Abstract
Background
Cannabis may be a substitute for opioids but previous studies have found conflicting results when using data from more recent years. Most studies have examined the relationship using state-level data, missing important sub-state variation in cannabis access.
Objective
To examine cannabis legalization on opioid use at the county level, using Colorado as a case study. Colorado allowed recreational cannabis stores in January 2014. Local communities could decide whether to allow dispensaries, creating variation in the level of exposure to cannabis outlets.
Design
Observational, quasi-experimental design exploiting county-level variation in allowance of recreational dispensaries.
Subjects
Colorado residents
Measures
We use licensing information from the Colorado Department of Revenue to measure county-level exposure to cannabis outlets. We use the state’s Prescription Drug Monitoring Program (2013–2018) to construct opioid-prescribing measures of number of 30-day fills and total morphine equivalents, both per county resident per quarter. We construct outcomes of opioid-related inpatient visits (2011–2018) and emergency department visits (2013–2018) with Colorado Hospital Association data. We use linear models in a differences-in-differences framework that accounts for the varying exposure to medical and recreational cannabis over time. There are 2048 county-quarter observations used in the analysis.
Results
We find mixed evidence of cannabis exposure on opioid-related outcomes at the county level. We find increasing exposure to recreational cannabis is associated with a statistically significant decrease in number of 30-day fills (coefficient: −117.6, p-value<0.01) and inpatient visits (coefficient: −0.8, p-value: 0.03), but not total MME nor ED visits. Counties with no medical exposure prior to recreational legalization experience greater reductions in the number of 30-day fills and MME than counties with prior medical exposure (p=0.02 for both).
Conclusions
Our mixed findings suggest that further increases in cannabis beyond medical access may not always reduce opioid prescribing or opioid-related hospital visits at a population level.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Cannabis legalization has become one potential policy states have implemented, in part, to help reduce the tide of harm and death caused by the evolving opioid crisis that continues to kill thousands of Americans every year.[1,2,3] By 2022, 37 states legalized access to medical cannabis and 21 states legalized access to recreational cannabis.[4]
Findings on whether cannabis legalization leads to reductions in opioid consumption or resulting adverse events such as overdoses have been contradictory. Findings obtained from healthcare prescription claims data showed that increased access to cannabis is associated with lower opioid prescribing.[5,6,7,8,9,10] Additional evidence suggested that the legalization of cannabis, or in some cases, allowances for dispensaries, was associated with reduced opioid-related mortality.[11,12,13,14,15,16,17,18] However, Shover et al. (2019) found that by extending the years of data over which the association is analyzed, the negative association between medical-cannabis laws and opioid-related mortality not only dissipates, but reverses itself.[19]
Most previous studies in this area have used state-level policy changes to analyze the association between cannabis legalization and opioid use. State-level policy indicators mask the substantial variation at the local level in terms of cannabis access and availability, since most states allow local jurisdictions to opt out of retail sales.[20,21] This has led some to criticize earlier findings for suffering from an aggregation bias or ecological fallacy.[22,23] However, only formal randomized controlled trials can truly determine whether cannabis is a substitute for opioids in pain management.[24] Very limited work at the individual level using survey or trial data from specific geographic areas showed that cannabis was not a substitute for opioid use.[25,26,27,28]
In the current paper, we add to the ongoing debate regarding the relationship between cannabis legalization and opioid-related harms by exploiting the geographic availability of cannabis within a single state, Colorado. Using within-state data eliminates the problem of confounding differential state policy approaches to the opioid epidemic, which are often ignored.[17] While opioid mortality has risen over time, Colorado has experienced lower opioid-related mortality rates than the national average.[29] Furthermore, there is often a gap in time between when a state passes a legalization law and when dispensaries actually open to the public.
Colorado is unique in that it was an early adopter of both medical (2000) and recreational cannabis (2012), where medical dispensaries could begin operating in 2010 and recreational in 2014. However, local communities allowed dispensary sales, which created a unique natural experiment in dispensary exposure. Counties that adopted medical cannabis sales prior to recreational may have more population-wide experience with cannabis use. If access to cannabis reduces opioid use and resulting sequelae, then we hypothesize that counties with no or low baseline exposure to medical cannabis should see a larger impact of exposure to recreational cannabis than counties with prior high medical exposure.
