Abstract
Background
Obesity (body mass index [BMI]≥30kg/m2) among US adults has tripled over the past 45 years, but it is unclear how this population-level weight change has occurred.
Objective
We sought to identify distinct long-term BMI trajectories and examined associations with demographic and clinical characteristics.
Design
The design was latent trajectory modeling over 10 years of a retrospective cohort. Subgroups were identified via latent class growth mixture models, separately by sex. Weighted multinomial logistic regressions identified factors associated with subgroup membership.
Participants
Participants were a retrospective cohort of 292,331 males and 62,898 females enrolled in VA.
Main Measures
The main outcome measure was 6-month average VA-measured BMI over the course of 10 years. Additional electronic health record measures on demographic, clinical, and services utilization characteristics were also used to characterize latent trajectories.
Key Results
Four trajectories were identified for men and for women, corresponding to standard BMI categories “normal weight” (BMI <25), “overweight” (BMI 25-29.99), and “with obesity” (BMI ≥30): “normal weight” and increasing (males: 28.4%; females: 22.8%), “overweight” and increasing (36.4%; 35.6%), “with obesity” and increasing (33.6%; 40.0%), and “with obesity” and stable (males: 1.6%) or decreasing (females: 1.6%). Race, ethnicity, comorbidities, mental health diagnoses, and mental health service utilization discriminated among classes.
Conclusions
BMI in the 10 years following VA enrollment increased modestly. VA should continue prioritizing weight management interventions to the large number of veterans with obesity upon VA enrollment, because the majority remain with obesity.
Similar content being viewed by others
INTRODUCTION
The prevalence of obesity (body mass index [BMI]≥30 kg/m2) in US adults has increased from 13% in 1960 to 40% in 2016.1,2,3 Currently, 74% of US adults are classified as either overweight (BMI≥25 kg/m2) or with obesity, and nearly half of US adults are expected to have obesity by 2030.4 Rates of overweight or obesity are higher among veterans than among the general population, with 79% being classified as either overweight or with obesity.5,6,7 This increasing prevalence is especially problematic as obesity is associated with increased risk for numerous medical issues,8 including complications from COVID-19.9
National estimates of obesity prevalence have been generated using rotating cross-sectional cohorts to summarize changes over time at the population level.10,11 Since cohort composition changes with every 2- to 4-year measurement, these population estimates cannot characterize within-person changes of specific individuals over long timeframes. More recent research has estimated weight change in fixed cohorts of adults with repeated weight measures over time, and identified subgroups with persistently normal BMI, slowly increasing BMI, more rapidly increasing BMI, or persistent obesity.12 Most of these studies examined weight trends over only a few years, and lacked a meaningful reference point from which to anchor weight change. Moreover, most of this work evaluated weight change in non-veteran cohorts, yet veterans are a critically important population to understand given their higher rates of chronic health conditions that are associated with obesity.13,14
A notable exception was a study that examined 6-year weight trajectories among 16,656 veterans who enrolled in VA after serving in Iraq or Afghanistan.15 This study found five distinct weight trajectories. Approximately half of all veterans were classified with obesity upon military discharge, and higher initial BMI was associated with larger increases in BMI over the 6 years. A more robust investigation is needed to determine longer weight trends in veterans and explore demographic and clinical characteristics that may be associated with these trajectories.
To inform clinical care priorities, and address gaps in scientific evidence, this study characterized the natural history of post-military discharge BMI trajectories among veterans enrolled in VA care up to 10 years after VA enrollment, shortly after military discharge. We also compared key clinically meaningful and widely available characteristics between subgroups to help identify specific at-risk groups, which may guide future screening and intervention efforts.
METHODS
Data Sources
This retrospective cohort study examined several VA databases. The primary data source was the national Corporate Data Warehouse (CDW), which contains information on all encounters delivered in all VA facilities. To determine veterans’ discharge data from military service, we linked CDW data with the VETSNET file that describes veterans’ military service from the Veterans Benefits Administration.16
Study Sample
We identified all veterans who enrolled in VA for the first time between 10/01/1999–09/30/2018. We excluded veterans age <18 or >70 at the time of their first recorded BMI measure, or veterans with implausible BMIs. We further required veterans’ dates of VA enrollment to be within 90 days of military discharge and have at least one weight recorded during a VA visit any time between 21 days prior (to allow for discordant dates) and 365 days after VA enrollment to avoid including veterans whose immediate post-discharge weight changes would not be captured in VA data. We further limited the sample to veterans with least three 6-month time periods to accommodate flexible polynomial models of time in the longitudinal BMI analysis. For veterans meeting these inclusion criteria (292,331 male veterans with 2,445,754 6-month mean BMI measurements and 62,898 female veterans with 586,691 measurements [eFigure 1]), we tracked BMI in 6-month time intervals for up to 10 years (Fig. 1). In each sex-specific cohort, 20,000 veterans were randomly chosen for model exploration and the remainder were retained for model validation and association analysis.
