Abstract
Background
Many severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) positive patients take commonly prescribed medications with properties which may affect mortality.
Objective
Assess if common medications postulated to affect clinical outcomes are associated with mortality in SARS-CoV-2 positive patients in the Veterans Health Administration (VHA).
Design
Observational national cohort analysis.
Participants
Consecutive 26,508 SARS-CoV-2 positive Veterans (7% of 399,290 tested from March 1 to September 10, 2020) constitute the study cohort.
Main Measures
The primary outcome was 30-day mortality from the first positive SARS-CoV-2 test date. In patients receiving medications or drug pairs within 2 weeks post-SARS-CoV-2 positive test, 30-day mortality was estimated as relative risk (RR) on the log-binomial scale or using multinomial models with and without adjusting for covariates.
Key Results
The 26,508 SARS-CoV-2 positive patients were predominantly male (89%) and White (59%), and 82% were overweight/obese. Medications associated with decreased 30-day mortality risk included the following: metformin (aRR, 0.33; 95% CI, 0.25–0.43), colchicine, angiotensin-converting-enzyme inhibitors (ACEi), angiotensin II receptor blockers, statins, vitamin D, antihistamines, alpha-blockers, anti-androgens, and nonsteroidal anti-inflammatory drugs (aRR, 0.69; 95% CI, 0.61–0.78). The effect of co-prescribed medications on 30-day mortality risk revealed the lowest risk for combined statins and metformin (aRR, 0.21; 95% CI, 0.15–0.31), followed by ACEi and statins (aRR, 0.25; 95% CI, 0.18–0.35), ACEi and metformin (aRR, 0.26; 95% CI, 0.17–0.40), antihistamines and NSAIDs (aRR, 0.41; 95% CI, 0.32–0.52), and in men, combined alpha-blockers and anti-androgens (aRR, 0.51; 95% CI, 0.42–0.64).
Conclusions
In this large national cohort, treatment of SARS-CoV-2 positive patients with individual or co-prescribed metformin and statins, ACEi and statins (or metformin) and other medications was associated with a markedly decreased 30-day mortality and can likely be continued safely. Clinical trials may assess their therapeutic benefit.
Similar content being viewed by others
INTRODUCTION
Coronavirus disease-19 (COVID-19) has become a leading cause of US deaths with its high infectivity, inadequate COVID-19 vaccination rates, and dearth of highly effective treatments.1,23,4,5 Despite concerted efforts to evaluate repurposed medications in the prevention and treatment of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), few agents have demonstrated efficacy in controlled clinical trials and/or received emergency use authorization. Among these, dexamethasone has the most consistent mortality benefit — decreasing mortality by approximately 30% in the RECOVERY Trial.6 However, there are many safe, commonly prescribed medications that have mechanisms of action and pharmacology that suggest that they could be beneficial for the treatment of COVID-19.
As the largest integrated US health care system, the Veterans Health Administration (VHA) includes extensive pharmacy data in its electronic health record database to assess the effect of licensed medications on SARS-CoV-2.3,7,8 In a national observational VHA cohort, we compared the 30-day mortality of Veterans testing positive for SARS-CoV-2 with and without prescriptions for medications hypothesized to modulate outcomes (in the presence and absence of potential confounders and risk modifiers).9 Medications which may modulate inflammation and/or cytokine release syndrome and affect COVID-19 mortality include the following: metformin, antihistamines, vitamin D, non-steroidal anti-inflammatory agents (NSAIDs), α-1 adrenergic receptor antagonists, statins, corticosteroids, and others.10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27 By examining approved therapeutics with a biologic rationale to affect COVID-19 progression in a large national cohort, we anticipate identifying drugs which may be safely continued in SARS-CoV-2 and may favorably impact mortality.
METHODS
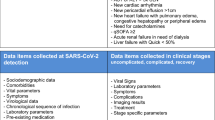
Study Design, Data Source, and Study Drug Selection
We previously developed a well-characterized patient cohort tested for SARS-CoV-2 using the COVID-19 shared data resource and related data in the Corporate Data Warehouse (CDW).28
Prior to analysis, we identified eleven safe, commonly used licensed medications with a mechanism of action or pharmacologic effect hypothesized to decrease SARS-CoV-2 30-day mortality as our study medications: angiotensin-converting enzyme inhibitors (ACEis), angiotensin receptor blockers (ARBs), alpha-blockers, anti-androgens, antihistamines, colchicine, metformin, nicotine replacement products, statins, and vitamin D.10,11,12,13,14,15,16 Inpatient or outpatient systemic administration of corticosteroids (e.g., dexamethasone) was treated as a covariate in our analysis.