METHODS
Data Sources and Measures
Several data sources were used for this study that broadly cover the period January 1, 2011, through December 31, 2018. A few exceptions are noted below.
Cannabis Dispensary Data
Information on the number of medical and recreational cannabis dispensaries per county were obtained from the Colorado Department of Revenue (DOR). The DOR data includes license number, name, and address information, making it possible to identify when the dispensary began operating for which type, since co-located medical and recreational dispensaries have different license numbers.
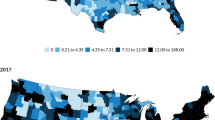
The state began accepting applications for medical dispensary licenses in 2010; however, the first applications were not recorded until November 2010 as it took time for Colorado to set up its system. For this reason, we limit the license data to 2011 onward, and include information only on approved dispensaries. Licensing of recreational dispensaries went into effect in January 2014, although only existing medical cannabis dispensaries were initially allowed to apply for a recreational license for the first three quarters of 2014.[30] As late as 2013, nearly 50% of county jurisdictions in Colorado did not allow even medical dispensaries.
Exposure to cannabis markets is measured in three ways. First, we defined recreational exposure with an indicator for when a county had one or more new recreational stores post legalization. Second, to capture exposure to medical dispensaries, we divided counties into three groups based on their level of exposure to medical cannabis dispensaries in each quarter: no dispensary counties (50% of our sample); low (fewer than 10, 40% of our sample); and high (10 or more, 10% of our sample). For the sensitivity analysis, we stratified counties into whether they had no or any medical dispensaries at baseline. We hypothesized that the “no medical” dispensary counties are more “exposed” to the passage of legal recreational cannabis than the high baseline dispensary exposure group, and thus should see a bigger effect on opioid-related outcomes.
Colorado Prescription Drug Monitoring Program (PDMP) Database
Legally prescribed opioids are often the gateway for many opioid addictions and still represent a key drug in physician-monitored pain management. The PDMP also captures patients with non-chronic-opioid prescriptions, who also may substitute cannabis for opioids. This database captures adjudicated pharmacy claims for all US Drug Enforcement Agency scheduled drugs, and comes from the Colorado Department of Regulatory Agencies. In 2012, the PDMP switched data vendors and the levels of reported prescriptions changed markedly. Thus, we limited the use of the PDMP data for the period 2013–2018. Because all licensed pharmacies report data directly to the PDMP on every prescription filled involving a scheduled substance, [31] the PDMP effectively represents the entire population of Colorado being prescribed an opioid; and hence, it provides us with the strongest measure of opioid prescribing patterns available. Other claims databases miss the uninsured and those paying cash. Opioids were identified using the Centers for Disease Control and Prevention’s list of outpatient opioids that are identified at the National Drug Code level.[32]
We construct two measures of prescribing from the PDMP data. The first is the number of 30-day fills per county resident. The second is the total morphine milligram equivalents (MME) per capita. The calculation of MME multiplies the prescription strength, the quantity dispensed, and the MME conversion factor,[33] and then divides this amount by the days supplied.[34] We combined overlapping and concurrent fills to assign each patient a daily MME following previous work.[34] Each prescription was summed to create the total MME for the quarter and then divided by the total number of residents in the county.
Colorado Hospital Association (CHA)
While the PDMP captures legally prescribed opioids, we know that illicit opioid markets continue to proliferate.[3] For this reason, we use CHA data on inpatient and emergency department (ED) visits at general and acute care hospital facilities, allowing us to identify opioid-related visits regardless of whether the opioids were purchased legally or illegally.[35] CHA’s data captures downstream effects of opioid use from all insurance types, including the uninsured.