Outcome Variable
BMI was constructed from all weight and height measures captured during health care encounters at VA facilities. We cleaned all weight measures using a multistep outlier-detection algorithm that examined the standard deviation of consecutively measured weights and weights measured on the same day,17 which excluded 4.8% of weight measurements. We then calculated the mean of cleaned weights within each 6-month interval from the date of VA enrollment or the first weight through the following 10 years. Height was defined as the modal value across all recorded measures.
Veteran Characteristics
Demographic characteristics were pulled from CDW or the linked VETSNET file. Veterans’ copayment exemption was obtained from priority group status at VA enrollment. VA healthcare use during 1-year post-VA enrollment was calculated using VA stop codes for the total number of primary care visits, specialty care visits, mental health visits, and whether they had at least one inpatient stay. Gagne comorbidity score was calculated from chronic health conditions within 1-year post-VA enrollment, and coded as 0, <0, or >0 (with scores above 0 representing greater disease burden; <0 scores are possible due to specific diagnoses).18 Mental health diagnoses (depression, anxiety, post-traumatic stress disorder [PTSD], schizophrenia, bipolar) and homelessness were also captured from diagnosis codes within 1-year post-VA enrollment.
Statistical Analyses
To identify distinct longitudinal BMI trends, we estimated latent class growth mixture models (GMM).19 In GMMs, unobserved heterogeneity in longitudinal measurements is captured by latent variables to identify different classes (k) of individuals whose BMI changes vary around different mean growth curves within each latent class.20 To allow for curvilinear developmental patterns of BMI over time, we specified linear, quadratic, and cubic slopes and adjusted for age at VA enrollment on the mean trajectory as a fixed effect. For computational feasibility, we randomly subsampled each sex-specific dataset to include 20,000 patients for initial latent subgroup estimation.
We conducted GMM analysis using the exploratory datasets to estimate the optimal number of classes (k) using a forward procedure with k=1 to 5 classes.21 The optimal model was determined by identifying increasing classes until at least one of the following criteria was met: (1) change in Bayesian Information Criterion <20,22 (2) average posterior class probability lower than 60% for at least one class, (3) the smallest class represented <0.5% of the sample, or (4) trajectories had similar BMIs. The quality of the classification was assessed by entropy.23 The resulting sex-specific, k-class solutions were then applied to the corresponding validation cohort to compute predicted values and posterior class probabilities for each individual. Individuals were assigned the class corresponding to the maximum posterior class probability.
In sensitivity analyses, we created five separate datasets of 20,000 randomly sampled veterans from the validation cohort for each sex, allowing veterans to be repeatedly sampled. Our validation procedure consisted of specifying (1) an unconstrained model, where only the number of classes was specified, and (2) a constrained model, where the number of classes and class-specific parameters were fixed to those generated by the final exploratory model.24 A likelihood ratio test (LRT) was then conducted to determine whether freeing the parameters in the unconstrained model significantly improved model fit in comparison to the constrained model.
To identify veteran characteristics associated with each trajectory in the validation sample, we fit weighted multinomial logistic (MNL) regressions with weights based on the posterior probability of class membership to account for the variability in class membership assignment.25 Veteran characteristics in the MNL regressions were selected based on clinical importance and expected associations with BMI.
Data construction and cleaning was performed in SAS Enterprise Guide (version 8.2; SAS Institute Inc.). All analyses were conducted in R (version 4.1.1) using the hlme function of the lcmm package.26 We followed the GRoLTS checklist for reporting latent trajectory studies.27 The MNL analysis was performed using the nnet package (version 7.3-16).28 This study was approved by the institutional review board at the Durham VA Health Care System.
RESULTS
Sample Characteristics
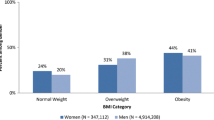
For both male and female veterans, average age at enrollment was around 30 years, and average first 6-month BMI was in the overweight range (Table 1). The majority were White race, previously served in the Army, and had weighted comorbidity scores of 0, at least one VA primary care visit in the first year of VA enrollment, and at least one mental health visit, but no VA specialty care visits. Mental health conditions were more common than medical condition diagnoses. However, no single mental health diagnosis was present in more than a quarter of patients with PTSD being the most common in both males (24.8%) and females (19.6%).
