Abstract
Background
In the USA, nearly 40% of adults ≥ 20 years have a body mass index (BMI) ≥ 30, and 11% of households are reported as food insecure. In adults, evidence shows women are more likely than men to be food insecure. Among adults with food insecurity, differences in BMI exist between men and women with women reporting higher BMI. Factors associated with this difference in BMI between genders are less understood.
Objective
The aim of this study was to assess gender differences in the relationship between food insecurity and BMI.
Design
Hierarchical models were analyzed using a general linear model by entering covariates sequentially in blocks (demographics, lifestyle behaviors, comorbidities, and dietary variables) and stratified by gender.
Participants
The sample included 25,567 adults in the USA from the National Health and Nutrition Examination Survey (NHANES), 2005–2014.
Main Measures
The dependent variable was BMI, and food insecurity was the primary predictor.
Key Results
Approximately 51% of the sample was women. Food insecure women were significantly more likely to have higher BMI compared to food secure women in the fully adjusted model after controlling for demographics (β = 1.79; 95% CI 1.17, 2.41); demographic and lifestyle factors (β = 1.79; 95% CI 1.19, 2.38); demographic, lifestyle, and comorbidities (β = 1.21; 95% CI 0.65, 1.77); and demographic, lifestyle, comorbidities, and dietary variables (β = 1.23; 95% CI 0.67, 1.79). There were no significant associations between food insecure and food secure men in the fully adjusted model variables (β = 0.36; 95% CI − 0.26, 0.98).
Conclusion
In this sample of adults, food insecurity was significantly associated with higher BMI among women after adjusting for demographics, lifestyle factors, comorbidities, and dietary variables. This difference was not observed among men. More research is necessary to understand this relationship among women.
Similar content being viewed by others
INTRODUCTION
Body mass index (BMI) is a well-known measure for tracking weight and an important indicator of increased adiposity, with those having a BMI ≥ 30 considered obese.1 In 2016, approximately 37% of adults in the USA aged 20 years and older were obese.2 Approximately 41% of women have a BMI ≥ 30 compared to 34% of men.2 Without intervention, it is projected that 51% of adults will be obese by 2030.3 Obesity is a leading risk factor for chronic disease,4 with obese adults having higher rates of type 2 diabetes, hypertension, stroke, cancer, myocardial infarction, and depression.5,6 Finally, obesity carries significant financial burden as it is associated with a 36% increase in healthcare costs and lowered earning potential.7
The prevalence of obesity is further increased among food insecure adults.8,9 Food insecurity is defined as being uncertain of having or the inability to acquire enough food to meet nutritional needs because of insufficient money or other food-related resources.10 Since 2018, 11% of US households are estimated to be food insecure.10 Among adults, households with children, with lower incomes, and with Non-Hispanic Black (NHB) or Hispanic heads of household have higher rates of food insecurity than the national average.11 Similarly, in adults under the age of 65, food insecurity is more prevalent among NHBs and Hispanics.12 Furthermore, food insecurity is more prevalent in adult women than adult men, where evidence shows women are more likely to be overweight or obese compared to men.12,13,14 Although the association between food insecurity and increased BMI in women has been shown in prior studies,12,13,14 the mechanism underlying this disparity remains unclear.15
Because of the increasing prevalence of obesity in our society and evidence supporting higher BMI and poorer outcomes in food insecure women, it is important to understand how the relationship between obesity and food insecurity differs both between and within gender groups. While previous studies have focused on understanding the relationship between being overweight and food insecure13,14 particularly among women,12,13,14,16 there is a lack of literature looking into the factors associated with the relationship between obesity and food insecurity by gender and BMI level in adults. Evidence showing women to have poorer outcomes related to obesity and food insecurity, both independently and collectively, warrants additional research to understand this relationship. In addition, prior studies in this area have limited their investigations to including only covariates such as demographic variables in the analysis,13,14,15 within smaller subgroups of the US population.15,16 However, our study aims to explore a variety of covariates consisting of demographic, lifestyle, comorbidity, and dietary variables within a large, nationally representative adult population to further investigate this relationship. Therefore, this study aimed to understand gender differences in the relationship between food insecurity and BMI in a nationally representative sample of adults from the USA.