We use inpatient discharges for the period 2011–2018, but because CHA did not begin collecting ED visits until 2013, the ED visits cover only 2013–2018. For both the inpatient and ED visits, we identify opioid-related hospital visits using the International Classification of Disease (ICD) Version 10 codes and their corresponding Version 9 codes, though we report just the Version 10 codes here for brevity. These diagnosis codes included opioid use, misuse or dependence (F11*), opioid poisonings (T400*–T404*, T406*, and T507*), and the long-term use of opioids (Z798*). We err on the side of being more comprehensive in the codes included because of the difficulty in exactly crosswalking ICD codes between Versions 9 and 10. We constructed two measures: (1) the number of opioid-related inpatient visits per capita per county, and (2) the number of opioid-related ED visits per capita per county. Both were based on the patient’s county of residence.
Analytic Approach
Our analytic method uses recent developments in the quasi-experimental design literature for difference-in-differences designs. Recent work has shown that treatment effects can be biased when the treatment occurs at different times.[36,37] In our context, counties opening recreational stores in later years may have a different treatment effect because the potency of cannabis products increased while the price decreased over time. As a result, we implement the Gardner (2021) two-stage difference-in-difference approach: (1) estimate the outcome in the never treated/pre-treated observations, controlling for time and county fixed effects; and (2) estimate the treatment variable on the difference between the treated observations and the estimated never/pre-treated trend. We use the following model:
Where yit is the outcome in county i in quarter t. Xit is the calendar year county unemployment rate and total number of county hospital admissions, drawn from the Bureau of Labor Statistics[38] and the American Health Resource File,[39] respectively. We also include the categorical variable for the baseline level of medical dispensaries (none, low, high) in county i at quarter t. δt is the interaction of year * quarter fixed effects and γi are county fixed effects.
The second stage estimates the average outcome in all counties minus the estimated effect in the untreated counties to isolate the effect of initiating recreational sales in a county with the following model:
Where yit is our opioid outcome of interest in county i and quarter t. The parameter \(\alpha_{l}\) captures the impact of recreational stores opening in the county (\({RecExposure}_{it}\)). Standard errors are clustered at the county level. We used the did2s command in R to estimate the models.[40] The RAND Human Subjects Protection Committee deemed this study to be exempt from human subjects protections.
RESULTS
Over the entire period, the number of medical dispensaries per capita did not change markedly, hovering around 1 per 10,000 residents per county per quarter, or about 8 dispensaries per county per quarter (Table 1). Recreational dispensaries increased from 3.6 per county per quarter in 2014 to 8.5 in 2018. While total MME and number of 30-day fills generally decreased from 2015 onward, rates of opioid-involved inpatient and ED visits both rose through 2017.
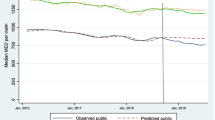
For all opioid-related outcomes, the trends do not indicate an immediate drop in opioid prescribing or opioid-related hospital visits post legalization. Figure 1 shows the downward trend in number of 30-day fills and MME after 2015 which is consistent across levels of baseline medical dispensary exposure. Counties with no prior medical exposure have higher levels of opioid use. Figure 2 shows trends in the quarterly average number of opioid-involved ED visits (left panel) and inpatient visits per 10,000 residents (right panel) for the study period. In the upper panel, areas with higher levels of medical dispensary exposures have higher absolute levels of opioid-involved visits compared to counties with relatively low or no exposure, although the trends are generally consistent. When we adjust for population within the county (lower panel), the differences in levels shrink; however, the counties with no baseline medical exposure have a generally higher level of opioid-related ED visits in later years.
Trends in number of 30-day fills and total MME, by level of medical-cannabis dispensary exposure, 2011–2018. MME, milligram morphine equivalents. The vertical line represents the start of legal recreational sales in January 2014, when recreational dispensaries were allowed to open. Counties are categorized according to the number of medical-cannabis dispensaries in Quarter 3, 2012. The dotted bars indicate the level of opioid-related visits in the highest exposure medical-cannabis counties; the dashed lines show the outcomes in counties with 1–9 medical dispensaries; and the solid lines show trends in counties with no medical dispensaries as of November 2012, prior to legalization of recreational cannabis.
