Abstract
Background
Delirium is among the most prevalent harmful events in hospitals that is associated with an elevated risk for severe outcomes such as functional decline, falls, longer length of stay, and increased mortality.
Objective
To evaluate the impact of the implementation of a multi-component delirium program on the prevalence of delirium and the incidence of falls among patients staying on general medicine inpatient hospital units.
Design
A pre-post intervention study using retrospective chart abstraction and interrupted time series analysis.
Cohort
Patients were selected from adult patients that stayed at least 1 day on one of the five general medicine units in a large community hospital in Ontario, Canada. A total of 16 random samples of 50 patients per month for 8 consecutive months pre-intervention (October 2017 to May 2018) and 8 months post intervention (January 2019 to August 2019) were selected for a total of 800 patients. There were no exclusion criteria.
Intervention
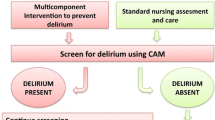
The delirium program included multiple components: education of staff and hospital leadership, twice per day bed-side screen for delirium, non-pharmacological and pharmacological prevention, and intervention strategies and a delirium consultation team.
Measurement
Delirium prevalence was assessed using the evidence-based delirium chart abstraction method, CHART-del. Demographic data as well as fall incidence were also collected.
Result
Our evaluation showed that the implementation of a multicomponent delirium program led to a reduction in delirium prevalence and fall incidences. The reduction in both delirium and falls was the largest for patients in the ages between 72 and 83 years old and varied across inpatient units.
Conclusion
A multi-component delirium program to improve the prevention, recognition, and management of delirium reduces the prevalence of delirium and fall incidence among patients in general medicine units.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Problem Description
Delirium is a common multifactorial condition among hospitalized patients that is associated with an elevated risk for severe outcomes such as functional decline, falls, longer length of stay, and increased mortality.1,2,3 It is also very common, accounting for 10% of all reported harmful hospital events in Canada,4 especially in older patients where delirium prevalence is estimated to be as high as 20%. Despite that up to 30–40% of cases is preventable5, it is often not recognized by clinicians in the early stages 6,7,8,9,10, and efforts to reduce the incidence of delirium are challenged by lack of delirium awareness; the conflation of delirium with dementia; and the absence of training and in-service education programs for physicians, nursing, and allied health staff.8,9
Available Knowledge
To address the multiple factors affecting the prevention and care for patients with delirium, multicomponent interventions are needed 11 and have been shown to reduce delirium incidence from 3% up to 30% in randomized trials as compared to usual care, 12,13,14 thereby improving the quality of life for patients and their families, while reducing healthcare costs and societal burden of delirium.15. These interventions often include the use of education, implementation of both non-pharmacological and pharmacological prevention strategies, and the support of inter-professional teams at the point of care to address potentially modifiable risk factors.15,16,17
Rationale
Our local hospital did not have a formalized delirium program. Therefore, based on the available knowledge, we developed, implemented, and evaluated a practical, evidence-informed multicomponent program for the prevention, early recognition, and effective management of delirium at a large community hospital.
Specific Aims
In this paper, we present the evaluation of a multi-component delirium program in a large community hospital serving a diverse population to understand the effectiveness of the intervention in reducing the number of delirium cases and falls analysed with pre-post Interrupted Time Series (ITS) design.
METHODS
Context
The delirium program was implemented at Trillium Health Partners (THP), a large community hospital, in Mississauga, Canada, serving a diverse population of over one million people. With 1379 inpatient beds, the hospital provides the full range of acute care hospital services. In the 5 years leading up to this implementation, a few other initiatives related to delirium and falls were initiated at THP. First, the organization attained Registered Nurses Association of Ontario (RNAO) Best Practice Spotlight Organization (BPSO) certification (2012–2015), during which time the Prevention of Falls and Fall Injuries in Older Adults Best Practice Guideline (BPG) was implemented across multiple units. After this, the RNAO Delirium, Dementia and Depression in Older Adults: Assessment and Care BPG was implemented in conjunction with the delirium program activities (2015–2021). This BPG was intentionally launched concurrently with the work related to the delirium program. The BPG team supported the educational efforts for the delirium program. The journey to BPSO certification could have stimulated a culture of change and learning which could have had a positive influence on the implementation and uptake of the delirium program.
