORT diagram for more details, Fig. 1). We collected data at baseline, 3 months, and 15 months. Among the 341 participants who provided baseline data, 240 provided data at the 3-month mark, and 217 at the 15-months mark. Notably, nearly 30% of the participants dropped out of the study after randomization. Sub-analyses indicated that social risk factors (e.g., transportation) and personal health concerns were primary drivers for suboptimal participation. For this analysis, we excluded 25 participants with missing responses on two or more items on the CES-D-10. We constrained the analytic sample to those who furnished data during all 3 data collection time points. This reduced the sample to 172 participants (516 observations).
Randomization
Details of our randomization strategy have been captured elsewhere.33 In summation, recruitment procedures in Washington, DC commenced in 2017 and ended in 2018. The facility generated a list of patients across their practices who met the study's eligibility criteria and shared their names and addresses with the study team. Potential candidate participants received a letter highlighting information about the study, incentives for participation, contact information for study team members, and the dates and locations of the recruitment sessions. Those who were interested were invited to a recruitment meeting to learn about the PTSC-RCT, including specifics about the PTSC. During this meeting, participants were randomly assigned to the PTSC intervention or control groups. Upon providing written consent, study participants completed a baseline survey that was administered verbally by the study team. Data were collected immediately after the intervention (3 months), and one-year post-intervention (15 months).33 The CES-D-10 was administered at baseline, three months, and 15 months.
Statistical Analysis
We conducted descriptive analyses to compare those in the control group (those receiving usual care), PTSC group (intervention), and Intent-to-Treat (ITT, assigned to PTSC but did not participate in the intervention sessions) groups. Using unequal variance t-tests and Chi-Squared tests, we examined potential differences between control, PTSC, and ITT for control variables. Then, we ran a fixed-effect model analysis using a balanced panel, which allowed us to measure the impact of the PTSC program on the same individual 3 months and 15 months after the intervention. We ran sets of unadjusted and adjusted models. For the unadjusted model, we controlled only for the group (PTSC), time (3 months and 15 months), and interaction (being in PTSC/ITT groups at 3 or 15 months as a fixed effect measure to measure the impact of PTSC program at 3 and 15 months). For the adjusted models, we controlled for age, marital status, education, income, health insurance status, smoking status, drinking status, and the number of chronic conditions.
There were some missing values for the control variables, including age, marital status, education, income, health insurance coverage, smoking, and drinking behaviors; we cite the percentage of missing values for these variables in Table 1. To address the issue of missing data, we used the multiple imputations (MI) technique in Stata to fill in the missing values, assuming that data was missing at random. All statistical procedures were conducted using Stata, version 15.
For the Intent-to-Treat analysis, we used balanced panel data for women who participated in all 3 rounds of data collection. We included PTSC and ITT (participants initially assigned to PTSC regardless of whether they received the PTSC treatment) and control. The analytical sample of this analysis was 172 participants (516 observations). We also conducted a Per-Protocol analysis. To do so, we repeated the ITT analysis by excluding those assigned to the intervention group who did not receive the treatment (Intent-to-Treat), which reduced the sample to 140 participants (420 observations). This study was approved by the Institutional Review Boards (IRBs) of the Johns Hopkins Bloomberg School of Public Health (JHBSPH) and the American Institutes for Research (JHBSPH IRB No. 00007121).
Results
The distribution of characteristics among the PTSC-RCT participants by intervention groups is shown in Table 1. On average, women who participated in the PTSC intervention were 59 years old. They were also more likely to be single without a partner (53.5%), have a high school diploma (38.4%), and have a household income of less than $20,000 a year (75.6%). Our findings showed that more than 42.4% of the PTSC group were current smokers, 47.6% reported some level of alcohol consumption and had been diagnosed with at least 2.3 chronic conditions. In addition, almost all had health insurance coverage (98.8%). There were no significant differences in sociodemographic variables between PTSC, ITT, and control groups except for drinking and smoking. (See Table 1.)
Figure 2 compares CES-D-10 scale scores between control, PTSC, and ITT groups across baseline, three months, and 15 months surveys. In the PTSC group, the CES-D-10 score significantly declined by 2.6 points, from 11.54 points (95% CI: 10.36–12.73) at baseline to 8.94 points (95% CI: 7.77–10.11) at 3 months (22.5% reduction, p = 0.002). It also reduced by 2.7 points from baseline to 8.87 (95% CI: 7.50–10.24) at the 15 months mark (23.1% reduction, p = 0.004). In the ITT group, the CES-D-10 score reduced slightly from baseline (11.60 points; CI: 7.71–15.49) to 3 months (10.91 points; CI: 8.62–13.19), but this 5.9% reduction was not statistically significant (p = 0.737). Self-reported depressive symptoms in the ITT group rose slightly from baseline to 15 months (13.4% increase, p = 0.351), but this was insignificant. Finally, in the control group, the CES-D-10 score did not change substantially from 10.93 points at baseline (95% CI: 9.49–12.37) to 10.66 points at three months (2.5% reduction, p = 0.783), and was not significantly reduced at 15 months (9.79 points, 10.4% reduction, p = 0.247).