Trends in opioid-involved ED and inpatient visits, by level of medical-cannabis dispensary exposure, 2011–2018. The vertical line represents the start of legal recreational sales in January 2014, when recreational dispensaries were allowed to open. Counties are categorized according to the number of medical dispensaries in Quarter 3, 2012 (none; 1–9; and 10+). The dotted lines indicate the level of opioid-related visits in the highest exposure medical cannabis counties; the dashed lines show the outcomes in counties with 1–9 medical dispensaries; and the solid lines show trends in counties with no medical dispensaries as of November 2012, prior to legalization of recreational cannabis.
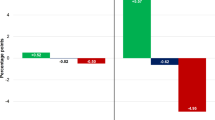
Table 2 provides the primary findings of the impact of exposure to cannabis dispensaries on opioid-related outcomes. We find a significant reduction in the number of 30-day fills after legalization of recreational cannabis of −117.6 fills per county per quarter. Counties with exposure to one or more recreational cannabis dispensary had −0.8 fewer hospitalizations per 10,000 residents per quarter (p=0.03), than counties with no recreational cannabis. For a sense of scale, there are approximately 715,000 Denver residents, which would imply 57 fewer opioid related inpatient visits per quarter in Denver (700k/10k * 0.8 = 57). We found no statistically significant direct effect of recreational dispensaries on either opioid-involved ED visits or total MME prescribed per resident per county per quarter.
In the sensitivity analysis, we stratified counties by whether they had previous exposure to medical cannabis, under the hypothesis that counties with no experience with medical should experience greater reductions in opioid use following recreational cannabis legalization, than counties with previous medical dispensary exposure (Table 3). We found that the number of 30-day fills dropped −130.3 compared with −120.9 in counties with prior exposure, and the MME drops −33.8 compared with −7.5 in counties with prior medical exposure (both significant at the 5% level).
DISCUSSION
With Colorado’s rapid growth in recreational dispensaries, we find a statistically significant drop in prescribing of −117.6 fills per county per quarter, while the total MME per resident remained unchanged. We found a −0.8 per 10,000 residents decrease in opioid-related inpatient visits, but no statistically significant impact on ED visits.
The PDMP data capture legally prescribed opioids. The MME may not have changed if patients who required access to cannabis for medicinal purposes had sufficient access under the previous medical cannabis policy, even in counties where medical dispensaries were not available. The reduction in fills may be among patients only occasionally filling opioid prescriptions whereas overall MME may stay more constant if the higher MMEs are coming from chronic pain patients.
The direction of effects we find for ED and inpatient visits is consistent with the hypothesis that cannabis may substitute for opioids (though ED visits are not statistically significant), but contrasts with two recent studies using sub-state data to assess the relationship between cannabis availability and opioid-related hospitalizations. Freisthler et al. (2020) use sub-state data in California and found dispensaries were associated with increased opioid-related hospitalizations.[41] Liang and Shi (2019) find that recreational dispensaries are positively associated with opioid use disorder diagnoses coded during an inpatient stay, but no association was found for medical dispensaries.[42] Due to the shift from using ICD9 to 10 during the study periods, we cannot rule out there is some measurement error in the outcomes between studies due to the exact codes used.
While the main models control for medical exposure, we also conducted a sensitivity analysis stratifying on whether a county had prior medical exposure to assess the differential impact of recreational cannabis in counties with no prior medical exposure. We find that counties with no prior medical exposure had greater decreases in both 30-day fills and MME than counties with prior exposure to medical dispensaries. The changes in ED or inpatient visits for opioid-related outcomes were generally not significant, though there was a statistically significant decline in ED visits for the counties with prior medical-dispensary exposure. The finding for the opioid prescribing outcomes is consistent with our hypothesis that areas with little exposure to medical cannabis prior to legalization would experience larger reductions in opioid-related outcomes as new recreational stores opened up, compared to counties which already had access to cannabis through the medical market.
The paper has several limitations. First, despite using sub-state data, our study may still suffer from aggregation bias given our focus on the county level. Second, our analysis ignores county-specific policies targeting the opioid epidemic that are time varying, such as differential distribution of naloxone or inappropriate prescribing campaigns. The exclusion of these local policies and campaigns should have biased results away from zero, if they were positively correlated with expansion of recreational cannabis markets. Third, while CHA represents nearly all Coloradans, there is variation in the hospitals and emergency departments reporting data to CHA. Moreover, the CHA outcomes used in this study reflect heavy or hazardous use of opioids sufficiently risky to generate a hospital or ED visit. Other margins of opioid use without a prescription or a physician’s supervision may not have the same relationship as those identified here.