BMI Trajectories for Male and Female Veterans
For each sex, the optimal number of BMI trajectory subgroups in the exploratory cohort was 4. The four-subgroup solutions were retained over the five-subgroup solutions due to this subgroup solution failing to meet a decision criterion (clinical meaningfulness of a fifth subgroup was limited as its initial BMI and trajectory differed from another subgroup only slightly). Three trajectories were characterized by initial BMI (mean±SD) in the range of “normal” weight (22.0±2.0 representing 21.9% of females; 24.2±2.3 representing 27.5% of males), overweight (26.3±2.3 representing 36.4% of females; 28.9±2.2 representing 36.8% of males), and obesity (31.0±4.5 representing 40.2% of females; 32.6±4.6 representing 34.2% of males). For each of these groups, average BMI modestly increased linearly over time (Figs. 2 and 3, eTable 1).
Among males, a fourth class emerged, characterized by slightly higher initial obesity (initial mean BMI=35.5) and no significant time trend over the 10 years, representing only 1.6% of the cohort. Among females, the fourth class was characterized by initial obesity (initial mean BMI=34.1) that declined significantly over the 10-year period, such that mean BMI was lower than the “with obesity” and increasing subgroup’s mean BMI after year five, but represented only 1.6% of the cohort.
In sensitivity analyses, significant differences were found based on the LRT with 30 degrees of freedom (34 parameters in the unconstrained model vs. 4 parameters in the constrained model). Despite this finding, the estimated trajectories from the unconstrained models (eFigure 2 and eFigure 3) gave largely similar clinical interpretation, with slight differences in the sparsest classes at later timepoints. Plots in eFigure 2 and eFigure 3 were generated based on pooled estimates of the predictions and standard errors across the five repetitions of the validation procedure.
Demographic and Clinical Characteristics of BMI Subgroups
Demographic and clinical characteristics can be found in eTable 2 and eTable 3. The initially normal and increasing subgroup was the reference group for all analyses. In weighted MNL regression of the validation cohort (Figs. 4 and 5; eTables 4 and 5), Black race, Hispanic/Latino(a) ethnicity, being married, having a >0 Gagne score (compared to 0), and later VA enrollment were associated with higher odds of being in the “overweight and increasing” or “with obesity and increasing” classes. Having one or more mental health visit in the first year (e.g., 1–2 mental health visits; males: OR=1.24, 95% C.I. [1.18,1.31]; females: OR=1.51, 95% C.I. [1.33,1.73]), a depression diagnosis (males: OR=1.07, 95% C.I. [1.03,1.12]; females: OR=1.18, 95% C.I. [1.08,1.30]), and a bipolar diagnosis (males: OR=1.27, 95% C.I. [1.17,1.39]; females: OR=1.37, 95% C.I. [1.13,1.67]) were associated with higher odds of being in the “with obesity and increasing” class. An inpatient stay within 1 year of VA enrollment was the only factor uniquely associated with higher odds of being in the fourth, smaller “with obesity” and stable/decreasing class.
For male veterans, being in the Army or Marine Corps (vs. Air Force) and having one or more specialty care visit in the first year were associated with higher odds of being in the “overweight” and increasing or “with obesity” and increasing classes. Copay exemption status other than >50% SCD was associated with lower odds of being in the “overweight and increasing” or “with obesity and increasing” classes for male veterans only. For female veterans only, being in the Navy (vs. Air Force) was associated with higher odds of being in the “overweight and increasing” or “with obesity and increasing” classes.
DISCUSSION
In this study of recently discharged veterans who enrolled in VA, we identified four distinct BMI trajectories for each sex who were followed up to 10 years. For both cohorts, three trajectories evidenced modest linear increases in BMI throughout the 10 years. Results showing four distinct BMI trajectories are generally consistent with prior work in adults that identified three,29,30 five,31 or six32,33 distinct BMI trajectories. Importantly, 10-year trends were largely characterized by the initial BMI upon VA enrollment. This suggests that interventions addressing obesity should continue to be prioritized by VA for those whose BMIs are consistent with overweight and obesity, reinforcing current priorities for VA clinical operations.