METHODS
Data Source and Study Population
The National Health and Nutrition Examination Survey (NHANES) is a series of cross-sectional surveys that were designed to estimate the health and nutritional status of adults and children in the USA. The NHANES interview includes demographic, socioeconomic, dietary, and health-related questions. Findings from NHANES can be used to determine the prevalence of major diseases and risk factors for diseases. Information can also be used to assess nutritional status and its association with health promotion and disease prevention.
This study used five cycles of continuous NHANES data between 2005 and 2014, for individuals 20 years of age and older, who completed both the dietary interview and the physical examination. In total, 26,091 participants were selected. There are 321 participants without BMI information and 203 without food security information, so the sample has 25,567 valid for analysis.
Outcomes
The primary outcome of interest was body mass index (BMI). We analyzed BMI as continuous.
Main Predictor
The primary predictor for this analysis was food insecurity. Eighteen Food Security Survey Module (FSSM) questions were asked of households with children under the age of 18 years. Ten questions were asked of households without children. Four response levels were created based on the number of affirmative responses for those questions. Household food security category: 1 = household full food security: no affirmative response in any of these items; 2 = household marginal food security: 1–2 affirmative responses; 3 = household low food security: 3–5 affirmative responses for household without children under the age of 18 and 3–7 affirmative responses for household with children; 4 = household very low food security: 6–10 affirmative responses for household without children under the age of 18 and 8–18 affirmative responses for household with children. Food insecurity was treated in two ways: as a 4-category variable as defined by NHANES above and as a 2-category variable by further dichotomizing the four categories into two distinctive categories: food security (categories 1 and 2) and food insecurity (categories 3 and 4).
Covariates
Covariates included demographic, lifestyle, comorbidity, and dietary intake variables.
Demographic variables included age (grouped as 20–34 years; 35–49 years; 50–64 years; and 65+ years), race/ethnicity (grouped as non-Hispanic White; non-Hispanic Black; Hispanic; and other minority), education (dichotomized as high school or below and college or above), marital status (dichotomized as married or not married), ratio of family income to poverty (dichotomized as 130% and less of poverty level and above 130% of poverty level), and insurance status (dichotomized as covered or not covered by insurance). These variables have been implicated as potential mediators impacting the relationship between food insecurity and obesity among adults.12
Lifestyle variables included physical activity (grouped as none, moderate, and vigorous), smoking status (grouped as non-smoker, former smoker, and current smoker), and drinking status (grouped as non-drinker, moderate drinker, and above-moderate drinker). These variables have been noted in the literature to be related to increased body fat in adult populations.17,18
Comorbidities included physical and mental health conditions. Physical comorbidities included the following diagnosed medical conditions: diabetes, hypertension, stroke, heart disease (congestive heart failure, coronary heart disease, angina, heart attack), lung-related disease (asthma, emphysema, chronic bronchitis), thyroid problem, arthritis, and cancer. Several comorbidities have been linked to increased body mass index and obesity among adults.19,20,21,22,23,24,25 Physical comorbidities were grouped by the count equal to 0, 1, 2, 3, and ≥ 4. Mental comorbidity included depression, which was measured by the Patient Health Questionnaire (PHQ), a nine-item instrument. Depression was defined as PHQ-9 score between 10 and 27, and a PHQ-9 score between 0 and 9 was defined as no depression. Depression has been linked to an increase in body mass index in adults, according to a study by Wiltink et al.26
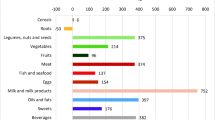
Dietary intake variables included total energy intake (kcal), total sugar intake (gm), and total carbohydrate intake (gm) during 24-h dietary recall.