Unfortunately, our findings do not clarify the muddy waters of the debate surrounding cannabis’s utility as a substitute for opioids and/or a treatment for opioid use disorder.[26,27,28,43] Sales from the adult-use market exceeded that from the medical market before the end of the first year of recreational sales in 2014, and have only continued to grow at double digit rates since.[44] However, we do not find similar blockbuster declines in opioid prescribing or opioid-related hospital visits. This suggests that while cannabis may have therapeutic benefits to patients suffering with particular ailments, it is not the panacea for solving the opioid crisis. Future work should examine changes in opioid utilization patterns using individual-level data to see if community exposure to cannabis changes opioid utilization among individuals, or among certain types of patients using opioids, such as the casual user versus the chronic pain patient.
Data Availability
Outcome data used in this study are proprietary to the data set owners and are not available for use from the authors.
REFERENCES
CDC. Provisional Drug Overdose Death Counts. Centers for Disease Control and Prevention. Accessed 8/26/21, https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
Stephenson J. CDC Warns of Surge in Drug Overdose Deaths During COVID-19. JAMA Health Forum. 2021;2(1) https://doi.org/10.1001/jamahealthforum.2021.0001
NIDA. Drug Overdose Death Rates. National Institute on Drug Abuse. Accessed 3/6/2023, https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates
NCSL. State Medical Marijuana Laws. National Conference of State Legislatures. https://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx
Bradford AC, Bradford WD. Medical Marijuana Laws Reduce Prescription Medication Use In Medicare Part D. Health Aff (Millwood). 2016;35(7):1230-6. https://doi.org/10.1377/hlthaff.2015.1661
Bradford AC, Bradford WD, Abraham A, Bagwell Adams G. Association Between US State Medical Cannabis Laws and Opioid Prescribing in the Medicare Part D Population. JAMA Intern Med. 2018;178(5):667-672. https://doi.org/10.1001/jamainternmed.2018.0266
Wen H, Hockenberry JM. Association of Medical and Adult-Use Marijuana Laws With Opioid Prescribing for Medicaid Enrollees. JAMA Intern Med. 2018;178(5):673-679. https://doi.org/10.1001/jamainternmed.2018.1007
Wen J, Wen H, Butler JS, Talbert JC. The impact of medical and recreational marijuana laws on opioid prescribing in employer-sponsored health insurance. Health Econ. 2021;30(5):989-1000. https://doi.org/10.1002/hec.4237
Shi Y, Liang D, Bao Y, An R, Wallace MS, Grant I. Recreational marijuana legalization and prescription opioids received by Medicaid enrollees. Drug Alcohol Depend. 2019;194:13-19. https://doi.org/10.1016/j.drugalcdep.2018.09.016
Liang D, Bao Y, Wallace M, Grant I, Shi Y. Medical cannabis legalization and opioid prescriptions: evidence on US Medicaid enrollees during 1993-2014. Addiction. 2018;113(11):2060-2070. https://doi.org/10.1111/add.14382
Chihuri S, Li G. State marijuana laws and opioid overdose mortality. Inj Epidemiol. 2019;6:38. https://doi.org/10.1186/s40621-019-0213-z
Wendelboe AM, Mathew R, Chongsuwat T, et al. Is There Less Opioid Abuse in States Where Marijuana Has Been Decriminalized, Either for Medicinal or Recreational Use? A Clin-IQ. J Patient Cent Res Rev. Fall 2019;6(4):267-273. https://doi.org/10.17294/2330-0698.1704
Smart R, Pacula RL. Early evidence of the impact of cannabis legalization on cannabis use, cannabis use disorder, and the use of other substances: Findings from state policy evaluations. Am J Drug Alcohol Abuse. 2019;45(6):644-663. https://doi.org/10.1080/00952990.2019.1669626
Chan NW, Burkhardt J, Flyr M. The Effects of Recreational Marijuana Legalization and Dispensing on Opioid Mortality. Economic Inquiry. 2020;58(2):589-606.