Table 2 displays the results of the fixed effects models ascertaining differences between the control and PTSC in the CES-D-10 scores over time. The parameter of interest in these models is the interaction between the group membership (PTSC vs. control) and the measurement timing (baseline vs. three months or baseline vs. 15 months). Panel A columns 1 and 2 show that, compared to women in the control group, women who participated in the 13-week intervention program had a significantly greater reduction in their CES-D-10 scores from baseline to 3-month follow up (Coeff.: -1.99, 95% CI: -3.57, -0.41) in the unadjusted model. Results remained similar in the adjusted model (Coeff.: -1.99, 95% CI: -3.49, -0.49), and we found similar results at 15 months. Those who participated in the PTSC intervention had a significantly greater reduction in the CES-D-10 score from baseline to 15 months follow up (Coeff.: -2.42, 95% CI: -4.04, -0.80) in the unadjusted model and (Coeff.: -2.68, 95% CI: -4.51, -0.84) in the adjusted model (See Columns 3 and 4). Table 2 also contains the results of the regression models used to conduct per-protocol analyses in Panel B. The results of the adjusted model indicate that women who participated in the 13-week PTSC intervention had significantly reduced CES-D-10 scores from baseline to 3-month follow-up (-2.14; 95% CI: -3.98, -0.30) and baseline to 15 months follow up (-2.22; 95% CI: -3.98, -0.38).
Discussion
In this study, we used the CES-D-R (CES-D-10) scale to measure self-reported depressive symptoms among low-income AA women between 40 to 75 years old with uncontrolled hypertension who participated in PTSC program in Washington, DC between 2017–2018. Our findings showed that the PTSC intervention effectively reduced women's depressive symptoms at 3 months and 15 months after the intervention. To our knowledge, there are very few studies to which we can compare our results. However, the decrease in depressive symptomology is similar to other group-based interventions. The reductions we observed may be due to aspects of the Sister Circles themselves, insofar as PTSC provided an environment that helped participants gain stress management skills with their peers. Being in a group of women with similar chronic diseases and mental health issues helped participants discuss their own situations, which could have lowered their stress and ameliorated other aspects of their psychosocial health associated with depression.39,40,41
Findings from our previous work showed that low-income AA women with hypertension have unmet depression care needs. Our cross-sectional analysis revealed that a majority of the women in the PTSC-RCT had experienced some level of depression, measured by CES-D-10 scores greater than 10.14 Based on the results of our current analysis, about 60% of participants with depression symptoms reported receiving some form of mental health services within the past six months, and about the same amount (58%) reported seeing a mental health professional. We expect these mental health needs to have increased as the COVID-19 pandemic persists and will continue after the SARS-COV-2 virus becomes endemic.42 Since the pandemic disproportionately impacts low-income and AA communities, we anticipate that depression care needs will remain high among low-income AA women. This affirms the need for public health and healthcare policymakers, practitioners, and advocates to implement policies and programs that address the unmet depression care needs of this population. Given the high depressive symptoms among low-income AA women with hypertension, we recommend promoting awareness and strategies to diagnose people with depression as early as possible. One approach could include incorporating an assessment of depression symptoms within routine bi-annual screening for low-income AA women with hypertension. Our study also reinforces the critical importance of developing, implementing, and evaluating community-based interventions that are contextualized to low-income AA women’s needs. We found strong evidence to suggest that a culturally responsive intervention, such as the PTSC Program, can reduce depressive symptoms among low-income AA women with hypertension receiving care at a facility.
There is an overall lack of access to treatment for mental illness in Americans, particularly among Black/African Americans.43 Several barriers have been enumerated by the American Psychiatric Association (APA) and other bodies and include, but are not limited to: (1) lack of culturally adopted mental health treatments, (2) lack of access to high-quality care, (3) stigma and negative attitudes and beliefs ascribed to mental health conditions, (4) lower rates of mental health providers with diverse racial backgrounds, and (5) inability to pay for treatment because of lack of income or a lower rate of health insurance.43,44,45 The PTSC partially addresses these barriers by offering a culturally tailored, community-based intervention that uses a peer group format to combat stigma and negative attitudes and trained lay facilitators to extend and support mental health providers. Public and private insurance should consider providing reimbursement to support interventions such as the PTSC.