Statistical Analysis
Data analysis was performed using SAS version 9.4 (SAS Institute). The SURVEYFREQ, SURVEYMEANS, SURVEYREG, and SURVEYLOGISTIC procedures in SAS were used to represent the US population and account for the complex survey sample design, including designs with stratification, clustering, and unequal weighting. Dietary day 1 sample weight was used.
The primary analytical goal was to explore the association between BMI and food insecurity stratified by gender. First, BMI was modeled as continuous, and survey general linear regression models were fitted to assess the relationship between food insecurity and BMI level. We first ran univariate survey general linear models (GLM) for food insecurity, as well as stratified by gender through domain statement, then developed four multivariable survey GLM in hierarchical sequence: (1) adjusted for all demographic variables; (2) adjusted for demographic and lifestyle variables; (3) adjusted for demographic, lifestyle, and comorbidity variables; and (4) adjusted for demographic, lifestyle, comorbidity, and dietary intake variables. Food insecurity was treated as a 4-category variable and as a 2-category variable separately for all above regression analyses. All p values were 2-sided, and p < 0.05 was considered statistically significant.
RESULTS
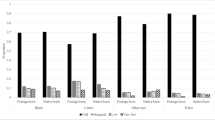
Table 1 shows the sample characteristics by gender for this cohort of adults. Fifty-one percent of the sample was women. Half of the sample was below the age of 50. Most men (45%) and women (46%) were non-Hispanic Whites. A majority of the sample was above 130% of the poverty level (67%), was covered by insurance (77%), were non-smokers (54%), were moderate drinkers (58%), and had none or at least one comorbidity (60%). Thirty-seven percent of the sample had a BMI of 30 or more, and 18% of the sample was food insecure.
Among this sample of adults, more women (41%) were obese than men (33%) (p < 0.001), and more women reported being food insecure compared to men (19% vs. 18%; p = 0.003). More men were married (57% vs. 47%; p < 0.001), physically active (69% vs. 59%; p < 0.001), smokers (25% vs. 18%, p < 0.001), and drinkers (84% vs. 61%, p < 0.001) compared to women. More women had income described as 130% and less of the poverty level (34% vs. 31%; p < 0.001) and were covered by insurance (79% vs. 74%; p < 0.001), non-smokers (63% vs. 45%; p < 0.001), non-drinkers (40% vs. 16%; p < 0.001), and depressed (11% vs. 6%; p < 0.001) compared to men. Women had a higher education level (p < 0.001), more comorbidities (p < 0.001), and a significantly higher energy (p < 0.001), total sugar (p < 0.001), and carbohydrate intake (p < 0.001) during 24-h dietary recall than men.
Table 2 shows unadjusted and adjusted linear regression models for the relationship between BMI and food insecurity by gender. In the unadjusted model (model 1), BMI was significantly higher in food insecure women compared to food secure women (β = 2.51; 95% confidence interval (CI) 1.96–3.07). When adjusting for demographic variables (model 2), BMI in food insecure women was statistically higher than the BMI in food secure women (β = 1.79; 95% CI 1.17–2.41). Similarly, when adjusting for demographic and lifestyle variables (model 3) and demographic, lifestyle, and comorbidity variables (model 4), the BMI in food insecure women was statistically higher than the BMI among food secure women (β = 1.79; 95% CI 1.19–2.38 and β = 1.21; 95% CI 0.65–1.77, respectively). In the fully adjusted model for demographic, lifestyle, comorbidity, and dietary variables, BMI in food insecure women was statistically higher than the BMI among food secure women (β = 1.23; CI 0.67–1.79). There were no statistically significant differences in BMI among food insecure men compared to food-men in any of the models.