Our hypothesis was that drugs suggested to alleviate COVID-19 progression through various mechanisms may exert protective effects and reduce overall mortality after SARS-CoV-2-infection. We also hypothesized that drugs may exert synergistic protective effects when used in combinations. Our specific aims were as follows: 1) to evaluate the associations between post-infection study drug use and 30-day overall mortality while considering confounders; and 2) to compare the risk reduction in single drug use vs. combination use for selected drug pairs. The Durham Veterans Affairs (VA) Health Care System Institutional Review Board approved this study protocol.
Cohort Definition
Using the previously defined cohort,28 we analyzed all the SARS-CoV-2 positive Veterans tested from March 1 to September 10, 2020. We included hospitalized and non-hospitalized patients, males and females, and all race/ethnicity categories for this analysis to increase the generalizability of the study findings. We report the first SARS-CoV-2 positive collection date as the index date and describe this first event only.
Study Variables Created for the SARS-COV-2 Cohort
Study Outcome
The primary outcome was 30-day overall mortality after the first positive SARS-CoV-2 test. The VA identifies deaths within and outside of the VA in the Corporate Data Warehouse through VA inpatient files, VA Beneficiary Identification and Records Locator System, Social Security Administration death files, and the Department of Defense.29
Predictor Variables
The primary predictors were use of the selected medications (listed in Supplementary Table 1). Using outpatient and inpatient prescription and dispense records, medication use was defined as drugs administered at least 50% of the time (≥7 days or a half of the survival time) within 2 weeks post-SARS-CoV-2 testing. Eleven individual binary variables were created accordingly. To assess synergistic drug effects, we created four categories (−/−, −/+, +/−, and +/+) for each pair. All medication use within the VHA and non-VHA medication use recorded in CDW were analyzed. Only VA hospitalizations were included. Most Veterans receiving antihypertensives, antiandrogens, metformin, statins, and vitamin D within 2 weeks post-SARS-CoV-2 testing also had these medications prescribed and dispensed prior to the positive SARS-CoV-2 test. However, antihistamines, NSAIDs, colchicine, and nicotine replacement were more frequently prescribed and dispensed after SARS-CoV-2 testing than before.
Covariates
Applying definitions used in our previous analysis,28 we considered the following as covariates: age categories; sex; race; smoking status; alcohol use disorder; BMI categories; facility location; time of test, pre-test Charlson Comorbidity Index; and post-test hospitalization and systemic corticosteroid use (defined in the same manner as other primary predictors). We categorized patients by smoking status (i.e., current, former, or never); we used self-reported health factor data recorded preceding and closest to the positive SARS-CoV-2 test. Using International Classification of Diseases-10 codes, inpatient and outpatient diagnoses of key comorbidities, including alcohol use disorder, were recorded within 2 years before the index date. Briefly, locations of VA facilities and calendar month of diagnosis (i.e., SARS-CoV-2 test date) were included to adjust for geographic and temporal variations in infection rates, resources, and patient care. Charlson Comorbidity Index was included to adjust for baseline mortality risk.
Other Variables
Baseline comorbidities relevant to the VA population and length of hospital stay (days of the first hospitalization only) within 30 days of the SARS-CoV-2 test date were also defined for a descriptive analysis only.27
Statistical Analysis
Clinical characteristics were expressed as frequency and percentage for categorical variables and median and interquartile range (IQR) for continuous variables. Chi-square and Deuchler–Wilcoxon tests were used to compare the distribution of clinical characteristics between fatal and surviving cases.30
To assess the associations between post-index drug use and 30-day mortality, individual models were developed to compute unadjusted and adjusted relative risk (aRR) and 95% confidence intervals (CIs) of 30-day overall mortality for each of eleven selected drugs, with final model adjusted for age categories, race, sex, region, month of diagnosis, BMI categories, current smoking, alcohol use disorder, Charlson Comorbidity Index score categories, post-test hospitalization and systemic corticosteroid administration. A weighted average of stratum-specific estimates on the log-binomial scale was used to approximate aRR.31 This categorical method minimizes inflated effect sizes and non-collapsibility bias compared with adjusted odds ratios.