Bachhuber MA, Saloner B, Cunningham CO, Barry CL. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999-2010. JAMA Intern Med. 2014;174(10):1668-73. https://doi.org/10.1001/jamainternmed.2014.4005
Livingston MD, Barnett TE, Delcher C, Wagenaar AC. Recreational Cannabis Legalization and Opioid-Related Deaths in Colorado, 2000-2015. Am J Public Health. 2017;107(11):1827-1829. https://doi.org/10.2105/AJPH.2017.304059
Powell D, Pacula R, Jacobson M. Do Medical Marijuana Laws Reduce Addictions and Deaths Relating to Pain Killers? NBER Working Paper. 2016;#21345
Hsu G, Kovacs B. Association between county level cannabis dispensary counts and opioid related mortality rates in the United States: panel data study. BMJ. 2021;372:m4957. https://doi.org/10.1136/bmj.m4957
Shover CL, Davis CS, Gordon SC, Humphreys K. Association between medical cannabis laws and opioid overdose mortality has reversed over time. Proc Natl Acad Sci U S A. 2019;116(26):12624-12626. https://doi.org/10.1073/pnas.1903434116
Dilley JA, Hitchcock L, McGroder N, Greto LA, Richardson SM. Community-level policy responses to state marijuana legalization in Washington State. Int J Drug Policy. 2017;42:102-108. https://doi.org/10.1016/j.drugpo.2017.02.010
Silver LD, Naprawa AZ, Padon AA. Assessment of Incorporation of Lessons From Tobacco Control in City and County Laws Regulating Legal Marijuana in California. JAMA Netw Open. 2020;3(6):e208393. https://doi.org/10.1001/jamanetworkopen.2020.8393
Bachhuber MA, Saloner B, Barry CL. What ecologic analyses cannot tell us about medical marijuana legalization and opioid pain medication mortality--reply. JAMA Internal Medicine. 2015;175(4):656-7. PMC Journal - In Process. https://doi.org/10.1001/jamainternmed.2014.8027
Finney JW, Humphreys K, Harris AH. What ecologic analyses cannot tell us about medical marijuana legalization and opioid pain medication mortality. JAMA Internal Medicine. 2015;175(4):655-6. PMC Journal - In Process. https://doi.org/10.1001/jamainternmed.2014.8006
Humphreys K, Saitz R. Should Physicians Recommend Replacing Opioids With Cannabis? JAMA. 2019;321(7):639-640. https://doi.org/10.1001/jama.2019.0077
Gorfinkel LR, Stohl M, Greenstein E, Aharonovich E, Olfson M, Hasin D. Is Cannabis being used as a substitute for non-medical opioids by adults with problem substance use in the United States? A within-person analysis. Addiction. 2021;116(5):1113-1121. https://doi.org/10.1111/add.15228
Campbell G, Hall WD, Peacock A, et al. Effect of cannabis use in people with chronic non-cancer pain prescribed opioids: findings from a 4-year prospective cohort study. Lancet Public Health. 2018;3(7):e341-e350. https://doi.org/10.1016/S2468-2667(18)30110-5
DiBenedetto DJ, Weed VF, Wawrzyniak KM, et al. The Association Between Cannabis Use and Aberrant Behaviors During Chronic Opioid Therapy for Chronic Pain. Pain Med. 2018;19(10):1997-2008. https://doi.org/10.1093/pm/pnx222
Olfson M, Wall MM, Liu SM, Blanco C. Cannabis Use and Risk of Prescription Opioid Use Disorder in the United States. Am J Psychiatry. 2018;175(1):47-53. https://doi.org/10.1176/appi.ajp.2017.17040413
NIDA. Colorado: Opioid-Involved Deaths and Related Harms. National Institute on Drug Abuse. Accessed 10/27/2020, https://www.drugabuse.gov/drug-topics/opioids/opioid-summaries-by-state/colorado-opioid-involved-deaths-related-harms
Brohl B, Kammerzell R, Koski W. Colorado Department of Revenue, Enforcement Division - Marijuana: Annual Update. CDOR. Accessed 10/27/2020, https://spl.cde.state.co.us/artemis/revserials/rev131internet/rev1312014internet.pdf
DEA. Controlled Substance Schedules. US Department of Justice; Drug Enforcement Administration. Accessed 2/17/2020, https://www.deadiversion.usdoj.gov/schedules/