This evaluation studied charts from patients that stayed on one of the 5 general medicine units at one of the three hospital sites. Implementation of the delirium program in these units started in June 2018. This evaluation examines the occurrence of study outcomes within the pre-implementation period (October 2017–May 2018) and the post-intervention period (January 2019–August 2019). This manuscript follows the Revised Standards for Quality Improvement Reporting Excellence (SQUIRE) reporting guidelines.18
Multicomponent Delirium Intervention
To change the existing model of delirium care in the organization, a team of administrators, clinicians, and scientists formed a project team and developed a multi-component delirium program based on current evidence. The developed delirium program intends to achieve three goals: (a) to prevent the onset of delirium, (b) to identify delirium when present, and (c) to improve the evidence-based management of delirium when identified.
Before implementation of the delirium program on inpatient hospital units, the project team engaged with “local” leadership (program directors, medical directors, unit managers, and charge nurse/clinical leaders) and staff to tailor the program to the context of the units. The pre-implementation activities included, but were not limited to, current state mapping, recruitment and training of delirium champions on each unit, and the creation of a delirium data dashboard and screening rate score cards for the units.
After the pre-implementation activities were completed, all clinical staff of the units were trained and the Delirium Program was implemented on the hospital units. The key components of the delirium program are the following: education on delirium for all staff involved, non-pharmacological and pharmacological delirium prevention strategies, delirium recognition with a bedside screener, and specific delirium management processes (order sheet) and strategies (see Fig. 1). More details can be found in Appendix 1.
Evaluation Study of a Multi-component Delirium Intervention
Implementation Assessment
In order to assess the implementation success of the delirium program, the two daily bedside delirium screening rates were calculated. The percentage of delirium screens done monthly for each of the 5 units was computed by dividing “the total number of delirium screens performed monthly per unit” over “the number of monthly bed days per unit, times 2” (times 2 since the delirium screen is done twice per day). The tracking of the delirium screening was done for 19 months after the start of the intervention for all patients that stayed on a unit in each given month to assess the implementation success; see Fig. 2. The post intervention chart abstraction was done for selected patients that stayed on the units in months 7–14 after the start of the implementation (see further the section below).
Effectiveness
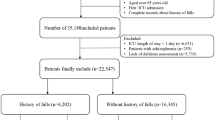
Previous evaluations of multicomponent interventions about delirium often use post-intervention study designs with small sample size, thereby limiting the assessment of effectiveness and generalizability.15 In order to assess the effectiveness of the multicomponent delirium program (hereafter also referred to as the intervention), we applied a pre-post evaluation study design using retrospective chart abstraction and Interrupted Time Series (ITS). ITS has increasingly been advocated as one of the more robust observational quasi-experimental designs for the evaluation of health system quality improvement interventions. The ITS design relies on data collected at multiple intervals over time before and after an intervention to establish a causal relationship between an intervention (e.g., delirium program) and an outcome of interest (e.g., delirium or falls).19 Based on Penfold and Zhang’s (2013), for our analysis, we considered a time period of 8 months before and after implementation of the intervention.20 For each month, we randomly selected a sample of 50 patients that stayed on any one of the 5 general medicine units. Patients were selected based on the month they were admitted to the hospital. For the pre-implementation period—October 2017 to May 2018—we selected 50 patients per month from 8 consecutive months in the period immediately prior to implementation of the delirium program in June 2018 (n = 400 patients). For the post-implementation period—January 2019 to August 2019—we selected 50 patients per month from 8 consecutive months starting 7 months after implementation of the delirium program to allow for the intervention to be fully implemented into practice (n = 400 patients). No stratification for unit or any other variable was used.