To assess synergistic drug effects, we developed multinomial models to compare aRR and 95% CI of 30-day mortality between single drug use and combination drug use, having no drug use as a common referent group. Adjustment for multiplicity was performed by the Hochberg–Bonferroni procedure, accounting for a common referent group (based on the closure method).32,33,34 This technique, also known as the Benjamini–Hochberg procedure, is designed to decrease the false discovery rate and minimize incorrectly rejecting the true null hypothesis (type I error).35 Study results were rounded using the Goldilocks (Efron–Whittemore) method.36 P-values <0.05 were considered statistically significant.
RESULTS
Demographics and Comorbidities
The study cohort consisted of 26,508 patients who tested positive for SARS-CoV-2 and were predominantly White (n=15,656; 59%), male (n=23,659; 89%), overweight or obese (n=21,790; 82%), with nearly half over age 60 (n=12,839; 48%) (Table 1). The group includes 9,815 [37%] Black and 4,453 [17%] Veterans of Latinx ethnicity, with fewer than 4% identified as Asian, American Indian/Alaska Native, Native Hawaiian/Other Pacific Islander, or Multiracial.
After the SARS-CoV-2 positive test, 7,845 (30%) patients were hospitalized within 30 days (Table 2). The 6,732 survivors (27%) were hospitalized for a median of 6 days (interquartile range, or IQR=10 days), while the 1,612 (69%) who died within 30 days were hospitalized for a median of 9 days (IQR=9 days; p<0.0001). Baseline Charlson Comorbidity Index scores were greater among those dying versus surviving (<0.0001). Compared with survivors, common selected comorbidities which were significantly greater in those who died within 30 days included hypertension (77% vs. 54%), hyperlipidemia (65% vs. 52%), atherosclerosis (54% vs. 23%), type 2 diabetes (51% vs. 32%), and chronic kidney disease (CKD; 38% vs. 14%).
Association of Analyzed Medications with 30-Day Mortality
Among those testing SARS-CoV-2 positive, the effect of eleven medications on the 30-day mortality was assessed as unadjusted and adjusted relative risk (aRR) (Table 3). All medications exhibited a decreased mortality risk in fully adjusted analyses. The largest decreases in mortality risk were observed for colchicine (aRR, 0.32; 95% CI, 0.15–0.67) and metformin (aRR, 0.33; 95% CI, 0.25–0.43), followed by angiotensin-converting-enzyme inhibitors (ACEi) (aRR, 0.43; 95% CI, 0.35–0.53), angiotensin II receptor blockers (ARBs) (aRR, 0.54; 95% CI, 0.43–0.69), vitamin D (aRR, 0.53; 95% CI, 0.37–0.77), statins (aRR, 0.54; 95% CI, 0.46–0.62), antihistamines (aRR, 0.57; 95% CI, 0.49–0.66), and alpha-blockers (aRR, 0.58; 95% CI, 0.51–0.66). Decreased risk was also seen for anti-androgens (aRR, 0.61; 95% CI,0.51–0.73, among male Veterans only) and nonsteroidal anti-inflammatory drugs (aRR, 0.69; 95% CI, 0.61–0.78). Nicotine replacement therapy exhibited a non-significant decreased risk of mortality (aRR, 0.60; 95% CI, 0.31–1.1).
Effect of Co-prescribed Medications on 30-Day Mortality Risk
We next analyzed the effect in SARS-CoV-2 positive patients of five commonly co-prescribed medications with differing mechanisms on 30-day mortality. The co-prescribed medications had a substantially lower mortality risk than either of the medications alone (Table 4). The mortality risk was lowest with the combination of statins and metformin (aRR, 0.21; 95% CI, 0.15–0.31), followed by ACEi and statins (aRR, 0.25; 95% CI, 0.18–0.35) and ACEi and metformin (aRR, 0.26; 95% CI, 0.17–0.40). Lower risk was also observed for combined antihistamines and NSAIDS (aRR, 0.41; 95% CI, 0.32–0.52), and in men, combined alpha-blockers and anti-androgens (aRR, 0.51; 95% CI, 0.42–0.64).