We examined BMI trends shortly after military discharge because this represents a major individual life event, which can substantially shift individuals’ weight trajectories. Furthermore, veterans were required to have enrolled in VA, which provides integrated care to eligible veterans. VA is well-positioned to foster healthy transition to military life including weight management care because veterans, once eligible, are enrolled for life. Thus, insights gained from this population can inform the delivery of interventions early in veterans’ enrollment aimed at preventing or treating obesity. It is surprising that over one-third of veterans who recently discharged from the military had obesity, given the fitness requirements of military service. However, these proportions are commensurate with the growing proportions of active-duty service members with overweight/obesity.34 Given the tendency for post-discharge BMIs to increase, this finding puts more emphasis on the need for early intervention to mitigate later obesity-related health complications. Given the surprisingly high rates of veterans with obesity at a pivotal transition point in their lives, intervention delivered shortly after VA enrollment may be particularly timely as veterans are already having to search for new information and develop new routines in the next chapter of their lives.
Study results reinforce the importance of VA providing comprehensive weight management services using a patient-centered approach. In the VA/DoD Clinical Practice guidelines, the first-line treatment recommended is VA’s behavioral weight management program MOVE!, which targets weight loss by addressing physical activity and diet.35 However, only 2–12% of eligible patients participate in MOVE!, and may be less during the COVID-19 pandemic.36,37 These results indicate VA may want to prioritize outreach to veterans based on their initial BMI and early mental health care and diagnoses to maximize clinical benefits to these weight management programs. Outreach could include tailored educational materials, such as those within the VA Welcome Kit that specifically address the health risks of higher BMI and help veterans get started with weight management services available from VA.38 Additionally, higher prevalence of mental health diagnoses and comorbid chronic disease in the “overweight and increasing” and “with obesity and increasing” classes may help to inform the VA’s eligibility requirements and outreach efforts for other programs. One example is bariatric surgery, which has produced clinically significant and sustained weight loss, but is only available to certain veterans based of strict eligibility criteria.37
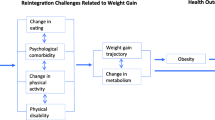
Several characteristics were associated with increasing BMI trajectories, indicating specific subgroups who should be prioritized for intervention. Characteristics associated with membership in the “overweight and increasing” and “with obesity and increasing” classes include Black race and Hispanic/Latino(a) ethnicity, greater mental health visits, and mental health diagnoses. These results align with previous investigations regarding the increased prevalence of overweight/obesity in Black and Hispanic/Latino(a) populations39 and individuals with mental health conditions.40 Note that our descriptive analysis focused on baseline variables and did not examine the association of time-varying characteristics such as events including incidence of cancer. Analyses of time-varying characteristics would require alternative approaches such as latent transition modeling and represents an area of future research.41
There are several potential reasons that mental health conditions could be associated with a higher likelihood of having overweight/obesity.42 First, there are known metabolic side effects of psychotropic medications.43 Additionally, psychiatric symptoms (e.g., anhedonia) can serve as barriers to physical activity and healthy eating, and can have direct metabolic effects (e.g., sleep disturbance). Veterans with mental health conditions could be prioritized for weight management services. However, this recommendation is complicated by evidence that some weight management programs, such as MOVE!, may be less effective for veterans with certain comorbid mental health conditions, such as PTSD.44
This study has several limitations. First, weights were limited to those in VA records and partitioned by biological sex, so results may not generalize to non-veterans, veterans not using VA healthcare, or veterans whose gender does not match their biological sex. Second, the study sample included veterans with a short period between military discharge and first measured weight in VA, consistent with the study aims. Results may not generalize to veterans who opt to enroll in VA later after military discharge. Specifically, our sample was younger, and a greater proportion were female, non-White, and Latino(a) than those excluded due to a later VA enrollment. While these results may not generalize to veterans who discharge from the military at older ages, the younger included sample represents a greater chance of impact over the course of the lifetime in early interventions upon VA enrollment. Third, due to data limitations, the observation window for baseline covariates overlapped BMI trends in the first year, limiting causal inference. Fourth, FDA-approved weight loss medications and medications where weight change is a side effect were not examined in descriptive analyses because initiation and dosage change over time. However, it should be noted that use of FDA-approved weight loss medications is rare in VA with less than 1% of our sample with any prescription fills. Finally, our sensitivity analyses showed statistically significant departures between the models constructed on the exploratory and validation cohorts. The primary differences between models occurred in later parts of the smallest class trajectories, likely due to sparsity of the data. Although even small departures between models can be detected with large sample sizes such as the present one, additional exploratory datasets for model-building may be beneficial to assess stability of our findings.
