Abstract
Background
Education and income, as two primary socioeconomic indicators, are often used interchangeably in health research. However, there is a lack of clear distinction between these two indicators concerning their associations with health.
Objective
This study aimed to investigate the separate and combined effects of education and income in relation to incident type 2 diabetes and cardiovascular diseases in the general population.
Design and Participants
Participants aged between 30 and 65 years from the prospective Dutch Lifelines cohort study were included. Two sub-cohorts were subsequently created, including 83,759 and 91,083 participants for a type 2 diabetes cohort and a cardiovascular diseases cohort, respectively.
Main Measures
Education and income level were assessed by self-report questionnaires. The outcomes were incident type 2 diabetes and cardiovascular diseases (defined as the earliest non-fatal cardiovascular event).
Key Results
A total of 1228 new cases of type 2 diabetes (incidence 1.5%) and 3286 (incidence 3.6%) new cases of cardiovascular diseases were identified, after a median follow-up of 43 and 44 months, respectively. Low education and low income (<1000 euro/month) were both positively associated with a higher risk of incident type 2 diabetes (OR 1.24 [95%CI 1.04–1.48] and OR 1.71 [95%CI 1.30–2.26], respectively); and with a higher risk of incident cardiovascular diseases (OR 1.15 [95%CI 1.04–1.28] and OR 1.24 [95%CI 1.02–1.52], respectively); independent of age, sex, lifestyle factors, BMI, clinical biomarkers, comorbid conditions at baseline, and each other. Results from the combined associations of education and income showed that within each education group, a higher income was associated with better health; and similarly, a higher education was associated with better health within each income group, except for the low-income group.
Conclusions
Education and income were both independently associated with incident type 2 diabetes and cardiovascular diseases. The combined associations of these two socioeconomic indicators revealed that within each education or income level, substantial health disparities existed across strata of the other socioeconomic indicator. Education and income are two equally important socioeconomic indicators in health, and should be considered simultaneously in health research and policymaking.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Health disparities related to non-communicable diseases persist across socioeconomic strata. Abundant evidence has demonstrated that people with low socioeconomic status (SES) are disproportionately affected by higher risks of all-cause mortality, the metabolic syndrome, type 2 diabetes, and cardiovascular diseases.1,2,3,4 It has been suggested that limited access to health and health-care resources, chronic stress, unhealthy lifestyle, and exposure to pollutants were found to play an important role in explaining the adverse health outcomes associated with low SES.5
Education and income are two primary components of SES. However, a clear distinction between these two socioeconomic indicators is often lacking.3, 6, 7 Many studies on health disparities only considered one of t0hem,7 while some other studies focused on an aggregate measure of SES derived from multivariate statistics.8, 9 Research often made references to one indicator to corroborate findings into the other. There is increasing awareness that education and income should not be used interchangeably, since they capture different dimensions of health-related resources and may impact on health through different pathways.6, 7 As the main upstream determinants of health outcomes, research is needed to clarify the differences between education and income concerning their associations with health outcomes.
In public health practice, the inconsistent use of education and income may result in inaccurate identification of socioeconomically vulnerable groups, since people do not always hold a matching socioeconomic position.8 It has been suggested that having such status inconsistency carries its own health risks. However, to date, only a few studies have explored such health disparities within different socioeconomic strata.10,11,12,13 It is therefore also important to assess how different combinations of education and income levels are associated with health outcomes.
Therefore, using a large Dutch population cohort, this study aimed to evaluate the effects of education and income — separately and jointly using a combined indicator — on incident type 2 diabetes and cardiovascular diseases. Specifically, this study aimed to address how education and income may contribute to the short-term inequities in these two health outcomes.
METHODS
Cohort Design
The Lifelines cohort is a multidisciplinary prospective population-based cohort study that uses a unique three-generation design to study the health and health-related behaviors of 167,729 persons living in the north of The Netherlands. It employs a broad range of investigative procedures in assessing the biomedical, socio-demographic, behavioral, and physical factors, which contribute to health and disease of the general population. Before study entry, a signed informed consent form was obtained from each participant. The Lifelines study is conducted according to the principles of the Declaration of Helsinki and approved by the Medical Ethics Committee of the University Medical Center Groningen, The Netherlands. The overall design and rationale of the study have been described in detail elsewhere.14, 15
After the baseline assessment (T1, years 2007 to 2013), all participants were invited for new rounds of assessments approximately every 5 years. In between assessments, follow-up questionnaires were completed approximately once every 1.5–2.5 years (Supplementary Figure S1). The current analysis used data from the baseline assessment T1 and the second assessment T4, as well as the two follow-ups (T2 and T3) in between. Currently, the third round of assessment is on-going. Comprehensive physical examinations, biobanking of blood and urine, and questionnaires were conducted at T1 and T4. Follow-up questionnaires for status of type 2 diabetes and cardiovascular diseases were issued to participants at T2, T3, and T4.