DISCUSSION
Of more than 26,000 SARS-CoV-2 positive Veterans in this diverse national cohort, most were male and White, and had overweight/obesity, with nearly half over age 60; one in three were Black and one in six Latinx. Compared with survivors, those who died had a significantly higher prevalence of hypertension, hyperlipidemia, atherosclerosis, diabetes, and chronic kidney disease. In SARS-CoV-2 positive individuals, we assessed the effect of study medications hypothesized to decrease mortality through effects on inflammation and other mechanisms. We found that metformin and colchicine, followed by ACEi and ARBs, were associated with the largest decreased risk of 30-day mortality. Vitamin D, statins, antihistamines, and alpha-blockers were associated with a moderate decrease in mortality risk, with a lesser effect observed for anti-androgens and NSAIDS. Nicotine replacement therapy showed a tendency toward a decreased mortality risk.
We then examined the effect of commonly co-prescribed medications on 30-day mortality risk, combining medications with differing mechanisms of action. Compared with each medication alone, all drug pairs were associated with a further decrease in 30-day mortality risk. Combined statins and metformin were associated with the greatest decrease in mortality risk relative to those who received neither drugs, followed by ACEi and statins or metformin. Antihistamines and NSAIDS also significantly decreased mortality risk, while alpha-blockers and anti-androgens decreased mortality risk in men.
Our findings suggest there may not be a need to discontinue use of these medications in patients receiving them when SARS-CoV-2 positive. In our study, many patients had indications for these study medications due to concomitant cardiovascular disease (CVD), CKD, or diabetes, which also increase the risk of severe COVID-19.37,38,39 In a large VHA study to identify the prevalence of prediabetes, nearly three of four overweight or obese Veterans exhibited prediabetes or diabetes40 — many of whom would likely benefit from use of metformin, statins, and ACEi, as recommended by the American Diabetes Association.41,42
With the ongoing coronavirus disease-19 (COVID-19) pandemic and high VHA rates of comorbidities, these promising individual and combination therapies could be prospectively studied in pragmatic controlled clinical trials to assess their therapeutic benefit. Among those SARS-CoV-2 positive, the therapeutic benefit of the statin and metformin drug pair may arise from its anti-inflammatory and other effects. Statins decrease inflammatory markers, thrombogenicity, and inflammasome activation in monocytes, while improving endothelial dysfunction.43,44 Metformin suppresses immune hyperactivation and reactive oxygen species, exhibits anti-microbial activity and decreased mortality in sepsis, in addition to improved glycemic control, and decreased insulin resistance.45 Observational COVID-19 clinical studies report decreased mortality risk with use of metformin and statins independently.11,18,22,46,47,48,49
In men in our study, a decreased 30-day mortality risk in SARS-CoV-2 positive Veterans was observed with combined alpha-blocker and anti-androgen therapy — which is commonly prescribed as a combination pill for benign prostatic hypertrophy. In severe COVID-19, inflammatory cytokines produced by macrophages can be increased by adrenaline; alpha-blockers prevent cytokine release and increase survival rate in observational analyses of COVID-1950 as well as non-COVID-19-associated acute respiratory distress syndrome (ARDS) or pneumonia, compared with nonusers. In a randomized controlled trial of the potent anti-androgen proxalutamide or placebo in 645 hospitalized men and women, proxalutamide decreased mortality 77%, relative to placebo, and was generally well-tolerated.51 These data suggest the value of examining a combined alpha-blocker and anti-androgen therapy in a controlled trial in SARS-COV-2 positive patients.