Patient Cohort
The study population included 800 adult patients aged 18 years or older who stayed for a minimum of 1 day on one of the 5 general medicine units during the data collection period (pre- or post-intervention). There were no exclusion criteria. The patient records covering their entire stay, including time in the emergency room and on other units, were used.
Measures
Delirium Screening
The bedside delirium screening was done using the Confusion Assessment Method (CAM)21,22,23, a brief delirium diagnostic tool that is accurate (sensitivity 86%, specificity 93%), with high inter-observer reliability.24
Delirium: CHART-del
The presence of delirium was assessed based on either clear physician-diagnosis of delirium as documented in physicians’ progress notes, consults or discharge summary, or by the validated chart-based identification method CHART-del.25 The chart abstraction involved a detailed review of the full patient’s medical records (a combination of paper and electronic medical records) and was designed with the goal of maximizing sensitivity for identification of delirium.25 Information on acute changes in mental status, time and duration of such episodes, evidence of agitation and reversibility or improvement of the acute confusion, and scanning and auditing medical records for the key words/terms for delirium identification were abstracted. Appendix 2 describes the data collection tool (CHART-del tool). The CHART-del tool is a validated instrument with good sensitivity and specificity (74% and 83% respectively) when compared to clinical assessment.25
Specialist consultation, restraint or safety attendant, falls, and bedside delirium screen
The following outcomes were collected for each patient during their entire hospital stay from their medical chart: received a specialist consultation, use of restraint, safety attendant/sitter, had a fall, and whether or not a screening was done for delirium using the CAM 22,23.
Data collection was performed by a research assistant (SA) who was fully trained in the CHART-del evidence-based method. Calibration and training had taken place as part of one other large study using the same methods.
Statistical Analysis
Descriptive statistics were performed, and values are presented as means and standard deviations (SD) for continuous values and counts (%) for categorical variables. Segmented regression was used to assess the impact of the multicomponent delirium intervention on the number of delirium cases and falls, by estimating the changes in level (and trend) in the post-intervention period compared to the pre-intervention period. Segmented regression analysis is a statistical method for modelling the interrupted time series data to draw more formal conclusions about the impact of an intervention on the measure of interest 26 (see Appendix 3). The datasets used and/or analyzed during the current study are available from the corresponding author on request.
Ethical Considerations
The THP Research Ethics Board approved this evaluation. Patients did not consent since the study operated under a waiver of patient consent because of the low risk of chart abstraction methodology.
RESULTS
Cohort
The characteristics of the patients in the pre- and post-intervention cohorts are reported in Table 1. There were no differences in the distribution of sex, age, place of residence, or hospital admission route between the pre- and post-intervention cohorts.
Implementation Assessment
As a measure of the implementation success of the delirium program, the two daily CAM screenings were tracked for the medicine units. Figure 2 represents the uptake for the first 19 months after implementation. The period in the post-implementation phase that is used for the evaluation is shaded in gray. The average CAM screening rates over our study period ranged from 65% for unit 4, 72% for unit 5, 75% for unit 2, 82% for unit 1, to 90% for unit 3.
Effectiveness
Main Results
The average number of patients with delirium per month over 50 patients decreased significantly from 10.25 (SD 1.83) before the implementation of the intervention to 7.38 (SD 2.39) after (see Table 2, Fig. 3, and Appendix 3) (p = 0.026, Std. error = 1.11). This is a relative reduction of 27.15% in the number of delirium cases per month. The estimate of the intervention effect did not change after adjusting the linear model for the negative autocorrelation in the error term, whereas it slightly reduced after accounting for the heterogeneity across units but remained significant (p = 0.037, Std. error = 1.021) (see Appendix 3, Table 1a).