This study has several important limitations. First, the study population was AA women ages 40–75 with low-income and uncontrolled hypertension who received primary care from a facility in Washington, DC. Our findings may not be generalizable to higher-income AA women or low-income AA women who cannot maintain consistent access to care. Second, the primary outcome of this RCT was hypertension, and the CES-D-10 scale (which is a screening tool) was collected as the secondary outcome to measure potential changes in depressive symptoms. While we powered the PTSC-RCT to detect changes in hypertension outcomes, we did not conduct power analyses to discern the impact of the intervention on depressive symptomology. This limits our ability to conclusively state that the PTSC intervention was solely responsible for reducing self-reported depressive symptoms among our study population. Third, we assumed the randomness of missing data with respect to our analyses; yet, given the sociodemographic profile of our study population, it is likely that missingness was linked to adverse social determinants of health that precluded full participation in the intervention and data collection strategies. Finally, we did not include other measures of psychosocial distress in the analyses, partially due to the unavailability of data.
Despite these limitations, this study has several strengths. The PTSC-RCT measured depressive symptoms in a largely homogeneous population with respect to race/ethnicity, socioeconomic and demographic characteristics, health status, and geography. Further, because participants in this study had received their care at a facility, it is reasonable to consider that undiagnosed depression was not due to a lack of access to care. Indeed, the association between depressive symptoms and hypertension underscores the need for integrated models of care that facilitate access to mental health support for women with high blood pressure. It also reinforces the importance of strategies to monitor both the quality of mental health services provided and the extent of the uptake of such services to ensure receipt of adequate treatment.46 Since the CES-D-10 is widely used to screen depressive symptoms, our study results are comparable to national survey results. Finally, there is a strong need to develop, implement, evaluate, and disseminate promising community-based interventions that reduce depression symptoms among AA women. This study builds our knowledge of effective interventions and can help equip lower-income Black women with much-needed tools to recognize symptoms of depression and seek help.47
Conclusion
The prevalence of depression is high among women with chronic diseases, especially hypertension, specifically African American women with lower socioeconomic status. Addressing the depression care needs of these women is a multidimensional mission that requires cooperation among mental health specialists, primary care providers, community-based programs, researchers, and public health officials. Interventions should consider addressing social determinants of health, including individual, sociocultural, environmental, and historical factors that impact the mental health of low-income African American women. There is a need for programs such as PTSC that empower women and help them better manage their emotional and physical health issues and depressive symptoms. Our findings show that free, culturally competent, community-based intervention programs such as the PTSC can effectively reduce depressive symptoms.
References
Villarroel. MA, Terlizzi. EP. Symptoms of Depression Among Adults: United States, 2019. NCHS Data Brief. No. 379. September 2020. Centers for Disease Control and Prevention National Center for Health Statistics. 2020. Available at: https://www.cdc.gov/nchs/data/databriefs/db379-H.pdf. Accessed May 25, 2023.
Braithwaite RL, Taylor SE, Treadwell HM. Health issues in the Black community. John Wiley & Sons; 2009.
Carrington CH. Clinical depression in African American women: Diagnoses, treatment, and research. Journal of clinical psychology. 2006;62(7):779-791.
Brody DJ PL, Hughes J. Prevalence of depression among adults aged 20 and over: United States, 2013–2016. NCHS Data Brief, no 303. Hyattsville, MD: National Center for Health Statistics. 2018. Available at: https://www.cdc.gov/nchs/data/databriefs/db303.pdf. Accessed May 25, 2023.
Lara-Cinisomo S, Akinbode TD, Wood J. A systematic review of somatic symptoms in women with depression or depressive symptoms: do race or ethnicity matter? Journal of women's health. 2020;29(10):1273-1282.
Michaels E, Thomas M, Reeves A, et al. Coding the Everyday Discrimination Scale: implications for exposure assessment and associations with hypertension and depression among a cross section of mid-life African American women. J Epidemiol Community Health. 2019;73(6):577-584.
Fins A. National snapshot: Poverty among women & families, 2020. National Women’s Law Center Retrieved September. 2020;23:2021.
Groh CJ. Poverty, mental health, and women: Implications for psychiatric nurses in primary care settings. Journal of the American Psychiatric Nurses Association. 2007;13(5):267-274.
Borah M, Knabe A, Pahlke K. Parental time restrictions and the cost of children: insights from a survey among mothers. The Journal of Economic Inequality. 2021;19(1):73-95.