Study Population
For this study, we included all participants aged between 30 and 65 years. We subsequently created two sub-cohorts from those included participants, with one for type 2 diabetes and the other for cardiovascular diseases. For the diabetes cohort, we included participants who were free of diabetes at baseline, and further excluded participants who had no follow-up data to determine status of diabetes. We also excluded participants who reported the development of type 1 diabetes or gestational diabetes during the follow-ups. For the cardiovascular diseases cohort, we included participants who were free of cardiovascular diseases at baseline, and further excluded participants who had no follow-up data to determine status of cardiovascular diseases. Participants who had less than 1 year of follow-up after baseline were also excluded. In order to avoid massive imputation, we additionally excluded participants who had no available data on education level and BMI at baseline for both sub-cohorts. This led to an additional exclusion of approximately 0.5% of the study population, which was not expected to influence our results. In total, 83,759 and 91,083 participants were included and analyzed in the diabetes cohort and the cardiovascular diseases cohort, respectively. Supplementary Figure S2 shows the study flow chart.
Data Collection
Ascertainment of Incident Type 2 Diabetes and Cardiovascular Diseases
Incident type 2 diabetes and cardiovascular diseases were assessed by self-report questionnaires at the two follow-ups (T2 and T3) and the second assessment (T4). Additionally, we assessed incident cases based on blood measurements and pathology on electrocardiograms, which were available at the second assessment (T4). For type 2 diabetes, an incident case was considered as fasting blood glucose ≥ 7.0 mmol/L or HbA1c ≥ 6.5%.16 For cardiovascular diseases, the primary outcome was defined as the earliest non-fatal major cardiovascular event, including stroke (ischemic and hemorrhagic), myocardial infarction, heart failure, percutaneous transluminal coronary angioplasty surgery, and coronary artery bypass grafting surgery.17 Secondary outcome was a composite of death from any cause and non-fatal major cardiovascular event as described above. However, data on prescribed medication was not available during follow-ups. Data of medical records, causes of death, and the precise time of diagnosis were also not available.
Assessment of Education and Income Levels
Education and income levels were assessed by self-report questionnaires (Supplementary Table S1). Highest education level was categorized according to the International Standard Classification of Education (ISCED): (1) low (level 0, 1, or 2); (2) middle (level 3 or 4); and (3) high (level 5 or 6).18 Income level was based on monthly household net income and was categorized as (1) low (<1000 euro/month); (2) lower-middle (1000–2000 euro/month); (3) upper-middle (2000–3000 euro/month); (3) high (>3000 euro/month); and (4) do not know/prefer not to answer.
Clinical Measurements
Blood samples were collected by venipuncture in a fasting state and serum levels of glucose, HbA1c, HDL-cholesterol, total cholesterol, and triglycerides were analyzed. Measurements of blood pressure, 12-lead electrocardiograms, and anthropometry were made by trained research staff following standardized protocols. These measurements were performed without shoes and heavy clothing. Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters. Hypertension status was defined as (1) hypertensive medication use (ATC codes C02, C03, C07, C08, C09); (2) systolic blood pressure ≥ 140 mmHg; or (3) diastolic blood pressure ≥ 90 mmHg.19
Assessment of Other Baseline Covariates
Age, smoking status (never, former, and current), and TV watching time were assessed by self-administered questionnaires. Physical activity level was assessed by the validated Short QUestionnaire to ASsess Health-enhancing physical activity (SQUASH), from which non-occupational moderate-to-vigorous physical activities (MVPA) were calculated in minutes per week.20 Dietary intake was assessed by a validated 110-item semi-quantitative self-administered food frequency questionnaire (FFQ).21 Macro- and micro-nutrients intake was calculated from the FFQ data according to the 2011 Dutch Food Composition Table (NEVO).22 The Lifelines Diet Score (LLDS) was calculated to evaluate the relative diet quality of each participant. The development of the LLDS has been described in detail elsewhere.23
Statistical Analysis
Associations of income and education with incident type 2 diabetes and cardiovascular diseases were estimated by logistic regression models, and results were shown as odds ratios (ORs) with 95% confidence intervals. For evaluation of the separate effects of education and income, these two socioeconomic indicators were singly and mutually adjusted in the models. An interaction term between education and income was also fit into the model to test possible effect modification. For evaluation of the combined effects of education and income, these two socioeconomic indicators were combined into twelve groups, e.g., a group of participants had high education and lower-middle income. The associations of these combined groups of education and income with incident type 2 diabetes and cardiovascular diseases were subsequently estimated. For all estimations, models were adjusted in a two-step manner: (1) basic model: age and sex; (2) multivariate model: age and sex from basic model, plus lifestyle behaviors (smoking status, TV watching time, non-occupational MVPA, total energy intake, LLDS, and alcohol intake), BMI, and clinical biomarkers (HDL-cholesterol, triglycerides, and blood pressure). For cardiovascular diseases, in the multivariate model, we additionally adjusted total cholesterol level and comorbid conditions at baseline (atrial fibrillation and diabetes). In all models, age was adjusted as a categorical variable, i.e., 30–39, 40–49, 50–59, and 60–65 years. Before estimation, values of HDL-cholesterol, triglycerides, BMI, total energy intake, total cholesterol, and blood pressure were log-transformed to improve normality. We also assessed the associations with adjustments for different domains of modifiable risk factors separately. Additionally, we determined the contribution of each modifiable risk factor in explaining the associations of income and education with incident type 2 diabetes and cardiovascular diseases by calculating the percentage of attenuation in the ORs after additional adjustment for another modifiable risk factor, in comparison to the previous reference model, namely 100%×(ORref−ORnew)/ORref.