The average number of patients who experienced a fall per month over 50 patients decreased significantly from 14.5 (SD 3.0) before the implementation of the intervention to 11.8 (SD 2.0) after (see Table 2, Fig. 4, and Appendix 3) (p = 0.049, Std. error = 1.28). This is a relative reduction of 18.97% in the number of falls per month. The estimate of the intervention effect did not change after adjusting the linear model for the negative autocorrelation in the error term, whereas the intervention effect reduced after accounting for the heterogeneity across units and became non-significant (p = 0.538, Std. error = 1.271) (see Appendix 3).
Explorative Analysis
As an explorative analysis, we examined the distribution of the number of delirium cases and falls within different age groups and within individual hospital units to gain insights into which segment of patients benefited most from the intervention. These results showed a 14.7% reduction in delirium among patients aged between 72 and 83 years of age (relative reduction 65.4%) (p = 0.01) and a 21% reduction in delirium among patients that stayed on Unit 3 (relative reduction 59.5%) (p = 0.03). Furthermore, we saw a 10.3% reduction in falls among patients that stayed on Unit 1 (relative reduction 41.2%) (p = 0.03). Although most other age groups and units saw a decrease in delirium and falls, none of the differences reached statistical significance, for some instances likely due to lack of power, since the study was not designed for this kind of explorative analysis, or due to a floor effect. Also of note is the large spread in delirium rates, from 10 to 35%, and falls, from 10 to 23%. Additionally, there is a large spread from pre-intervention to post-intervention in the absolute difference in delirium across the units: from an increase of 2% to a decrease of 21%; and for falls: from an increase of 2.5% to a decrease of 13.3% for falls (see Tables 3 and 4).
In Table 5, the descriptive statistics of the secondary outcomes before and after the implementation of the intervention are reported. The number of bedside screens for delirium was significantly higher after the implementation (97.8%) compared to before (20%), indicating an excellent uptake of this part of the intervention. Furthermore, no significant differences were found for length of stay, restraint, or safety attendant use.
DISCUSSION
Summary
Our evaluation of the multicomponent delirium program showed that the implementation led to a reduction in the number of patients with delirium, as well as a reduction in the number of patients that experienced a fall. The impact on falls should be interpreted with caution since the model that corrected for heterogeneity was not significant for the falls outcome. The reduction in delirium and falls was the largest in patients aged between 72 and 83 years old. Both older and younger patients were not improving as much. An individual’s delirium risk depends on both pre-disposing factors that influence ones’ vulnerability and precipitation factors that determine how noxious an insult is for the individual. The level of both of these determines one’s risk for delirium.27 In our case, it is likely that the older hospitalized adults aged 83 and above are very vulnerable so that even a mild insult can lead to the development of delirium thus making prevention challenging. On the contrary, in the younger population that is less vulnerable, only severe or repeated insults will lead to the development of delirium. These more severe insults such as surgery might not be preventable. A similar argument can be made for our fall results. Falls is a common geriatric syndrome that is multifactorial and mostly the result of a combined action of predisposing and precipitating factors much like delirium. Furthermore, falls and delirium share similar risk factors such as age and cognitive decline.28
In addition, our evaluation shows that the impact of the delirium program was not universal across all engaged hospital units. There are likely several factors at play that could potentially have influenced these results. First, we see that the uptake of the overall intervention, as approximated by the implementation of the bedside screen for delirium with the CAM tool, varied across different units. The unit (no. 3) with the best uptake of the bedside screen did have the largest reduction in delirium rates which could indicate that when the program is successfully implemented it has the potential to significantly reduce delirium rates. Screening for delirium, however, was only one of the core components of the delirium program; therefore, caution needs to be taken with the generalization to the implementation success of the full program. Second, we noticed that the baseline delirium rate had a large variation across units. For some units where this rate was relatively low compared to other units, we did not see much change after implementation of the program, which could have been the result of a floor effect. Third, implementing an elaborate program is labor intensive as it involves many healthcare professionals coordinating multiple tasks. Studies show that the “readiness” of hospital units and the unit context (time, workload, workflow, competing priorities, and staff turnover) are key factors to the success of new programs.29 Finally, as noted above, the risk for the development of delirium is multifactorial. A difference in any factor across units could have influenced the effectiveness of the delirium program on each particular unit. The statistical analysis applied in the current study, however, corrected for potential heterogeneity across the units and showed a significant impact of the multi-component delirium intervention on the reduction of delirium after controlling for heterogeneity.