Our study data on ACEi, ARBs, and NSAIDS were supported by multiple studies reporting an association with decreased mortality in COVID-19. In a meta-analysis of more than 100,000 patients in 52 studies (predominantly observational), more than 26,000 patients receiving ACEi or ARBs for hypertension exhibited a significantly decreased mortality rate compared with those not receiving these drugs.17 In the OpenSAFELY observational cohort of nearly 2 million patients with osteoarthritis and rheumatoid arthritis, a lower adjusted risk of mortality was observed among the one in ten patients receiving NSAIDS with COVID-19, relative to those not on NSAIDS.20
We also observed a decreased mortality risk in SARS-CoV-2 positive Veterans with colchicine and vitamin D treatment. However, published data on the effect of these drugs on COVID-19 mortality are conflicting. The large randomized controlled COLCORONA community trial of colchicine vs. placebo (randomizing more than 4500 patients) revealed no statistically significant difference in COVID-19-associated clinical events.52 Similarly, while demonstrating benefit for influenza, vitamin D shows conflicting results in COVID-19 in several small randomized controlled trials, although a meta-analysis and systematic review reported vitamin D generally improved clinical outcomes.24
We found that 30-day mortality risk was decreased with post-SARS-CoV-2 positive treatment with antihistamines; nicotine replacement therapy exhibited no effect on mortality risk. While there is limited data on antihistamines in SARS-CoV-2, antihistamines display antiviral effects in vitro and a decreased rate of infection was reported with diphenhydramine, hydroxyzine, and azelastine use in more than 200,000 patients tested for SARS-CoV-2.53 In more than 80 nursing home patients receiving antihistamines and azithromycin with severe COVID-19, a fourfold lower mortality rate (6% vs 28%) was observed compared with data pooled from other nursing homes.27 A randomized controlled trial of nicotine replacement therapy in COVID-19 is ongoing.54 As a cholinergic agonist, nicotine inhibits inflammatory cytokines,55,56 which could favorably affect SARS-CoV-2 outcomes. Additional data are awaited to support the use of antihistamines and nicotine replacement products in SARS-CoV-2.
Our study’s strengths are its assessment of frequently prescribed licensed medications administered to SARS-CoV-2 positive patients which provides support that these drugs may not need to be discontinued and could be beneficial for reducing mortality. Its additional strengths include its national scope, large size, racially diverse population, and reliable pharmacy data. Assessing all positive SARS-CoV-2 cases in the more than nine million Veterans within our integrated healthcare system,57 we completed a detailed evaluation of prescribed medications and comorbidities that could influence 30-day mortality in SARS-CoV-2 positive patients. As the study medications are prescribed for many of the most common comorbidities in the VHA, these results are both reassuring and relevant to clinical care, supporting greater use of metformin, statins, and ACEi/ARBs, when indicated.
Despite accurate VHA medication dispensing data, our study is limited by the fact that we did not confirm adherence (i.e., this biases our results toward the null) and did not adjust for medications other than corticosteroids reported to decrease COVID-19 mortality (e.g., selective serotonin reuptake inhibitors, etc.), and over-the-counter medications were not fully recorded. However, with the low or absent medication co-payments in the VHA, medication adherence is increased relative to the general population.58 As the VHA population is largely comprised of older males (with females constituting approximately 10%), our results may not be fully generalizable to other healthcare systems. While we adjusted our analyses for baseline comorbidities, the potential remains for residual confounding, effect modification, misclassification bias, and collider effects among variables.
In conclusion, we observed a significantly decreased adjusted relative risk of 30-day mortality in SARS-CoV-2 positive patients receiving commonly prescribed medications postulated to have a favorable effect, including metformin, statins, ACEi, ARBs, alpha-blockers, anti-androgens, antihistamines, vitamin D, and NSAIDS. In assessing co-prescribed drugs, we found a markedly decreased 30-day mortality with combined metformin and statins; ACEi and statins (or metformin); and NSAIDS and antihistamines. In men, a lower 30-day mortality risk was observed with combined alpha-blockers and anti-androgens, a combination pill commonly prescribed for benign prostatic hypertrophy. Our findings suggest that these generally safe medications and drug pairs should not be discontinued in SARS-CoV-2 positive patients and could be beneficial for reducing mortality. Controlled clinical trials of promising therapies may assess their therapeutic benefit.
Abbreviations
- ACEi:
-
Angiotensin-converting enzyme inhibitor
- ARB:
-
Angiotensin II receptor blocker
- COVID-19:
-
Coronavirus disease-19
- CDW:
-
Corporate Data Warehouse
- NSAIDs:
-
Non-steroidal anti-inflammatory agents
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- VA:
-
Veterans Affairs
- VHA:
-
Veterans Health Administration
- VINCI:
-
Veterans Health Administration Informatics and Computing Infrastructure
References
Woolf SH, Chapman DA, Lee JH. COVID-19 as the leading cause of death in the United States. JAMA 2021;325(2):123-4.
Oran DP. Prevalence of asymptomatic SARS-CoV-2 infection. Ann Intern Med 2020;173(5):362-7.
Ioannou GN, Locke E, Green P, Berry K, O’Hare AM, Shah JA, et al. Risk factors for hospitalization, mechanical ventilation, or death among 10 131 US Veterans with SARS-CoV-2 infection. JAMA Network Open. 2020;3(9):e2022310-e.
Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among Black patients and White patients with Covid-19. N Engl J Med 2020;382(26):2534-43.
Karaca-Mandic P, Georgiou A, Sen S. Assessment of COVID-19 hospitalizations by race/ethnicity in 12 states. JAMA Intern Med 2021;181(1):131-4.
Group RC. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med 2020;384(8):693-704.
Ioannou GN, O'Hare AM, Berry K, Fan VS, Crothers K, Eastment MC, et al. Trends over time in the risk of adverse outcomes among patients with SARS-CoV-2 infection. Clin Infect Dis. 2021;ciab419. https://doi.org/10.1093/cid/ciab419.
Donnelly JP, Wang XQ, Iwashyna TJ, Prescott HC. Readmission and death after initial hospital discharge among patients with COVID-19 in a large multihospital system. JAMA. 2021;325(3):304-6.
Piazza G, Morrow DA. Diagnosis, management, and pathophysiology of arterial and venous thrombosis in COVID-19. JAMA. 2020;324(24):2548-9.
Zhang X-J, Qin J-J, Cheng X, Shen L, Zhao Y-C, Yuan Y, et al. In-hospital use of statins is associated with a reduced risk of mortality among individuals with COVID-19. Cell Meta. 2020;32(2):176-87.e4.
Rosenthal N, Cao Z, Gundrum J, Sianis J, Safo S. Risk factors associated with in-hospital mortality in a US national sample of patients with COVID-19. JAMA Network Open. 2020;3(12):e2029058-e.
Rossotti R, Travi G, Ughi N, Corradin M, Baiguera C, Fumagalli R, et al. Safety and efficacy of anti-il6-receptor tocilizumab use in severe and critical patients affected by coronavirus disease 2019: a comparative analysis. J Infect 2020;81(4):e11-e7.
Konig MF, Powell M, Staedtke V, Bai R-Y, Thomas DL, Fischer N, et al. Preventing cytokine storm syndrome in COVID-19 using α-1 adrenergic receptor antagonists. J Clin Invest 2020;130(7):3345-3347.
Thomsen RW, Christiansen CF, Heide-Jørgensen U, Vogelstein JT, Vogelstein B, Bettegowda C, et al. Association of α1-blocker receipt with 30-day mortality and risk of intensive care unit admission among adults hospitalized with influenza or pneumonia in Denmark. JAMA Netw Open 2021;4(2):e2037053.
Bilaloglu S, Aphinyanaphongs Y, Jones S, Iturrate E, Hochman J, Berger JS. Thrombosis in Hospitalized Patients With COVID-19 in a New York City Health System. JAMA. 2020: 324(8):799-801.
Chow JH, Khanna AK, Kethireddy S, Yamane D, Levine A, Jackson AM, et al. Aspirin use is associated with decreased mechanical ventilation, ICU admission, and in-hospital mortality in hospitalized patients with COVID-19. Anesth Analg 2021;132(4):930-941.
Baral R, Tsampasian V, Debski M, Moran B, Garg P, Clark A, et al. Association between renin-angiotensin-aldosterone system inhibitors and clinical outcomes in patients with COVID-19: a systematic review and meta-analysis. JAMA Netw Open 2021;4(3):e213594.
Gupta A, Madhavan MV, Poterucha TJ, DeFilippis EM, Hennessey JA, Redfors B, et al. Association between antecedent statin use and decreased mortality in hospitalized patients with COVID-19. Nat Commun 2021;12(1):1325.
Gordon DE, Hiatt J, Bouhaddou M, Rezelj VV, Ulferts S, Braberg H, et al. Comparative host-coronavirus protein interaction networks reveal pan-viral disease mechanisms. Science. 2020:370(6521):eabe9403.
Wong AY, MacKenna B, Morton CE, Schultze A, Walker AJ, Bhaskaran K, et al. Use of non-steroidal anti-inflammatory drugs and risk of death from COVID-19: an OpenSAFELY cohort analysis based on two cohorts. Ann Rheum Dis 2021;80(7):943-51.
Imam Z, Odish F, Gill I, O'Connor D, Armstrong J, Vanood A, et al. Older age and comorbidity are independent mortality predictors in a large cohort of 1305 COVID-19 patients in Michigan, United States J Intern Med 2020;288(4):469-76.
Khunti K, Knighton P, Zaccardi F, Bakhai C, Barron E, Holman N, et al. Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England. Lancet Diabetes Endocrinol 2021;9(5):293-303.