Multiple imputation by chained equations was performed (creating 25 imputed datasets) to deal with missing data for income level (including both missing value and participants who responded “do not know” or “prefer not to answer”), LLDS, total energy intake, alcohol intake, non-occupational MVPA, and smoking status.24 These variables all had missing data more than 1%. All statistical analyses were conducted using STATA (version 13.1; StataCorp, College Station, TX).
Sensitivity Analysis
First, we repeated our analysis without imputation of income level for those who responded “do not know” or “prefer not to answer.” Instead, we recoded them as a single category in the income variable. Second, we evaluated the potential effect modifications by sex, age, unemployment status, comorbid conditions at baseline (cancer and cardiovascular diseases), and diabetes status at baseline and during follow-ups (for cardiovascular diseases), by additionally including an interaction term with education or income in the model. Third, for cardiovascular diseases, we performed a separate analysis, in which we adjusted the SCORE2 risk prediction algorithms according to the European Society of Cardiology.25 For type 2 diabetes, we additionally analyzed a composite outcome of incident type 2 diabetes and death from any cause, to gain insights into how death events during follow-ups may influence the results.
RESULTS
Baseline characteristics are shown in Table 1 and Supplementary Table S2. Approximately 28%, 40%, and 32% of participants reported having low, middle, and high education, respectively. For household net income, approximately 3%, 18%, 30%, and 33% of participants reported having low (<1000 euro), lower-middle (1000–2000 euro), upper-middle (2000–3000 euro), and high (>3000 euro) level of income per month, respectively; approximately 15% of participants did not disclose their income level. These numbers were comparable with the national-level data in The Netherlands, e.g., approximately 10% low-income households, and approximately 28% and 30% of the population had high and low education, respectively.26, 27 With increasing education level, participants tended to be younger and have higher income. In general, lifestyle behaviors, BMI, and clinical biomarkers were also socioeconomically patterned with more favorable conditions among people who had higher education level. Baseline characteristics across income levels showed similar socioeconomic patterns.
Frequency measures of incidences of type 2 diabetes and cardiovascular diseases across education and income levels are shown in Table 2. Among 83,759 participants included in the type 2 diabetes cohort, we identified 1228 cases of type 2 diabetes (incidence 1.5%) during a median follow-up of 43 months. Among 91,083 participants included in the cardiovascular diseases cohort, we identified 3286 cases of cardiovascular diseases (non-fatal cardiovascular events) during a median follow-up of 44 months. Additionally, a total of 1127 deaths were recorded during the follow-up in the cardiovascular diseases cohort. With decreasing education or income levels, incidences of type 2 diabetes and cardiovascular diseases increased. Supplementary Table S3 shows the frequency measures of incidences of type 2 diabetes and cardiovascular diseases among different combinations of education and income levels.
Separate associations of education and income with incident type 2 diabetes and cardiovascular diseases are shown in Tables 3 and 4 and Supplementary Table S4. Low education and low income were both positively associated with higher risks of type 2 diabetes and cardiovascular diseases after adjustment for age and sex (basic model). The mutual adjustment between education and income only moderately attenuated those associations. Additional adjustment for other covariates attenuated those associations as well. In the mutually adjusted multivariate model, participants with low education had 24% (OR 1.24 [95%CI 1.04–1.48]) and 15% (OR 1.15 [95%CI 1.04–1.28]) higher odds of incident type 2 diabetes and cardiovascular diseases, respectively; participants with low income had 71% (OR 1.71 [95%CI 1.30–2.26]) and 24% (OR 1.24 [95%CI 1.02–1.52]) higher odds of incident type 2 diabetes and cardiovascular diseases, respectively, using high education and high income as reference group as appropriate. Multiplicative interactive effects between education and income were absent: ORinteraction 1.01 (95%CI 0.91–1.12) and ORinteraction 0.97 (95%CI 0.91–1.04) in multivariate models for type 2 diabetes and cardiovascular diseases, respectively. For cardiovascular diseases, similar associations were observed for the secondary composite outcome, including both non-fatal cardiovascular event and death from any cause (Supplementary Table S5).
