Abstract
Background
Multidisciplinary transitional care services reduce readmissions for high-risk patients, but it is unclear if health system costs to offer these intensive services are offset by avoidance of higher downstream expenditures.
Objective
To evaluate net costs for a health system offering transitional care services
Design
One-year pragmatic, randomized trial
Participants
Adults aged ≥ 18 without a usual source of follow-up care at the time of hospital discharge were enrolled through a high-volume, urban academic medical center in Chicago, IL, USA, from September 2015 through February 2016.
Interventions
Eligible patients were silently randomized before discharge by an automated electronic health record algorithm allocating them in a 1:3 ratio to receive routine coordination of post-discharge care (RC) versus being offered intensive, multidisciplinary transitional care (TC) services.
Main Measurements
Health system costs were collected from facility administrative systems and transformed to standardized costs using Medicare reference files. Multivariable generalized linear models estimated proportional differences in net costs over one year.
Key Results
Study patients (489 TC; 164 RC) had a mean age of 44 years; 34% were uninsured, 55% had public insurance, and 49% self-identified as Black or Latinx. Over 90 days, cost differences between groups were not statistically significant. Over 180 days, the TC group had 41% lower ED/observation costs (adjusted cost ratio [aCR], 0.59; 95% CI, 0.36–0.97), 50% lower inpatient costs (aCR, 0.50; 95% CI, 0.27–0.95), and 41% lower total healthcare costs (aCR, 0.59; 95% CI, 0.36–0.99) than the RC group. Over 365 days, total cost differences remained of similar magnitude but no longer were statistically significant.
Conclusions
Offering TC services for vulnerable adults at discharge reduced net health system expenditures over 180 days. The promising economic case for multidisciplinary transitional care interventions warrants further research.
Trial Registration
National Clinical Trials Registry (NCT03066492)
Similar content being viewed by others
INTRODUCTION
Care transitions after hospital discharge are unsuccessful when follow-up care is delayed,1 inpatient and outpatient services are not coordinated,2,3 or insufficient attention is placed on psychological or social needs that interfere with a patient’s self-care.4 In the absence of timely, coordinated, and patient-centered transitional care, early warning signs of declining health can remain unrecognized, resulting in added burden for patients, caregivers, and healthcare systems, often culminating in readmission. These issues are magnified for patients of low socioeconomic status (SES), who often lack health insurance or access to a patient-centered medical home. Low-SES individuals also face more difficulty comprehending and following discharge plans and experience social and economic stressors that interfere with daily self-management behaviors and engagement with effective support services after discharge.5,6,7
Transitional care interventions involve supplemental resources and services to promote a safe and timely transfer from one level of care (or setting) to another, ensure healthcare continuity, and avoid preventable poor outcomes among at-risk populations.8 Such interventions have proved more effective when incorporating multidisciplinary care teams and combining multiple strategies to interrupt paths to readmission relating to a patient’s symptom burden, self-care, caregiver burden, co-occurring psychiatric or physical health conditions, and social and environmental conditions.9,10 Because the process for selecting, deploying, and coordinating multiple intervention components for each patient increases administrative costs, the financial sustainability of a transitional care approach depends on its effectiveness in reducing readmissions and other downstream expenditures, as well as its efficiency at deploying the right balance of resources and services for each patient.
We recently reported a pragmatic trial demonstrating reductions in hospital readmission with a multi-component transitional care intervention targeting adults without a usual source of medical care who were discharged from a large urban hospital or emergency department. Patients who were offered transitional care services experienced 42% fewer inpatient admissions over 180 days than those offered routine care.11 Given the importance of financial sustainability of transitional care interventions, we now report our evaluation of secondary outcomes of net healthcare expenditures for a health system offering transitional care services over 90, 180, and 365 days following discharge.
METHODS
Study Design
The study involves a pragmatic, individually randomized effectiveness trial comparing two different approaches for post-discharge care after inpatient or emergency department encounters at Northwestern Memorial Hospital in Chicago, IL. The transitional care (TC) approach involves pre-discharge instructions, assistance with scheduling, and engagement in multispecialty follow-up care services offered by a TC practice located across the street from the hospital. The routine care (RC) approach involves pre-discharge instructions and assistance scheduling follow-up care at local primary care offices (typically a federally qualified health center). Patients included in the study were encouraged, but not required, to utilize the post-discharge resources to which they were assigned. Study protocols are detailed elsewhere.12 The study protocol, which included a waiver of written informed consent, was approved by Northwestern University’s Institutional Review Board prior to pragmatic randomization of the first patient. Enrollment and the “silent” randomization of eligible patients within standard hospital discharge workflows occurred between September 2015 and February 2016. The research analysts had no contact with study participants and no role in the delivery of the healthcare interventions. The analysis protocol was posted on the National Clinical Trials Registry (NCT03066492), and pragmatic data extraction and analysis commenced in February 2017. The study was funded by the J.B. & M.K. Pritzker Family Foundation, which reviewed and approved the research protocol but had no role in the study conduct or reporting.