Table 3 shows the unadjusted and adjusted linear regression models for BMI outcomes between men and women by stratified food security levels. Women with marginal (β =1.55; CI 1.03–2.07), low (β = 2.49; CI 1.84–3.13), and very low (β = 2.97; CI 1.98–3.95) food security had higher BMI in the unadjusted model (model 1) compared to women with full food security. When adjusting for demographics (model 2), BMI in marginal food secure women (β = 1.15; CI − 0.61 to 1.69), low food secure women (β = 1.85; CI 1.07–2.63), and very low food secure women (β = 2.29; CI 1.27–3.31) was statistically higher than food secure women. When adjusting for demographics and lifestyle variables (model 3), BMI in marginal food secure women (β = 1.28; CI 0.72–1.85), low food secure women (β = 1.84; CI 1.08–2.59), and very low food secure women (β = 2.38; CI 1.46–3.30) was statistically higher than in food secure women. When adjusting for demographic, lifestyle, and comorbidity variables (model 4), BMI in marginal food secure women (β = 0.91; CI 0.39–1.42), low food secure women (β = 1.38; CI 0.65–2.10), and very low food secure women (β = 1.43; CI 0.51–2.35) was statistically higher than that of food secure women. In the fully adjusted model for demographic, lifestyle, comorbidity, and dietary variables (model 5), BMI in marginal food secure women (β = 0.93; CI 0.42–1.45), low food secure women (β = 1.40; CI 0.68–2.12), and very low food secure women (β = 1.46; CI 0.53–2.37) was statistically higher than that of food secure women. Food insecure men did not show a significant difference in BMI compared to food secure men at any of the food security levels across all models.
DISCUSSION
In this cross-sectional study of a sample of adults from the USA, significant differences were observed in the relationship between BMI and food insecurity by gender. In the unadjusted model, food insecure women were significantly more likely to have a higher BMI compared to food secure women. Significance for this relationship remained after adjusting for demographics alone; for demographic and lifestyle factors; for demographic, lifestyle factors, and comorbidities; and in the fully adjusted model for demographic, lifestyle variables, comorbidities, and dietary variables. No significant findings were observed in the relationship between food insecure and food secure men. When stratified by food security status, women who reported marginal, low, and very low food security had a significantly higher BMI compared to women with full food security. There were no significant relationships between stratified food security status and BMI among men. These findings suggest there is a relationship between BMI and food security status, particularly for women, and that an understanding of the factors associated with this significant relationship is warranted.
In this sample, we found a significant relationship between BMI and food insecurity for women, but not for men. This disparity by gender has been demonstrated previously in the literature13,15,27,28,29,30; however, gaps remain in understanding the factors associated with the difference.9,13,28,31 Several theories for this difference between women and men have been hypothesized, with focus on race/ethnicity, pregnancy status, and food stamp participation.15,32 Among women, it has been suggested that this relationship may be associated with non-Hispanic White, Hispanic,13,29,31,33 non-Hispanic Black, and Asian race/ethnicity, but this is not the same for men.13,33 While the influence race and ethnicity have on the relationship between food insecurity and BMI is unknown, it is hypothesized that genetic factors contribute to increased adiposity, which may influence the relationship between food insecurity and BMI.24 Additionally, pregnancy status has been noted as a factor among women and would not impact the relationship between food insecurity and BMI in men.12 Most notably, pregravid and postgravid severe obesity and gestational diabetes have shown associations between food insecurity status and BMI.12 In contrast, weight gain has not always been shown to influence the relationship between food insecurity and BMI.12,31 In our analysis, we did not assess the relationship between pregnancy status, food insecurity, and BMI; therefore, we are unable to offer new evidence on this relationship. Finally, Dinour et al. proposed that food stamp participation, which would likely influence the lived experiences of households led by women in comparison to men, leads to a binge-starvation cycle, contributing to the difference by gender.9