This multi-component delirium program was well resourced with the dedication of project leads, a dedicated project team, and the luxury of time to try things out. It remains a challenge with multicomponent interventions to pinpoint which components were key to the success on some units and which components were lacking on the less successful units. Previous research has shown the importance of education, champions, screening, and continuous support from hospital management.30 For future research, it would be interesting to measure these in order to expand the knowledge on which preconditions and key components contribute to success (e.g., adequate staffing levels; strong leadership support; clinical and managerial engagement) using a mixed methods design.
In our study population, the implementation of the delirium program did not change the length of stay, the use of safety attendants, or restraints. The length of hospital stay depends on a wide variety of factors that are related to, for example, the setting, clinical care, or logistics. Although the delirium program targeted some components related to these factors such as clinical pathways,31 patient mobility,32,33 medication management34, and collaborative care, it is important to underline that it was not specifically designed to reduce length of stay.
The implementation of delirium prevention programs within hospitals is currently at the discretion of hospital leadership and as a result not universally applied. Therefore, the creation of a standard delirium strategy within all acute care centers that focuses on components such as prevention, screening, and delirium management strategies that are evidence based is needed. Currently, hospitals in Ontario need to report the incidence of delirium35 which is a good start to have hospitals incentivize systematic screening and improve awareness; however, without a mechanism to respond to a positive delirium screen, this effort will fall short in improving delirium-related morbidities and mortalities.
Unlike many other studies, no specific exclusion criteria were applied other than being hospitalized on a medicine unit. This allows for an increased generalizability of our findings to other hospitals’ medicine units. The use of chart abstraction in this study allowed data collection for both the pre-intervention period and post-intervention period providing data suitable for a strong evaluation design using ITS analysis. Other studies evaluating delirium prevention programs are often limited to data from the post-intervention period or report on other main outcomes than delirium. We do recognize that a limitation of the use of the chart abstraction method is that it is inevitable that some cases might be systematically mislabeled as either false negative or false positive. However, previous research demonstrated that the CHART-del method has a reasonable sensitivity and specificity and any under- or overestimation should be stable over time and temporal trends should remain meaningful.25 Another limitation of the study was the use of aggregate data for each time point (i.e., data were aggregated across units). Current ITS methods, including segmented regression, do not account for the heterogeneity among patients and across sites, which can imply loss of power.36 In order to address the problem, we implemented a recent proposal by Ewusie and colleagues called weighted segmented regression.37,38
Future research might benefit from a larger sample size as well as the assessment of patient-related factors such as medical comorbidities or frailty to allow for segmentation of the patient population and de-aggregation of the data to identify who benefits and why. Furthermore, a deeper understanding of the implementation process will be key such as readiness for change, leadership involvement and endorsement, staffing ratios, and availability of real-time data to support practice changes. Together, this could increase our insights into what factors contribute to the successful implementation and sustainability of delirium programs.
CONCLUSION
Our results demonstrate that the implementation of a multicomponent delirium program on general medicine hospital units is associated with reductions in delirium and falls, with the strongest effects seen in the most vulnerable patients. Hence, we believe that multi-component interventions focused on education and screening, with delirium prevention and management strategies, can have demonstrable impacts on changing patient outcomes, reduce harm, and improve practice.
Data Availability:
Available upon request.
References
Hullick C, Conway J, Higgins I, et al. An assistant workforce to improve screening rates and quality of care for older patients in the emergency department: findings of a pre-post, mixed methods study. BMC Geriatr. 2018;18(1):126.