Kaiser Family Foundation (KFF). Mental Health and Substance Use State Fact Sheets. 2021. Available at: https://www.kff.org/statedata/mental‐health‐and‐substance‐use‐state‐fact‐sheets/. Accessed May 25, 2023.
McGuire TG, Miranda J. New evidence regarding racial and ethnic disparities in mental health: Policy implications. Health Affairs. 2008;27(2):393-403.
Bazargan M, Hamm-Baugh VP. The relationship between chronic illness and depression in a community of urban black elderly persons. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 1995;50(2):S119-S127.
Baker F, Okwumabua J, Philipose V, Wong S. Screening African-American elderly for the presence of depressive symptoms: a preliminary investigation. Journal of geriatric psychiatry and neurology. 1996;9(3):127-132.
Gabriel A, Zare H, Jones W, et al. Evaluating depressive symptoms among low-socioeconomic-status African American women aged 40 to 75 years with uncontrolled hypertension: a secondary analysis of a randomized clinical trial. JAMA psychiatry. 2021;78(4):426-432.
Germain CM. Ethnicity, Depression, and functional outcomes in oder women. Innovation in Aging. 2019;3(Suppl 1):S605.
Thomas Z, Banks J, Eaton AA, Ward LM. 25 years of psychology research on the “strong black woman”. Social and Personality Psychology Compass. 2022;16(9):e12705.
Giannino SS, China CR. A critical look at certainty adverbs and the essentializing discourse of Black female identity in the reality television show, girlfriend Intervention. Howard Journal of Communications. 2018;29(1):18-32.
Abrams JA, Hill A, Maxwell M. Underneath the mask of the strong Black woman schema: Disentangling influences of strength and self-silencing on depressive symptoms among US Black women. Sex roles. 2019;80:517-526.
Johnson LA. Variations in Social Support and Mental Health Among Black Women by Socioeconomic Status. Sociology Theses, Dissertations, & Student Research. 2010. Available at: https://digitalcommons.unl.edu/cgi/viewcontent.cgi?article=1008&context=sociologydiss. Accessed May 25, 2023.
Snowden LR, Snowden JM. Coronavirus trauma and African Americans’ mental health: Seizing opportunities for transformational change. International journal of environmental research and public health. 2021;18(7):3568.
Spence NJ, Adkins DE, Dupre ME. Racial differences in depression trajectories among older women: Socioeconomic, family, and health influences. Journal of health and social behavior. 2011;52(4):444-459.
Germain CM. Ethnicity, depression, and functional outcomes in older women. Innovation in Aging. 2019;3(Suppl 1):S605.
Burroughs Pena MS, Mbassa RS, Slopen NB, Williams DR, Buring JE, Albert MA. Cumulative psychosocial stress and ideal cardiovascular health in older women: data by race/ethnicity. Circulation. 2019;139(17):2012-2021.
Crosswell AD, Lockwood KG. Best practices for stress measurement: How to measure psychological stress in health research. Health psychology open. 2020;7(2):2055102920933072.
Jones HJ, Minarik PA, Gilliss CL, Lee KA. Depressive symptoms associated with physical health problems in midlife women: a longitudinal study. Journal of affective disorders. 2020;263:301-309.
Chirinos DA, Murdock KW, LeRoy AS, Fagundes C. Depressive symptom profiles, cardio-metabolic risk and inflammation: Results from the MIDUS study. Psychoneuroendocrinology. 2017;82:17-25.
Cooper DC, Trivedi RB, Nelson KM, et al. Sex differences in associations of depressive symptoms with cardiovascular risk factors and metabolic syndrome among African Americans. Cardiovascular psychiatry and neurology. 2013;2013
Moise N, Khodneva Y, Richman J, Shimbo D, Kronish I, Safford MM. Elucidating the association between depressive symptoms, coronary heart disease, and stroke in black and white adults: the REasons for geographic and racial differences in stroke (REGARDS) study. Journal of the American Heart Association. 2016;5(8):e003767.
Axon RN, Zhao Y, Egede LE. Association of depressive symptoms with all-cause and ischemic heart disease mortality in adults with self-reported hypertension. American journal of hypertension. 2010;23(1):30-37.
Landsbergis PA, Dobson M, Koutsouras G, Schnall P. Job strain and ambulatory blood pressure: a meta-analysis and systematic review. American journal of public health. 2013;103(3):e61-e71.
Madsen IE, Nyberg ST, Hanson LM, et al. Job strain as a risk factor for clinical depression: systematic review and meta-analysis with additional individual participant data. Psychological medicine. 2017;47(8):1342-1356.