In this sample, we found women with food insecurity had significantly higher levels of BMI compared to women without food insecurity. Like our findings, the literature has shown that food insecure women have a higher incidence of obesity compared to food secure women.12,13,27,28,29,30 One study concluded that the prevalence of overweight and obese status in women exists regardless of race or ethnicity, with increased odds of higher BMI among food insecure non-Hispanic White and Hispanic women.13 In two studies, after adjusting for socioeconomic, demographic, and lifestyle variables, food insecure women had increased likelihood of overweight BMI compared to food secure women.12,30 Alternatively, it has been suggested that by stratifying food insecurity by mild, moderate, and severe, overweight BMI is only seen in mild food insecure women,34 or most strongly correlated with mild to moderate food insecure compared to severely food insecure women.19,35 Hanson et al. suggest that the prevalence of obesity among those with mild to moderate food insecurity could be due to obese women perceiving their food insecurity status as more severe than non-obese women because of the lack of quality and prevalence of food in their lives.35,36 Mild to moderate food security may lead to diets high in inexpensive, lower-quality foods until the food insecurity level further increases to a point where the individual can no longer provide enough food to sustain a high body weight.37
In our study, an additional finding was that there were no significant relationships between food insecurity and BMI among men, and our findings are supported by previous literature.12,13,27 This finding may be due to gender differences in body composition and the higher retention of fat in women than men.38 In addition, evidence suggests men exhibit different coping skills when faced with stressors, so coping mechanisms that result in increased weight gain and BMI may be less.39 For example, men are more likely to act in response to stress, such as by decreasing food intake when food is scarce, leading to lower calorie intake.40
Our study was uniquely designed to assess the factors associated with the relationship between food insecurity and BMI and differs from prior studies by using sophisticated methodology to assess whether demographic characteristics, lifestyle behaviors, comorbidities, and dietary factors were associated with the relationship between food insecurity and BMI by gender. In our study, the relationship between food insecurity and BMI remained significant for women when adjusting for covariates in each model; these same relationships were not significant for men. Given that adjustment for all covariates, entered sequentially in blocks, did not alter significance among women, our findings suggest these variables were not associated with the relationship between food insecurity and BMI among women. Researchers have agreed that there is an immense need for more studies regarding the paradoxical relationship between food insecurity and obesity in women given the disease burden caused by obesity.12,13,27,29,39 Despite an increase in knowledge concerning the importance of a healthy diet, women with food insecurity still exhibit increased BMI, while men and food secure women do not. Because obesity prevalence is rising in the USA, it is important that we understand the factors associated with increased BMI among food insecure women.
While a major strength of our paper is the large sample of a nationally representative cohort of adults from the USA, limitations of this study need to be addressed. First, we were limited by conducting a cross-sectional study; therefore, we were unable to determine causality. Second, by not utilizing a longitudinal method, we cannot speak to how the effects of food insecurity status affect individuals’ body weights over time. Third, we did not assess for some cofounders, such as access to care, social support, diet education, food stamp use, pregnancy status, and availability of resources, which may have influenced the study findings. Fourth, given that NHANES is a dataset that is based on self-reported data, we must acknowledge that reporting of chronic conditions and dietary information may be biased and thus difficult to interpret.41,42 In addition, the limited length of time in which dietary intake was measured may not accurately describe an individual’s typical intake.
CONCLUSIONS
In this cross-sectional study of a nationally representative sample of adults, gender differences in the relationship between food insecurity and BMI were observed, particularly among women. Women with any level of food insecurity had a significantly higher BMI than women with food security after adjusting for relevant covariates. These results indicate more research is necessary to understand this relationship among women. Future research should focus on identifying the underlying mechanisms associated with the observed differences in BMI among women with food insecurity. In addition, women should be informed about the increased risk for obesity that is associated with food insecurity status and provided education concerning strategies to maintain a healthy BMI through a variety of lifestyle changes to avoid adverse outcomes.
References
Pi-Sunyer FX. Obesity: criteria and classification. Proc Nutr Soc. 2000;12:4:505-09.
NHANES questionnaires, datasets, and related documentation. Available at: https://www.cdc.gov/nchs/nhanes/Default.aspx. Accessed October 1, 2019.