CDC. Data Resources: Analyzing Prescription Data and Morphine Milligram Equivalents (MME). Centers for Disease Control and Prevention. 1/21/2020, https://www.cdc.gov/drugoverdose/resources/data.html
CDC. Data Resources: Analyzing Prescription Data and Morphine Milligram Equivalents (MME) Centers for Disease Control and Prevention. Accessed 6/26/2020, https://www.cdc.gov/drugoverdose/resources/data.html
OIG. HHS OIG Toolkits for Calculating Opioid Levels and Identifying Patients At Risk of Misuse or Overdose. 2018. https://oig.hhs.gov/oei/reports/oei-02-17-00560.asp
Colorado Hospital Association. CHA Databank. Colorado Hospital Association. Accessed January 26, 2017. http://www.cha.com/Member-Services/CHA-DATABANK.aspx
Gardner J. Two-stage differences in differences. Updated April 2021. https://jrgcmu.github.io/2sdd_current.pdf
Callaway B, Sant’Anna PHC. Difference-in-Differences with multiple time periods. J Econometrics. 2021;225(2):200-230. https://doi.org/10.1016/j.jeconom.2020.12.001
BLS. Local Area Unemployment Statistics. US Bureau of Labor Statistics. Accessed 10/29/2020, https://www.bls.gov/lau/
HRSA. Area Health Resources Files. Health Resources & Services Administration. Accessed June 25, 2020. https://data.hrsa.gov/topics/health-workforce/ahrf
Butts K, Gardner J. did2s: Two-Stage Difference-in-Differences. The R Journal. 2022 2022;
Freisthler B, Sumetsky N, Kranich C, Chadwick C, Mair C. Opioid Misuse and the Availability of Medical Marijuana Through Dispensaries. J Stud Alcohol Drugs. 2020;81(4):489-496.
Liang D, Shi Y. The Associations of Neighborhood Availability of Marijuana Dispensaries and DATA-2000 Waivered Providers with Hospital Stays Related to Opioids. Subst Use Misuse. 2019;54(14):2387-2399. https://doi.org/10.1080/10826084.2019.1650775
Lake S, Walsh Z, Kerr T, et al. Frequency of cannabis and illicit opioid use among people who use drugs and report chronic pain: A longitudinal analysis. PLoS Med. 2019;16(11):e1002967. https://doi.org/10.1371/journal.pmed.1002967
CDOR. Marijuana Sales Reports. Colorado Department of Revenue. Accessed June 25, 2020. https://www.colorado.gov/pacific/revenue/colorado-marijuana-sales-reports
Acknowledgements
We thank Lisa Jonsson, a Pardee RAND graduate student, for her assistance with cleaning the dispensary license data. We also thank Aaron Kofner for his assistance with descriptive analyses supporting this paper.
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium. The National Institute on Drug Abuse funded this study, grant number 7R01DA045051-03.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Question: What is the impact of cannabis availability on opioid prescribing and opioid-related hospital visits at the county level?
• Findings: This observational study using a quasi-experimental design of county-level claims data from two different sources in Colorado finds that recreational cannabis legalization was associated with statistically significant decreases in 30-day fills for opioids and opioid-related inpatient visits, but not ED visits nor total morphine equivalents per capita filled at pharmacies.
• Meaning: Our mixed findings provide weaker evidence than previous work using national claims data sources and state variation in access, suggesting that increasing access to cannabis may not be effective at reducing opioid prescribing or opioid-related hospital visits at a population level.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Buttorff, C., Wang, G.S., Wilks, A. et al. Impact of Recreational Cannabis Legalization on Opioid Prescribing and Opioid-Related Hospital Visits in Colorado: an Observational Study. J GEN INTERN MED 38, 2726–2733 (2023). https://doi.org/10.1007/s11606-023-08195-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08195-3