Sharma S, Ray A, Sadasivam B. Metformin in COVID-19: a possible role beyond diabetes. Diabetes Res Clin Pract 2020;164:108183.
Pal R, Banerjee M, Bhadada SK, Shetty AJ, Singh B, Vyas A. Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and meta-analysis. J Endocrinol Investig 2021;45(1):53-68.
Montopoli M, Zumerle S, Vettor R, Rugge M, Zorzi M, Catapano CV, et al. Androgen-deprivation therapies for prostate cancer and risk of infection by SARS-CoV-2: a population-based study (N = 4532). Ann Oncol 2020;31(8):1040-5.
Deftereos SG, Siasos G, Giannopoulos G, Vrachatis DA, Angelidis C, Giotaki SG, et al. The Greek study in the effects of colchicine in COvid-19 complications prevention (GRECCO-19 study): Rationale and study design. Hell J Cardiol 2020;61(1):42-5.
Morán Blanco JI, Alvarenga Bonilla JA, Homma S, Suzuki K, Fremont-Smith P, Villar Gómez de Las Heras K. Antihistamines and azithromycin as a treatment for COVID-19 on primary health care - a retrospective observational study in elderly patients. Pulm Pharmacol Ther 2021;67:101989.
Suzuki A, Efird JT, Redding TSt, Thompson AD, Jr., Press AM, Williams CD, et al. COVID-19-associated mortality in US Veterans with and without SARS-CoV-2 infection. Int J Environ Res Public Health 2021;18(16):8486.
Sohn M-W, Arnold N, Maynard C, Hynes DM. Accuracy and completeness of mortality data in the Department of Veterans Affairs. Popul Health Metrics 2006;4(1):2.
Kruskal WH. Historical notes on the wilcoxon unpaired two-sample test. J Am Stat Assoc 1957;52(279):356-60.
Breslow NE, Day NE. Statistical methods in cancer research. Volume I - The analysis of case-control studies. IARC Sci Publ. 1980(32):5-338.
Hochberg Y. A sharper Bonferroni procedure for multiple tests of significance. Biometrika. 1988;75(4):800-2.
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Methodol 1995;57(1):289-300.
Benjamini Y, Yekutieli D. False Discovery rate–adjusted multiple confidence intervals for selected parameters. J Am Stat Assoc 2005;100(469):71-81.
Efird JT, Nielsen SS. A method to compute multiplicity corrected confidence intervals for odds ratios and other relative effect estimates. Int J Environ Res Public Health 2008;5(5):394-8.
Efird JT. Goldilocks Rounding: achieving balance between accuracy and parsimony in the reporting of relative effect estimates. Cancer Informat 2021;20:1176935120985132.
Jalili M, et al. Characteristics and Mortality of Hospitalized Patients With COVID-19 in Iran: A National Retrospective Cohort Study. Ann Intern Med 2021;174(1):125-7.
Petrilli CM, Jones SA, Yang J, Rajagopalan H, O’Donnell L, Chernyak Y, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966.
Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430-6.
Moin T, Damschroder LJ, Youles B, Makki F, Billington C, Yancy W, et al. Implementation of a prediabetes identification algorithm for overweight and obese Veterans. J Rehabil Res Dev 2016;53(6):853-62.
American Diabetes Association. Cardiovascular disease and risk management: standards of medical care in diabetes-2018. Diabetes Care 2018;41(Suppl 1):S86-s104.
American Diabetes Association. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2018. Diabetes Care 2018;41(Suppl 1):S73-s85.
Kong F, Ye B, Lin L, Cai X, Huang W, Huang Z. Atorvastatin suppresses NLRP3 inflammasome activation via TLR4/MyD88/NF-κB signaling in PMA-stimulated THP-1 monocytes. Biomed Pharmacother 2016;82:167-72.
Bikdeli B, Madhavan MV, Gupta A, Jimenez D, Burton JR, Der Nigoghossian C, et al. Pharmacological agents targeting thromboinflammation in COVID-19: review and implications for future research. Thromb Haemost 2020;120(7):1004-24.
Scheen AJ. Metformin and COVID-19: from cellular mechanisms to reduced mortality. Diabetes Metab 2020;46(6):423-6.