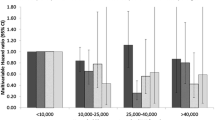
Joint associations of education and income with incident type 2 diabetes and cardiovascular diseases are shown in Figure 1 and Supplementary Table S6. In general, gradients of associations across education and income levels were observed after adjustment for age and sex. Further adjustment for other covariates substantially attenuated these associations. For cardiovascular diseases, gradients of associations were weakened after adjustments for these risk factors. In the multivariate model, participants who had high education and low income had the highest risks for incident type 2 diabetes (OR 3.04 [95%CI 1.52–6.05]) and cardiovascular diseases (OR 1.85 [95%CI 1.18–2.91]), followed by participants who had low education and low income, i.e., OR 2.24 [95%CI 1.54–3.25] for type 2 diabetes and OR 1.46 [95%CI 1.11–1.92] for cardiovascular diseases, using participants who had high education and high income as reference.
Joint associations of education and income with incident type 2 diabetes (a) and cardiovascular diseases (b). Figures are shown according to each education and income level, using high education and high income (>3000 euro/month) group as low risk reference (OR = 1.00). A dagger indicates a basic model: OR derived from multivariate logistic regression models adjusted for age and sex and n = 83,381 and n =90,531 for type 2 diabetes and cardiovascular diseases, respectively. A double dagger indicates a multivariate model: OR derived from multivariate logistic regression models adjusted for basic model covariates plus BMI, smoking status, TV watching time, non-occupational MVPA, total energy intake, LLDS, alcohol intake, HDL-cholesterol, triglycerides, blood pressure, and n = 82,722 and n = 89,251 for type 2 diabetes and cardiovascular diseases, respectively; for cardiovascular diseases, total cholesterol, diabetes at baseline, and atrial fibrillation at baseline were additionally adjusted in the multivariate model.
Percentages of attenuation in ORs across each education and income group are shown in Supplementary Table S4. When education and income were simultaneously controlled, adjustment for modifiable risk factors at baseline in total explained 33.1% and 15.2% of the associations of education with type 2 diabetes and cardiovascular diseases, respectively; for income, in total 23.5% and 7.7% of the associations were explained for type 2 diabetes and cardiovascular diseases, respectively. Adjustment for lifestyle behaviors explained more socioeconomic variations than other modifiable risk factors. Additional adjustments for clinical biomarkers and comorbid conditions at baseline (for cardiovascular diseases) showed no clear effects on explaining these socioeconomic variations.
Sensitivity analyses in general yielded similar results compared with the main analyses. Supplementary Table S7 presents the results of the analysis by including the responses of “do not know” or “prefer not to answer” for income as a single category. Large variations in the risks of incident type 2 diabetes and cardiovascular diseases were found in this income group across education levels. Furthermore, no significant multiplicative interactive effects were found for sex, age, unemployment status, comorbid conditions at baseline, and diabetes status at baseline and during the follow-up (for cardiovascular diseases), with education and income (Supplementary Table S8). For cardiovascular diseases, results were basically unchanged when adjusting for the SCORE2 risk prediction algorithms according to the European Society of Cardiology (Supplementary Table S9). For type 2 diabetes, using a composite outcome of incident type 2 diabetes and death from any cause yielded a smaller effect size for education (low education: OR 1.11 [95%CI 0.98–1.25]) but a stronger effect size for income (low income: OR 1.85 [95%CI 1.51–2.27]), compared with the main results (Supplementary Table S10).
DISCUSSION
The primary objective of this study was to investigate the effects of education and income simultaneously on incident type 2 diabetes and cardiovascular diseases. Specifically, this study was directed at assessing the short-term inequities in incident type 2 diabetes and cardiovascular diseases. Using this large population-based cohort sample, we found that low education and low income were both independently but also differentially associated with higher risks of these two health outcomes. In addition, results from the combined associations of education and income revealed substantial health disparities in these two health outcomes across education and income levels.
In general, our results are consistent with previous similar studies on prevalent type 2 diabetes in a German cohort and incident type 2 diabetes in a US community-based cohort.7, 28 Our results on cardiovascular diseases are also comparable with an Italian cohort.29 Our analyses thus provide the very important additional evidence demonstrating the independent associations of education and income with incident type 2 diabetes and cardiovascular diseases in a European setting. With a broader perspective, we also found that our results were partly in line with studies conducted in different geographical and socioeconomic settings, despite the differences in study design and methodology that preclude direct comparisons. For example, a systematic review reported that low or middle education and low income were associated with higher risks of cardiovascular outcomes in US and European settings, while the effects of education were absent in Asian settings.30 On the other hand, a global study found that low education was a strong predictor for cardiovascular diseases in all 20 countries analyzed, while wealth showed no or weak associations.31 For type 2 diabetes, results seemed to be more consistent, as a meta-analysis found that both education and income were associated with a higher risk of developing type 2 diabetes, irrespective of different geographical settings.32 In brief, our study further underlines the broader notion that it is important to consider and prioritize education and income as two indispensable socioeconomic dimensions when addressing health disparities, irrespective of geographical and socioeconomic settings.4
The independent associations of education and income with health highlight that these two socioeconomic indicators are of equal importance and should both be considered in health research. Our findings support the hypothesis suggesting that education and income may impact on health through different causal processes, as they provide different dimensions of resources in relation to health.1, 3, 6, 7, 28, 33,34,35,36,37 More specifically, education determines one’s non-material resources such as knowledge, skills, and self-efficacy that help individuals ease their barriers to be more receptive to health messages and transfer those messages into health behaviors. Such improvements in cognitive functioning associated with higher education level were argued to be the major driver in delaying the onset of non-communicable diseases. On the other hand, income reflects one’s material resources in regard to health, such as healthy food, health services, and leisure time activities.6, 38,39,40 In line with these theoretical assumptions, we did observe that lifestyle behaviors explained a considerable proportion of the associations for both socioeconomic indicators.