In conclusion, 10-year BMI trends were largely characterized by the initial value upon VA enrollment, which enables VA to prioritize veterans with obesity upon VA enrollment for weight management programs, especially if they are Black race or Hispanic/Latino(a) ethnicity, have mental health conditions, and/or mental health VA visits within the first year of VA enrollment.
Data Availability
Datasets cannot be made publicly available because they were generated from Veterans Affairs patients and cannot be sent in any disaggregated form outside the VA firewall.
References
Ogden CL, Carroll MD, Curtin LR, Mcdowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295(13):1549.
Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960–1994. Int J Obes. 1997;22(1):39-47.
Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007-2008 To 2015-2016. JAMA. 2018;319(16):1723-1725.
Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381(25):2440-2450.
Statistics NCfH. Obesity and overweight. https://www.cdc.gov/nchs/fastats/obesity-overweight.htm. Published 2017. Accessed 8/17/2021.
Koepsell TD, Forsberg CW, Littman AJ. Obesity, overweight, and weight control practices in U.S. veterans. Prev Med. 2009;48(3):267-271.
Breland JY, Phibbs CS, Hoggatt KJ, et al. The obesity epidemic in the veterans health administration: prevalence among key populations of women and men veterans. J Gen Intern Med. 2017;32(Suppl 1):11-17.
Kopelman PG. Obesity as a medical problem. Nature. 2000;404(6778):635-643.
Dietz W, Santos-Burgoa C. Obesity and its implications for Covid-19 mortality. Obesity. 2020;28(6):1005-1005.
Flegal KM. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293(15):1861.
Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA. 2012;307(5):491.
De Rubeis V, Andreacchi AT, Sharpe I, Griffith LE, Keown-Stoneman CDG, Anderson LN. Group-based trajectory modeling of body mass index and body size over the life course: a scoping review. Obes Sci Pract. 2020;7(1):100-128.
Hoerster KD, Lehavot K, Simpson T, Mcfall M, Reiber G, Nelson KM. Health and health behavior differences. Am J Prev Med. 2012;43(5):483-489.
Lehavot K, Hoerster KD, Nelson KM, Jakupcak M, Simpson TL. Health indicators for military, veteran, and civilian women. Am J Prev Med. 2012;42(5):473-480.
Rosenberger PH, Ning Y, Brandt C, Allore H, Haskell S. BMI trajectory groups in veterans of the Iraq and Afghanistan wars. Prev Med. 2011;53(3):149-154.
VA HSR RES 13-457. Va Informatics and Computing Infrastructure (Vinci). https://vincicentral.vinci.med.va.gov/.
Maciejewski ML, Arterburn DE, Van Scoyoc L, et al. Bariatric surgery and long-term durability of weight loss. JAMA Surg. 2016;151(11):1046-1055.
Gagne JJ, Glynn RJ, Avorn J, Levin R, Schneeweiss S. A combined comorbidity score predicted mortality in elderly patients better than existing scores. J Clin Epidemiol. 2011;64(7):749-759.
Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Modeling Multidiscip J. 2007;14(4):535-569.
Wells JCK. Sexual dimorphism of body composition. Best Pract Res Clin Endocrinol Metab. 2007;21(3):415-430.
Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Social Personal Psychol Compass. 2007;2(1):302-317.
Kim S-Y. Determining the number of latent classes in single- and multi-phase growth mixture models. Struct Equ Modeling. 2014;21(2):263-279.
Proust-Lima C, Séne M, Taylor JMG, Jacqmin-Gadda H. Joint latent class models for longitudinal and time-to-event data: a review. Stat Methods Med Res. 2014;23(1):74-90.
Wang M, Bodner TE. Growth mixture modeling. Organ Res Methods. 2007;10(4):635-656.
Clark SL, Muthén B. Relating latent class analysis results to variables not included in the analysis https://www.statmodel.com/download/relatinglca.pdf. Published 2009. Accessed.
Proust-Lima C, Philipps V, Liquet B. Estimation of extended mixed models using latent classes and latent processes: the R Package lcmm. J Stat Softw. 2017;78(2).
van de Schoot R, Sijbrandij M, Winter SD, Depaoli S, Vermunt JK. The GRoLTS-Checklist: guidelines for reporting on latent trajectory studies. Struct Equ Model Multidiscip J. 2016;24(3):451-467.
Venables WN, Ripley BD. Time series analysis. In. Modern Applied Statistics with S: Springer New York; 2002:387-418.