Finkelstein EA, Khavjou OA, Thompson H, et al. Obesity and severe obesity forecasts through 2030. Am J Prev Med. 2012;42:6:563-570.
Haslam DW, James WP. Obesity. Lancet. 2005;366:9492:1197-209.
Cawley J, Meterhoefer C. The medical care costs of obesity: an instrumental variables approach. J Health Econ. 2012;31:1:219-30.
Bhaskaran K, Douglas I, Forbes H, Dos-Santos-Silva I, Leon DA, Smeeth L. Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5·24 million UK adults. Lancet. 2014;384:9945:755-65.
Apovian CM. Obesity: Definition, comorbidities, causes and burden. Am J Manage Care. 2016;22:7:176-185.
Ahn S, Smith ML, Hendricks M, Ory MG. Associations of food insecurity with body mass index among baby boomers and older adults. Food Secur. 2014;6:3:423-433.
Dinour LM, Bergen D, Ming-Chin Y. The food insecurity-obesity paradox: a review of the literature and the role food stamps may play. J Am Diet Assoc. 2007;107:11:1952-61.
USDA ERS – Key Statistics & Graphics. Available at: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/key-statistics-graphics/#foodsecure Accessed October 1, 2019.
Brown AGM, Esposito LE, Fisher RA, Nicastro HL, Tabor DC, Walker JR. Food insecurity and obesity: research gaps, opportunities, and challenges. Transl Behav Med. 2019;9:5:980-87.
Franklin B, Jones A, Love D, Puckett S, Macklin J, White-Means S. Exploring mediators of food insecurity and obesity: a review of recent literature. J Commun Healh. 2012;37:1:253-64.
Hernandez DC, Reesor LM, Murillo R. Food insecurity and adult overweight/obesity: gender and race/ethnic disparities. Appetite. 2017;117:373-78.
Olson CM. Nutrition and health outcomes associated with food insecurity and hunger. J Nutr. 1999;129:2:521S-524S.
Dhurandhar EJ. The food-insecurity obesity paradox: a resource scarcity hypothesis. Physiol Behav. 2016;162:88-92.
Walker RJ, Garacci E, Dawsom AZ, Williams JS, Ozieh M, Egede LE. Trends in food insecurity in the United States from 2011-2017: disparities by age, sex, race/ethnicity, and income. Popul Health Manag. 2021;24:4:496-501.
Raistenskis J, Sidlauskiene A, Strukcinskiene B, Baysal SU, Buckus R. Physical activity and physical fitness in obese, overweight and normal-weight children. Turk J Med Sci. 2016;46:2:443-450.
Traversy G, Chaput J. Alcohol consumption and obesity: an update. Curr Obes Rep. 2015;4:1:122-130.
Drøyvold WB, Midthjell K, Nilsen TIL, Holmen J. Change in body mass index and its impact on blood pressure: a prospective population study. Int J Obesity (London). 2005;29:6:650-655.
Maggio CA, Pi-Sunyer FX. Obesity and type 2 diabetes. Endocrinol Metab Clin North Am. 2003;32:4:805-822.
Jokinen, E. Obesity and cardiovascular disease. Minerva Pediatr. 2015;67:1:25-32.
Dixon AE, Peters U. The effect of obesity on lung function. Expert Rev Respir Med. 2018;12:9:755-767.
Pearce, EN. Thyroid hormone and obesity. Curr Opin Endocrinol Diabetes Obes. 2012;19:5:408-13.
Moroni L, Farina N, Dagna L. Obesity and its role in the management of rheumatoid and psoriatic arthritis. Clin Rheumatol. 2020;39:4:1039-1047.
Kolb R, Sutterwala FS, Zhang W. Obesity and cancer: inflammation bridges the two. Curr Opin Pharmacol. 2016;29:77-89.
Wiltink J, Michal M, Wild PS, et al. Associations between depression and different measures of obesity (BMI, WC, WHtR, WHR). BMC Psychiatry. 2013;13:223.