Results of the combined associations of education and income indicated that their effects on health were likely to be additive. As we observed within each education or income level, substantial health disparities existed across strata of the other socioeconomic indicator. More specifically, we showed that within different education groups, a higher income was associated with a better health; similarly, within different income groups, a higher education was associated with a better health. Differences in modifiable risk factors did not fully annul these excessive risks. We further illustrate this with status inconsistency, that is, people having discrepant socioeconomic positions in two or more of these ranking indicators. For example, we observed that participants who had high income but low education were worse off regarding their health outcomes, compared with those who had a matching socioeconomic position (i.e., high income and high education). And such status inconsistency–related health disparities were prevalent across almost every education and income level in our study sample. Previous studies have shown that status inconsistency between education and occupational class carried higher health risks.12, 13, 41 Our findings thus provide further support of this in the dimensions of education and income. It should be noted that we observed some non-linear associations especially after adjustment for modifiable risk factors. As these non-linear associations appeared gradually with the stepwise adjustments, we were unable to clearly specify the causes of this counterintuitive finding.
In our study sample, approximately 5% of the study population had extreme status inconsistency; not surprisingly, education and income were only moderately correlated (Spearman’s correlation coefficient = 0.34, Supplementary Table S3). We therefore further emphasize the importance and necessity of considering both education and income. Especially in public health programs (such as healthy eating campaigns or diabetes screening) where the effectiveness and outreach are often compromised among people who are socioeconomically disadvantaged, additional attention and support should be given to those not only having low income, but also having low education.42 Additionally, further understanding of such within-group differences may lead the way toward the design of policies that do not require the adjustment of socioeconomic characteristics that are generally fixed such as education. Indeed, in our case, income supports individuals who had low education, which may contribute to their health even after their education level has been attained.
Of all modifiable risk factors examined, lifestyle behaviors and BMI contributed the most to the socioeconomic gradients, while additional adjustment for clinical biomarkers did not further explain those health disparities. The higher risk for cardiovascular diseases conferred by poor socioeconomic status also appeared to be independent of diabetes status. It is noteworthy that after accounting for all modifiable risk factors, a large proportion of the risks for type 2 diabetes and cardiovascular diseases were still left unexplained. Previous studies have found that the most socioeconomically deprived individuals had disproportionately higher risks for type 2 diabetes and cardiovascular diseases, even if they practiced the healthiest lifestyle.2, 43 These results indicate that even though people who have low socioeconomic status may benefit from lifestyle interventions and obesity control, their excessively higher risks of developing type 2 diabetes and cardiovascular diseases may still be preserved. Particularly, as our study was based in the context of The Netherlands, a developed country with a high coverage of government-subsidized public education system and well-structured social security system, the persistent socioeconomic patterning in health inequities observed may not be addressed only by extensive public health interventions, but also through institutional and structural changes with support in all socioeconomic dimensions simultaneously.6
Strengths of this study include the large sample size, which allows the investigation of joint associations of education and income with sufficient statistical power. Secondly, we also conducted sensitivity analyses supporting the robustness of our findings. On the other hand, several limitations should be noted. Because of the intrinsic limitation of the Lifelines questionnaire, we are unable to translate household net income level into individual equivalent disposable income level. Since the Lifelines cohort study was established in The Netherlands, a country with a well-developed welfare system, it may not be possible to extrapolate our results to other population groups in another setting. We are also unable to assess the possible changes in participants’ education and income level. However, education is considered to be very stable over the entire adult life. Similarly, income in The Netherlands is also relatively stable because of the organization of the Dutch labor market (e.g., wide-spread use of collective wage bargaining as well as generous unemployment insurance). We therefore do not expect dramatic changes in participants’ socioeconomic status during follow-up.44 Another limitation is that the resolution in time, regarding the time of diagnosis of type 2 diabetes and cardiovascular diseases, was limited in the Lifelines dataset, hence limiting the suitability of the data for survival analysis. Nevertheless, considering the low event rate, moderate effect sizes, and the relatively short follow-up time, logistic regression models may provide similar estimates for the effect sizes. We therefore used logistic regression models instead.45, 46 Furthermore, misclassification could occur in the ascertainment of cases of type 2 diabetes and cardiovascular diseases, as at T2 and T3 only self-reported data was available. Data on participants’ medical records and causes of death were not available in the Lifelines study. Natriuretic peptide measurements, echocardiography, and coronary imaging were not performed in the Lifelines study. For type 2 diabetes, however, we consider this lack of medical records is not expected to substantially influence our results, since at T4 most new cases were identified by objective laboratory measurements, which is a strength of our study. For cardiovascular diseases, we cross-checked new self-reported cases at T4 with electrocardiographic results. Finally, approximately 18% of the study population was excluded because of loss of follow-up. However, we do not expect this attrition to substantially influence our results. We did not observe substantial differences in the baseline characteristics between the included participants and those who had no follow-up data (Supplementary Table S11), although there seemed to be fewer participants having high education or high income among those who had no follow-up information; participants who had no follow-up data also appeared to smoke more. A simulation study found that loss to follow-up (<50%) may lead to minor underestimation on the estimates of socioeconomic inequities in cohort studies.47 This suggests if full information was available, our estimation would be even more pronounced, despite the clear gradients of associations that have already been revealed in our results.