Piotrowicz K, Rewiuk K, Górski S, et al. The "Wholesome Contact" non-pharmacological, volunteer-delivered multidisciplinary programme to prevent hospital delirium in elderly patients: study protocol for a randomised controlled trial. Trials. 2018;19(1):439-439.
Reston JT, Schoelles KM. In-facility delirium prevention programs as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5 Pt 2):375-380.
Chan B, Cochrane D. Canadian Institute for Health Information, Canadian Patient Safety Institute. Measuring Patient Harm in Canadian Hospitals. With What can be done to improve patient safety?. CIHI. 2016;Ottawa, ON.
Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911-922.
Mast R, Huyse F, Drooglever H, et al. Richtlijn Delirium. Amesterdam 2004.
Ritter SRF, Cardoso AF, Lins MMP, Zoccoli TLV, Freitas MPD, Camargos EF. Underdiagnosis of delirium in the elderly in acute care hospital settings: lessons not learned. Psychogeriatrics. 2018;18(4):268-275.
Yanamadala M, Wieland D, Heflin MT. Educational Interventions to Improve Recognition of Delirium: A Systematic Review. 2013;61(11):1983-1993.
Teodorczuk A, Reynish E, Milisen K. Improving recognition of delirium in clinical practice: a call for action. BMC Geriatr. 2012;12:55.
van Velthuijsen EL, Zwakhalen SMG, Mulder WJ, Verhey FRJ, Kempen G. Detection and management of hyperactive and hypoactive delirium in older patients during hospitalization: a retrospective cohort study evaluating daily practice. Int J Geriatr Psychiatry. 2018;33(11):1521-1529.
Kalisvaart CJ, Vreeswijk R, de Jonghe JF, Milisen K. [A systematic review of multifactorial interventions for primary prevention of delirium in the elderly]. Tijdschr Gerontol Geriatr. 2005;36(6):224-231.
Siddiqi N, Harrison JK, Clegg A, et al. Interventions for preventing delirium in hospitalised non-ICU patients. Cochrane Database Syst Rev. 2016;3:Cd005563.
Janssen TL, Alberts AR, Hooft L, Mattace-Raso F, Mosk CA, van der Laan L. Prevention of postoperative delirium in elderly patients planned for elective surgery: systematic review and meta-analysis. Clin Interv Aging. 2019;14:1095-1117.
Godfrey M, Green J, Smith J, et al. Process of implementing and delivering the Prevention of Delirium system of care: a mixed method preliminary study. BMC Geriatr. 2019;20(1):1.
Hshieh TT, Yue J, Oh E, et al. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med. 2015;175(4):512-520.
Bauernfreund Y, Butler M, Ragavan S, Sampson EL. TIME to think about delirium: improving detection and management on the acute medical unit. BMJ Open Qual. 2018;7(3):e000200.
Schubert M, Schürch R, Boettger S, et al. A hospital-wide evaluation of delirium prevalence and outcomes in acute care patients - a cohort study. BMC Health Serv Res. 2018;18(1):550.
SQUIRE 2.0 Guidelines SQUIRE. http://squire-statement.org/index.cfm?fuseaction=Page.ViewPage&PageID=471. Published 2020. Accessed 28 Sep 2022.
Hategeka C, Ruton H, Karamouzian M, Lynd LD, Law MR. Use of interrupted time series methods in the evaluation of health system quality improvement interventions: a methodological systematic review. BMJ Glob Health. 2020;5(10).
Penfold RB, Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr. 2013;13(6 Suppl):S38-44.
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941-948.
Wei LA, Fearing MA, Sternberg EJ, Inouye SK. The Confusion Assessment Method: a systematic review of current usage. J Am Geriatr Soc. 2008;56(5):823-830.