Shim RS, Baltrus P, Bradford LD, Holden KB, Fresh E, Fuller Sr LE. Characterizing depression and comorbid medical conditions in African American women in a primary care setting. Journal of the national medical association. 2013;105(2):183-191.
Ibe CA, Haywood DR, Creighton C, et al. Study protocol of a randomized controlled trial evaluating the Prime Time Sister Circles (PTSC) program's impact on hypertension among midlife African American women. BMC public health. 2021;21(1):1-10.
Ward EC, Brown RL. A culturally adapted depression intervention for African American adults experiencing depression: Oh Happy Day. American Journal of Orthopsychiatry. 2015;85(1):11.
Eaton WW, Smith C, Ybarra M, Muntaner C, Tien A. Center for Epidemiologic Studies Depression Scale: review and revision (CESD and CESD-R). 2004;
Miller W, Anton H, Townson A. Measurement properties of the CESD scale among individuals with spinal cord injury. Spinal cord. 2008;46(4):287-292.
Mohebbi M, Nguyen V, McNeil JJ, et al. Psychometric properties of a short form of the Center for Epidemiologic Studies Depression (CES-D-10) scale for screening depressive symptoms in healthy community dwelling older adults. General hospital psychiatry. 2018;51:118-125.
Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and aging. 1997;12(2):277.
Bressington D, Mui J, Yu C, et al. Feasibility of a group-based laughter yoga intervention as an adjunctive treatment for residual symptoms of depression, anxiety and stress in people with depression. Journal of affective disorders. 2019;248:42-51.
Sun C, Tikellis G, Klein R, Steffens DC, Marino Larsen EK, Wong TY. Depressive symptoms and age-related macular degeneration in older people: the cardiovascular health study. Ophthalmic epidemiology. 2007;14(3):127-133.
Bell TP. Meditative practice cultivates mindfulness and reduces anxiety, depression, blood pressure, and heart rate in a diverse sample. Journal of Cognitive Psychotherapy. 2015;29(4):343-355.
Xie Y, Xu E, Al-Aly Z. Risks of mental health outcomes in people with covid-19: cohort study. bmj. 2022;376
Wang PS, Demler O, Kessler RC. Adequacy of treatment for serious mental illness in the United States. American journal of public health. 2002;92(1):92-98.
National Alliance on Mental Illness. Black/African American. Available at: https://nami.org/Your-Journey/Identity-and-Cultural-Dimensions/Black-African-American#:~:text=One%20study%20showed%20that%2063,against%20due%20to%20their%20condition. Accessed May 25, 2023.
Primm A, Lawson B. African Americans, chapter in Disparities in Psychiatric Care. Ruiz & Primm editors. Washington, DC: Lippincott, Williams & Wilkins; 2010.
Bogner HR, de Vries HF. Integration of depression and hypertension treatment: a pilot, randomized controlled trial. The Annals of Family Medicine. 2008;6(4):295-301.
Baldwin-Clark T, Ofahengaue Vakalahi HF, Anderson B. What about African American older women and depressive symptoms? Educational Gerontology. 2016;42(5):310-320.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial Disclosures
• No financial disclosures were reported by Hossein Zare, Wehmah Jones, Manshu Yang, Nicole Jones, Vivienne Rose, Chidinma A. Ibe, or Darrell J. Gaskin.
• Michele Balamani receives consulting fees from the Gaston and Porter Health Improvement Center, Inc., which administers the Prime Time Sister Circles® Program (PTSC). The PTSC is the intervention that serves as the focus of this paper.
• Marilyn Gaston and Gayle Porter are the Co-Directors of the Gaston and Porter Health Improvement Center, Inc., which administers the PTSC. The PTSC is the intervention that serves as the focus of this paper.
• Denise L. Woods is an employee of the Gaston and Porter Health Improvement Center, Inc., which administers the PTSC. The PTSC is the intervention that serves as the focus of this paper.
Conflict of Interest:
The authors have no conflicts of interest to report. The Prime Time Sister Circles® Study is supported by a grant from the National Institute on Minority Health and Health Disparities (grant no. R01MD010462-05). Darrell J. Gaskin received this award. The National Institute on Minority Health and Health Disparities was not involved in the study design; in the collection, analysis, and interpretation of data; in writing this report; or in the decision to submit this paper for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zare, H., Ibe, C.A., Yang, M. et al. Evaluating the Impact of the Prime Time Sister Circles® Intervention on Reducing Depressive Symptoms Among African American Women with Uncontrolled Hypertension. J GEN INTERN MED 38, 2879–2887 (2023). https://doi.org/10.1007/s11606-023-08288-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08288-z