Cariou B, Hadjadj S, Wargny M, Pichelin M, Gourdy P. Comment on Chen et al. Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication. Diabetes Care 2020;43:1399-1407. Diabetes Care 2020;43(10):e163-e164.
Luo P, Qiu L, Liu Y, Liu XL, Zheng JL, Xue HY, et al. Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis. Am J Trop Med Hyg 2020;103(1):69-72.
Crouse AB, Grimes T, Li P, Might M, Ovalle F, Shalev A. Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes. Front Endocrinol 2021;11(1081):600439.
Ibrahim S, Lowe JR, Bramante CT, Shah S, Klatt NR, Sherwood N, et al. Metformin and Covid-19: focused review of mechanisms and current literature suggesting benefit. Front Endocrinol 2021;12(625):587801.
Rose L, Graham L, Koenecke A, Powell M, Xiong R, Shen Z, et al. The association between Alpha-1 adrenergic receptor antagonists and in-hospital mortality from COVID-19. Front Med. 2021;8(304).
Cadegiani FA, Zimerman RA, Fonseca DN, Correia MN, Muller MP, Bet DL, et al. Efficacy of proxalutamide in hospitalized COVID-19 patients: a randomized, double-blind, placebo-controlled, parallel-design clinical trial. Cureus. 2021;13(12):e20691.
Tardif JC, Bouabdallaoui N, L'Allier PL, Gaudet D, Shah B, Pillinger MH, et al. Colchicine for community-treated patients with COVID-19 (COLCORONA): a phase 3, randomised, double-blinded, adaptive, placebo-controlled, multicentre trial. Lancet Respir Med 2021;9(8):924–932.
Reznikov LR, Norris MH, Vashisht R, Bluhm AP, Li D, Liao YJ, et al. Identification of antiviral antihistamines for COVID-19 repurposing. Biochem Biophys Res Commun 2021;538:173-9.
NCT04583410. Efficacy of Nicotine in Preventing COVID-19 Infection (NICOVID-PREV). Available at: https://clinicaltrials.gov/ct2/show/NCT04583410 Accessed on March 12 2021.
Farsalinos K, Niaura R, Le Houezec J, Barbouni A, Tsatsakis A, Kouretas D, et al. Editorial: Nicotine and SARS-CoV-2: COVID-19 may be a disease of the nicotinic cholinergic system. Toxicol Rep 2020;7:658-63.
Gauthier AG, Lin M, Wu J, Kennedy TP, Daley L-A, Ashby CR, et al. From nicotine to the cholinergic anti-inflammatory reflex – Can nicotine alleviate the dysregulated inflammation in COVID-19? J Immunotoxicol 2021;18(1):23-9.
US Department of Veterans Affairs. Available at https://www.va.gov/health/docs/VA_COVID_Response.pdf Accessed on July 20 2021.
Weidenbacher HJ, Beadles CA, Maciejewski ML, Reeve BB, Voils CI. Extent and reasons for nonadherence to antihypertensive, cholesterol, and diabetes medications: the association with depressive symptom burden in a sample of American veterans. Patient Prefer Adherence 2015;9:327-36.
Acknowledgements
We acknowledge the use of the Observational Medical Outcomes Partnership Common Core Library, a SQL library developed in The Center for Improving the Public’s Health through Informatics (CIPHI) in the Department of Biomedical Informatics (DBMI) at Vanderbilt Health (VUMC), graciously provided by Michael E. Matheny, MD, MS, MPH, Chad Dorn, MS, and Ruth M Reeves, PhD. This work was made possible with the data resource from the VA Informatics and Computing Infrastructure (VINCI) COVID-19 Shared Data Resource.
Funding
This work was funded by Veterans Affairs (VA) Clinical Science Research and Development COVID Rapid Response program and supported by resources from Durham VA Medical Center and Durham Cooperative Studies Program Epidemiology Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Hunt is a consultant to Akebia Therapeutics, Inc. Dr. Hostler is co-owner of Infection Control Education for Major Sports, LLC, and consultant for OneBeacon Insurance and Prime Education, LLC.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 31 kb)
Rights and permissions
About this article
Cite this article
Hunt, C.M., Efird, J.T., Redding, T.S. et al. Medications Associated with Lower Mortality in a SARS-CoV-2 Positive Cohort of 26,508 Veterans. J GEN INTERN MED 37, 4144–4152 (2022). https://doi.org/10.1007/s11606-022-07701-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07701-3