Sullivan AF, Clark S, Pallin DJ, Camargo CA. Food security, health, and medication expenditures of emergency department patients. J Emerg Med. 2010;38:4:524-48.
Gooding HC, Walls CE, Richmond TK. Food insecurity and increased BMI in young adult women. Obesity. 2012;20:9:1896-901.
Townsend MS, Peerson J, Love B, Achterberg C, Murphy SP. Food insecurity is positively related to overweight in women. J Nutr. 2001;131:6:1738-45.
Jones SJ, Frongillo EA. The modifying effects of food stamp program participation on the relation between food insecurity and weight change in women. J Nutr. 2006;136:4:1091-94.
Olson CM, Strawderman MS. The relationship between food insecurity and obesity in rural childbearing women. J Rural Health. 2008;24:1:60-66.
Shi H, Clegg DJ. Sex differences in the regulation of body weight. Physiol Behav. 2009;97:2:199-204.
Adams EJ, Grummer-Strawn L, Chavez G. Food insecurity is associated with increased risk of obesity in California women. J Nutr. 2003;133:4:1070-74.
Institute for Research on Poverty. Nutritional consequences of food insecurity in a rural New York state county. Discussion Paper no. 1120-97. Available at: https://www.irp.wisc.edu/publications/dps/pdfs/dp112097.pdf. Accessed: July 14, 2022.
Kaiser LL, Townsend MS, Melgar-Quinonez HR, Fuji ML, Crawford PB. Choice of instrument influences relations between food insecurity and obesity in Latino women. Am J Clin Nutr. 2004;80:5:1372-78.
Olson, CM. Food insecurity in women: a recipe for unhealthy trade-offs. Top Clin Nutr. 2005;20:4:321-28.
Smith EM, Colon-Ramos U, Pinard CA, Yaroch AL. Household food insecurity as a determinant of overweight and obesity among low-income Hispanic subgroups: data from the 2011-2012 California Health Interview Survey. Appetite. 2016;97:37-42.
Harris GK, Baer DJ. Gender differences in body fat utilization during weight gain, loss, or maintenance. Phytopharma Obes Treat. 2007:139-244.
Hanson KL, Sobal J, Frongillo EA. Gender and marital status clarify associations between food insecurity and body weight. J Nutr. 2007;137:6:1460-65.
Hobfoll SE, Cameron RP, Chapman HA, Gallagher RW. Social support and social coping in couples. Handbook of Social Support and the Family. New York: Springer Science; 1996:413-433.
Beltrán S, Pharel M, Montgomery CT, López-Hinojosa IJ, Arenas DJ, DeLisser HM. Food insecurity and hypertension: a systematic review and meta-analysis. PLoS One. 2020;15:11:e0241628.
Beltrán S, Arenas DJ, Pharel M, Montgomery C, Lopez-Hinojosa I, DeLisser HM. Food insecurity, type 2 diabetes, and hyperglycaemia: a systemic review and meta-analysis. Endocrinol Diabetes Metab. 2022;5:1:e00315.
Funding
Effort for this study partially supported by the National Institute of Diabetes and Digestive and Kidney Diseases K24DK093699 (PI: Leonard E. Egede, MD, MS), R01DK118038 (PI: Leonard E. Egede, MD, MS), R01DK120861 (PI: Leonard E. Egede, MD, MS), and R21DK123720 (PI: Joni S. Williams, MD, MPH).
Author information
Authors and Affiliations
Contributions
EK, JSW, and LEE designed the study. LEE and EG acquired and analyzed the data. EK, JSW, and LEE developed the analyses, interpreted the data, and critically revised the manuscript for important intellectual content. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 45 kb)
Rights and permissions
About this article
Cite this article
Koller, E.C., Egede, L.E., Garacci, E. et al. Gender Differences in the Relationship Between Food Insecurity and Body Mass Index Among Adults in the USA. J GEN INTERN MED 37, 4202–4208 (2022). https://doi.org/10.1007/s11606-022-07714-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07714-y