Helfand BKI, D'Aquila ML, Tabloski P, et al. Detecting Delirium: A Systematic Review of Identification Instruments for Non-ICU Settings. J Am Geriatr Soc. 2021;69(2):547-555.
Wong CL, Holroyd-Leduc J, Simel DL, Straus SE. Does this patient have delirium? Value of bedside instruments. Jama. 2010;304(7):779-786.
Inouye SK, Leo-Summers L, Zhang Y, Bogardus ST, Jr., Leslie DL, Agostini JV. A chart-based method for identification of delirium: validation compared with interviewer ratings using the confusion assessment method. J Am Geriatr Soc. 2005;53(2):312-318.
Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299-309.
Inouye SK. Prevention of delirium in hospitalized older patients: risk factors and targeted intervention strategies. Ann Med. 2000;32(4):257-263.
Iamaroon A, Wongviriyawong T, Sura-Arunsumrit P, Wiwatnodom N, Rewuri N, Chaiwat O. Incidence of and risk factors for postoperative delirium in older adult patients undergoing noncardiac surgery: a prospective study. BMC Geriatr. 2020;20(1):40.
Geerligs L, Rankin NM, Shepherd HL, Butow P. Hospital-based interventions: a systematic review of staff-reported barriers and facilitators to implementation processes. Implement Sci. 2018;13(1):36.
Godfrey M, Smith J, Green J, Cheater F, Inouye SK, Young JB. Developing and implementing an integrated delirium prevention system of care: a theory driven, participatory research study. BMC Health Serv Res. 2013;13(1):341.
Rotter T, Kinsman L, James E, et al. Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev. 2010(3): Cd006632.
Hoyer EH, Friedman M, Lavezza A, et al. Promoting mobility and reducing length of stay in hospitalized general medicine patients: A quality-improvement project. J Hosp Med. 2016;11(5):341-347.
Surkan MJ, Gibson W. Interventions to Mobilize Elderly Patients and Reduce Length of Hospital Stay. Can J Cardiol. 2018;34(7):881-888.
Corbi G, Gambassi G, Pagano G, et al. Impact of an Innovative Educational Strategy on Medication Appropriate Use and Length of Stay in Elderly Patients. Medicine (Baltimore). 2015;94(24):e918-e918.
Canadian Institute for Health Information. Hospital Harm Indicator General Methodology Notes. CIHI. 2021;Ottawa, Ontario.
Taljaard M, McKenzie JE, Ramsay CR, Grimshaw JM. The use of segmented regression in analysing interrupted time series studies: an example in pre-hospital ambulance care. Implement Sci. 2014;9:77.
Ewusie J, Thabane L, Beyene J, Straus SE, Hamid JS. MultiCenter Interrupted Time Series Analysis: Incorporating Within and Between-Center Heterogeneity. Clin Epidemiol, 2020;12, 625–636.
Ewusie J, Beyene J, Thabane L, Straus SE, Hamid JS. An improved method for analysis of interrupted time series (ITS) data: accounting for patient heterogeneity using weighted analysis. Int J Biostat. 2021; doi:https://doi.org/10.1515/ijb-2020-0046
Acknowledgements:
The authors thank the many hospital staff members, project team members, and patients, who supported the multicomponent delirium program.
Funding
This work is supported by the Medical Psychiatry Alliance, a collaborative health partnership of the University of Toronto, the Centre for Addiction and Mental Health, the Hospital for Sick Children, Trillium Health Partners, the Ontario Ministry of Health and Long- Term Care, and an anonymous donor.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest:
The authors declare that they do not have a conflict of interest.
Permission to Reproduce Material from Other Sources:
NA
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior Presentations: none
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Versloot, J., Minotti, S.C., Amer, S. et al. Effectiveness of a Multi-component Delirium Prevention Program Implemented on General Medicine Hospital Units: an Interrupted Time Series Analysis. J GEN INTERN MED 38, 2936–2944 (2023). https://doi.org/10.1007/s11606-023-08238-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08238-9