CONCLUSIONS
In conclusion, our results showed that education and income were both independently and also differentially associated with incident type 2 diabetes and cardiovascular diseases. Additionally, by analyzing the effects of education and income using a combined indicator, substantial health disparities were observed within socioeconomic groups. These findings suggest that education and income are two equally indispensable socioeconomic indicators in health, and should both be considered in health research and policymaking.
Data Availability
The manuscript is based on the data from the Lifelines cohort study. Lifelines adheres to standards for data availability. The data catalogue of the Lifelines cohort study is publicly accessible at www.lifelines.nl. All international researchers can obtain data at the Lifelines research office (research@lifelines.nl), for which a fee is required. The Lifelines research system allows access for reproducibility of the study results.
Abbreviations
- BMI:
-
Body mass index
- FFQ:
-
Food frequency questionnaire
- LLDS:
-
Lifelines Diet Score
- MVPA:
-
Moderate-to-vigorous physical activity
- SES:
-
Socioeconomic status
References
Bonaccio M, Di Castelnuovo A, Costanzo S, Persichillo M, Donati MB, de Gaetano G, et al. Interaction between education and income on the risk of all-cause mortality: prospective results from the MOLI-SANI study. Int J Public Health. 2016;61(7):765-76. https://doi.org/10.1007/s00038-016-0822-z
Vinke PC, Navis G, Kromhout D, Corpeleijn E. Socio-economic disparities in the association of diet quality and type 2 diabetes incidence in the Dutch Lifelines cohort. EClinicalMedicine. 2020;19:100252. https://doi.org/10.1016/j.eclinm.2019.100252
Blanquet M, Legrand A, Pelissier A, Mourgues C. Socio-economics status and metabolic syndrome: A meta-analysis. Diabetes Metab Syndr. 2019;13(3):1805-12. https://doi.org/10.1016/j.dsx.2019.04.003
Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, et al. Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation. 2018;137(20):2166-78. https://doi.org/10.1161/CIRCULATIONAHA.117.029652
Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood). 2002;21(2):60-76. https://doi.org/10.1377/hlthaff.21.2.60
Herd P, Goesling B, House JS. Socioeconomic position and health: the differential effects of education versus income on the onset versus progression of health problems. J Health Soc Behav. 2007;48(3):223-38. https://doi.org/10.1177/002214650704800302
Geyer S, Hemström Ö, Peter R, Vågerö D. Education, income, and occupational class cannot be used interchangeably in social epidemiology. Empirical evidence against a common practice. J Epidemiol Community Health. 2006;60(9):804-10. https://doi.org/10.1136/jech.2005.041319
Sharker MAY, Nasser M, Abedin J, Arnold BF, Luby SP. The risk of misclassifying subjects within principal component based asset index. Emerg Themes Epidemiol. 2014;11(1):6. https://doi.org/10.1186/1742-7622-11-6
Zhu Y, Duan MJ, Riphagen IJ, Minovic I, Mierau JO, Carrero JJ, et al. Separate and combined effects of individual and neighbourhood socio-economic disadvantage on health-related lifestyle risk factors: a multilevel analysis. Int J Epidemiol. 2021;50(6):1959-69. https://doi.org/10.1093/ije/dyab079
Ferrer RL, Palmer R. Variations in health status within and between socioeconomic strata. J Epidemiol Community Health. 2004;58(5):381-7. https://doi.org/10.1136/jech.2002.003251
de Boer WIJ, Dekker LH, Koning RH, Navis GJ, Mierau JO. How are lifestyle factors associated with socioeconomic differences in health care costs? Evidence from full population data in the Netherlands. Prev Med. 2020;130:105929. https://doi.org/10.1016/j.ypmed.2019.105929
Honjo K, Iso H, Inoue M, Sawada N, Tsugane S. Socioeconomic status inconsistency and risk of stroke among Japanese middle-aged women. Stroke. 2014;45(9):2592-8. https://doi.org/10.1161/strokeaha.114.005238
Braig S, Peter R, Nagel G, Hermann S, Rohrmann S, Linseisen J. The impact of social status inconsistency on cardiovascular risk factors, myocardial infarction and stroke in the EPIC-Heidelberg cohort. BMC Public Health. 2011;11:104. https://doi.org/10.1186/1471-2458-11-104
Scholtens S, Smidt N, Swertz MA, Bakker SJ, Dotinga A, Vonk JM, et al. Cohort Profile: LifeLines, a three-generation cohort study and biobank. Int J Epidemiol. 2014;44(4):1172-80. https://doi.org/10.1093/ije/dyu229
Klijs B, Scholtens S, Mandemakers JJ, Snieder H, Stolk RP, Smidt N. Representativeness of the LifeLines Cohort Study. PLOS ONE. 2015;10(9):e0137203. https://doi.org/10.1371/journal.pone.0137203
World Health Organization (WHO), International Diabetes Federation (IDF). Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia: report of a WHO/IDF consultation. Geneva, Switzerland; 2006.