Dhana K, van Rosmalen J, Vistisen D, et al. Trajectories of body mass index before the diagnosis of cardiovascular disease: a latent class trajectory analysis. Eur J Epidemiol. 2016;31(6):583-592.
Hoekstra TB-L C, Koppes LL, Twisk JW. Developmental trajectories of body mass index throughout the life course: an application of latent class growth (mixture) modelling. Longitud Life Course Stud. 2011;2(3).
Paynter L, Koehler E, Howard AG, Herring AH, Gordon-Larsen P. Characterizing long-term patterns of weight change in china using latent class trajectory modeling. PLoS ONE. 2015;10(2):E0116190-E0116190.
Zheng H, Tumin D, Qian Z. Obesity and mortality risk: new findings from body mass index trajectories. Am J Epidemiol. 2013;178(11):1591-1599.
Tanofsky-Kraff M, Sbrocco T, Theim KR, et al. Obesity and the US military family. Obesity (Silver Spring). 2013;21(11):2205-2220.
Maciejewski ML, Shepherd-Banigan M, Raffa SD, Weidenbacher HJ. Systematic review of behavioral weight management program MOVE! for veterans. Am J Prev Med. 2018;54(5):704-714.
Hoerster KD, Gray K, Raffa SD. Weight management and healthy lifestyles. JAMA Intern Med. 2020;180(10):1403.
Gray KE, Hoerster KD, Spohr SA, Breland JY, Raffa SD. National Veterans Health Administration MOVE! Weight management program participation during the Covid-19 pandemic. Prev Chronic Dis. 2022;19.
Atkins D. Improving weight management among veterans. J Gen Intern Med. 2017;32(Suppl 1):1-3.
Print Out Your VA Welcome Kit | Veterans Affairs. @Deptvetaffairs. https://www.va.gov/welcome-kit/. Published 2022. Updated 2022-07-18. Accessed.
Pan L, Galuska DA, Sherry B, et al. Differences in prevalence of obesity among Black, White, and Hispanic adults - United States, 2006-2008. Morb Mortal Wkly Rep. 2009;58:740-744.
Scott KM, Bruffaerts R, Simon GE, et al. Obesity and mental disorders in the general population: results from the world mental health surveys. Int J Obes (Lond). 2008;32(1):192-200.
Allison DB, Newcomer JW, Dunn AL, et al. Obesity among those with mental disorders. Am J Prev Med. 2009;36(4):341-350.
Hoerster KDY, Alexander S. Improving diet, activity and weight. In: Corrigan PWB, Sonya L, Ed. Health and Wellness in People Living with Serious Mental Illness. American Psychiatric Association Publishing; 2021:267.
Hoerster KD, Lai Z, Goodrich DE, et al. Weight loss after participation in a National VA Weight Management Program among veterans with or without PTSD. Psychiatric Serv. 2014;65(11):1385-1388.
Hoerster KD, Tanksley L, Sulayman N, et al. Testing A tailored weight management program for veterans with PTSD: the MOVE! + UP randomized controlled trial. Contemp Clin Trials. 2021;107:106487.
Acknowledgements
The authors thank Natalie A. Bontrager for extensive editorial assistance in preparing this paper. The authors also thank the editor and two reviewers for helpful comments.
Funding
This study was funded by award IIR 18-019 from the Veterans Health Administration Office of Research Development. Dr. Blalock, Dr. Pura, Ms. Stechuchak, Dr. Dennis, Dr. Maciejewski, Dr. Smith, and Dr. Hung were supported by award CIN 13-410 from Veterans Health Administration Health Services Research and Development. Dr. Blalock was also supported by award CDA 19-035 from the Veterans Health Administration Office of Research Development. Dr. Maciejewski was also supported by a Research Career Scientist award RCS 10-391 from the VA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Blalock receives consulting fees from Eating Recovery Center. All authors declare no conflict of interest.
Disclaimer
The Health Services Research and Development Service, Department of Veterans Affairs, had no role in the design, conduct, collection, management, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript. The opinions expressed are those of the authors and not necessarily those of the Department of Veterans Affairs, the United States Government, Duke University, and the University of Washington.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 266 kb)
Rights and permissions
About this article
Cite this article
Blalock, D.V., Pura, J.A., Stechuchak, K.M. et al. BMI Trends for Veterans Up to 10 Years After VA Enrollment Following Military Discharge. J GEN INTERN MED 38, 1423–1430 (2023). https://doi.org/10.1007/s11606-022-07818-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07818-5