van der Ende MY, Hartman MH, Hagemeijer Y, Meems LM, de Vries HS, Stolk RP, et al. The LifeLines Cohort Study: prevalence and treatment of cardiovascular disease and risk factors. Int J Cardiol. 2017;228:495-500. https://doi.org/10.1016/j.ijcard.2016.11.061
UNESCO. International Standard Classification of Education - ISCED 2011. Montreal, Canada: UNESCO Institute for Statistics; 2012.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041. https://doi.org/10.1097/hjh.0000000000001940
Wendel-Vos GC, Schuit AJ, Saris WH, Kromhout D. Reproducibility and relative validity of the short questionnaire to assess health-enhancing physical activity. J Clin Epidemiol. 2003;56(12):1163-9. https://doi.org/10.1016/s0895-4356(03)00220-8
Streppel MT, de Vries JH, Meijboom S, Beekman M, de Craen AJ, Slagboom PE, et al. Relative validity of the food frequency questionnaire used to assess dietary intake in the Leiden Longevity Study. Nutr J. 2013;12:75. https://doi.org/10.1186/1475-2891-12-75
Dutch Food Composition Table - version 3 [database on the Internet]. RIVM (National Institute of Public Health and the Environment). 2011 [cited 13 Mar 2021]. Available from: https://www.rivm.nl/nieuws/nieuwe-nevo-tabel-2011-beschikbaar.
Vinke PC, Corpeleijn E, Dekker LH, Jacobs DR, Jr., Navis G, Kromhout D. Development of the food-based Lifelines Diet Score (LLDS) and its application in 129,369 Lifelines participants. Eur J Clin Nutr. 2018;72(8):1111-9. https://doi.org/10.1038/s41430-018-0205-z
van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med. 1999;18(6):681-94. https://doi.org/10.1002/(sici)1097-0258(19990330)18:6<681::aid-sim71>3.0.co;2-r
Score Working Group, ESC Cardiovascular Risk Collaboration. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 2021;42(25):2439-54. https://doi.org/10.1093/eurheartj/ehab309
Statistics Netherlands. Trends in The Netherlands 2017. The Hague. 2017. https://longreads.cbs.nl/trends17-eng/labour_and_income/figures/income_and_expenditure/.
Statistics Netherlands. Dutch population better educated. The Hague. 2013. https://www.cbs.nl/en-gb/news/2013/40/dutch-population-better-educated.
Maty SC, Everson-Rose SA, Haan MN, Raghunathan TE, Kaplan GA. Education, income, occupation, and the 34-year incidence (1965-99) of Type 2 diabetes in the Alameda County Study. Int J Epidemiol. 2005;34(6):1274-81. https://doi.org/10.1093/ije/dyi167
Petrelli A, Gnavi R, Marinacci C, Costa G. Socioeconomic inequalities in coronary heart disease in Italy: a multilevel population-based study. Soc Sci Med. 2006;63(2):446-56. https://doi.org/10.1016/j.socscimed.2006.01.018
Khaing W, Vallibhakara SA, Attia J, McEvoy M, Thakkinstian A. Effects of education and income on cardiovascular outcomes: A systematic review and meta-analysis. Eur J Prev Cardiol. 2017;24(10):1032-42. https://doi.org/10.1177/2047487317705916
Rosengren A, Smyth A, Rangarajan S, Ramasundarahettige C, Bangdiwala SI, AlHabib KF, et al. Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: the Prospective Urban Rural Epidemiologic (PURE) study. Lancet Glob Health. 2019;7(6):e748-e60. https://doi.org/10.1016/S2214-109X(19)30045-2
Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011;40(3):804-18. https://doi.org/10.1093/ije/dyr029
Fitzpatrick T, Rosella LC, Calzavara A, Petch J, Pinto AD, Manson H, et al. Looking beyond income and education: socioeconomic status gradients among future high-cost users of health care. Am J Prev Med. 2015;49(2):161-71. https://doi.org/10.1016/j.amepre.2015.02.018
Leinonen T, Martikainen P, Lahelma E. Interrelationships between education, occupational social class, and income as determinants of disability retirement. Scand J Public Health. 2012;40(2):157-66. https://doi.org/10.1177/1403494811435492
Veenstra G, Vanzella-Yang A. Does household income mediate the association between education and health in Canada? Scand J Public Health. 2020;49(8):857-64. https://doi.org/10.1177/1403494820917534
Allen K, McFarland M. How are income and education related to the prevention and management of diabetes? J Aging Health. 2020;32(9):1063-74. https://doi.org/10.1177/0898264319879608
Hoveling LA, Liefbroer AC, Bültmann U, Smidt N. Understanding socioeconomic differences in incident metabolic syndrome among adults: What is the mediating role of health behaviours? Prev Med. 2021;148:106537. https://doi.org/10.1016/j.ypmed.2021.106537
Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey Smith G. Indicators of socioeconomic position (part 1). J Epidemiol Community Health. 2006;60(1):7-12. https://doi.org/10.1136/jech.2004.023531
Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey Smith G. Indicators of socioeconomic position (part 2). J Epidemiol Community Health. 2006;60(2):95-101. https://doi.org/10.1136/jech.2004.028092
Mirowsky J, Ross CE. Education, health, and the default American lifestyle. J Health Soc Behav. 2015;56(3):297-306. https://doi.org/10.1177/0022146515594814
Faresjö T, Svärdsudd K, Tibblin G. The concept of status incongruence revisited: a 22-year follow-up of mortality for middle-aged men. Scand J Soc Med. 1997;25(1):28-32. https://doi.org/10.1177/140349489702500107
Kivela J, Wikstrom K, Virtanen E, Georgoulis M, Cardon G, Civeira F, et al. Obtaining evidence base for the development of Feel4Diabetes intervention to prevent type 2 diabetes - a narrative literature review. BMC Endocr Disord. 2020;20(Suppl 1):140. https://doi.org/10.1186/s12902-019-0468-y
Foster HME, Celis-Morales CA, Nicholl BI, Petermann-Rocha F, Pell JP, Gill JMR, et al. The effect of socioeconomic deprivation on the association between an extended measurement of unhealthy lifestyle factors and health outcomes: a prospective analysis of the UK Biobank cohort. Lancet Public Health. 2018;3(12):e576-e85. https://doi.org/10.1016/S2468-2667(18)30200-7
de Boer WIJ, Mierau JO, Schoemaker J, Viluma L, Koning RH, Lifelines Corona Research I. The impact of the Covid-19 crisis on socioeconomic differences in physical activity behavior: Evidence from the Lifelines COVID-19 cohort study. Prev Med. 2021;153:106823. https://doi.org/10.1016/j.ypmed.2021.106823
Annesi I, Moreau T, Lellouch J. Efficiency of the logistic regression and Cox proportional hazards models in longitudinal studies. Stat Med. 1989;8(12):1515-21. https://doi.org/10.1002/sim.4780081211
Green MS, Symons MJ. A comparison of the logistic risk function and the proportional hazards model in prospective epidemiologic studies. J Chronic Dis. 1983;36(10):715-23. https://doi.org/10.1016/0021-9681(83)90165-0
Howe LD, Tilling K, Galobardes B, Lawlor DA. Loss to follow-up in cohort studies: bias in estimates of socioeconomic inequalities. Epidemiology. 2013;24(1):1-9. https://doi.org/10.1097/EDE.0b013e31827623b1
Acknowledgements
The authors wish to acknowledge the services of the Lifelines cohort study, the contributing research centers delivering data to Lifelines, and all the study participants.
Funding
This project has received funding from the European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie grant agreement no. 754425 (Ming-Jie F. Duan). This project also received financial support from the China Scholarship Council (Yinjie Zhu). The Lifelines Biobank initiative has been made possible by subsidies from the Dutch Ministry of Health, Welfare and Sport, the Dutch Ministry of Economic Affairs, the University Medical Center Groningen (UMCG), University of Groningen, and the Provinces in the north of The Netherlands (Drenthe, Friesland, Groningen). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
MJD conceptualized the study. MJD, YZ, LHD, and GN designed the study. MJD analyzed the data and drafted the manuscript. YZ organized the supplementary data. YZ, LHD, JOM, EC, SJLB, and GN contributed to the discussion and critically reviewed/edited the manuscript. LHD and GN supervised the project. MJD and YZ have primary responsibility for the final content. All authors approved the final content of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The study was conducted in accordance with the Declaration of Helsinki and the protocol was approved by the Medical ethical committee of the University Medical Center Groningen Institutional Review Board, The Netherlands (2007/152).
Conflict of Interest
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ming-Jie F. Duan and Yinjie Zhu are joint first authors.
Supplementary Information
ESM 1
(DOCX 201 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Duan, MJ.F., Zhu, Y., Dekker, L.H. et al. Effects of Education and Income on Incident Type 2 Diabetes and Cardiovascular Diseases: a Dutch Prospective Study. J GEN INTERN MED 37, 3907–3916 (2022). https://doi.org/10.1007/s11606-022-07548-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07548-8