Study Sample and Randomization
Study randomization was pragmatically imbedded into standard hospital discharge workflows involving a patient referral services team that routinely arranges follow-up care and provides patient education prior to discharge. Specifically, adults aged ≥ 18 years who were discharged from an emergency department (ED), observation, or inpatient encounter between September 2015 and February 2016 and who did not have an existing source of follow-up primary care were computer-randomized by an imbedded electronic health record procedure that used digits in each patient’s medical record number to assign them in a 1:3 ratio for post-discharge care with either the RC or TC approach.12 No patients were excluded based on age, gender, race, ethnicity, nature of their health conditions, or insurance status.
TC Practice Intervention
The TC practice offers an array of services to stabilize medical and psychosocial issues, build patient self-efficacy, address social determinants of health, and transition each patient to a primary care medical home for long-term follow-up.11,12 When a referral is placed, TC staff attempt to engage the patient before leaving the hospital. The chart is reviewed, and phone calls are placed until the patient attends the initial TC visit. At this initial visit, the care team conducts comprehensive psychosocial and medical assessments to identify patient needs and develop individualized care plans. Each patient is offered a customized mix of services including generalist care, psychiatry, psychotherapy, medication reconciliation by a clinical pharmacist, social work, financial counseling, nursing services occurring at the practice or in the home, and support of a clinic-based “health advocate,” who functions much like a community health worker to provide culturally salient teaching, self-management support, community and healthcare resource navigation, and advocacy. Follow-up appointments are scheduled as needed, with many patients initially seen weekly for medication management, assistance with insurance applications, and self-management support. When the patient and care team agree the patient is ready to transition from the practice, the TC team schedules a visit with a community primary care provider (typically a partnering federally qualified health center) while being offered ongoing access to specialty care within the Northwestern Medicine health system.
Outcome Metrics and Data Collection
Our cost analysis compared net direct medical costs between patients in the two randomized treatment groups, from the perspective of the health system. Net healthcare expenditures include the direct medical costs of all care delivered at the TC practice and of other hospital and outpatient services provided to study patients throughout the Northwestern Medicine health system during the study period.
Costs of Services Offered by the TC Practice
We used an ingredient-based approach to estimate overall and per-patient operating costs for the TC practice.13,14,15 This involved (1) estimating total annual operating costs from administrative records; (2) determining the percentage of total operating costs consumed by study patients; (3) categorizing each cost component (i.e., personnel, supplies, office space use, etc.) as fixed or varying with the numbers of patients or practice visits; and (4) calculating per-person costs for each study patient, based on numbers of visits completed. We conducted interviews with health system leaders to identify all TC practice components and to estimate the proportion of time each personnel member spent in administrative versus patient care roles. Annual personnel costs were determined from 2017 national mean salaries found in the Occupational Employment Statistics published by the US Bureau of Labor Statistics,16 plus a fringe benefit rate set by the employing health system. Annual costs for clinical office space, utilities, and other facility operations were provided directly by health system administrators.
During the entire evaluation period, 27.3% of all visits to the TC practice were completed by study participants, so we estimated the portion of costs consumed by study participants to be 27.3% of total operating costs. Facilities costs and the cost of time spent by TC personnel performing administrative roles were considered fixed costs and assigned equally to each study participant managed by the TC practice (489 patients randomized to TC plus 10 patients randomized to RC who completed ≥ 1 TC visit). Average personnel costs for an initial TC visit (i.e., visit #1) were calculated differently from subsequent follow-up visits, because interviews with health system administrators identified that visit #1 involved a different mix of personnel and lasted 40% longer than the average follow-up TC visit. We applied the estimated cost of a typical visit #1 to each patient with at least one TC visit (186 patients randomized to TC and 10 patients in the RC group with TC visits). Similarly, we applied the estimated cost of a typical TC follow-up visit to every completed follow-up visit. The costs of time spent by personnel performing clinical roles were assigned to patients based on the number and type of TC practice visits completed. Costs of medical supplies and office-administered medications were divided equally across all completed visits. Mean 12-month TC practice costs overall and per person can be found in the Supplemental Appendix.
Costs of All Other Healthcare Services
Direct costs of all other healthcare services were estimated by assigning a relative dollar value to every billed professional and hospital service provided to every patient.17 Data sources included health system billing, diagnoses, procedures, patient demographic characteristics, payer information, and facility and provider information for all professional and hospital services rendered for a study period spanning 90 days before and 365 days after each patient’s date of randomization.
With the exception of TC practice encounters, all other professional services were assigned standardized costs derived from national reimbursement amounts in Medicare fee schedules for the year the service was rendered.18 This common approach for estimating direct medical costs was selected because it has national generalizability and circumvents the high variation in charges and reimbursements across facilities and other payers.19 Hospital-based services were assigned costs by multiplying charge amounts under each uniform billing revenue code by hospital-specific Medicare cost-to-charge ratios found in the hospital’s annual Medicare cost report.20 Sources of all reference files can be found in the Supplemental Appendix.
All costs during the follow-up period were categorized as ambulatory care (which included TC practice costs and the standardized costs of all other non-hospital and non-ED professional services), emergency (including hospital observation unit costs), or inpatient costs. Costs spanning 90 days prior to the randomization date, including costs for the index hospitalization or ED visit, were classified as baseline costs; costs after the date of randomization were categorized as occurring within 90, 180, and 365 days after randomization. All cost data were adjusted for medical care inflation to calendar year 2017, the year study follow-up concluded.
Statistical Analysis
Analyses were conducted using Stata, version 14.2 (StataCorp; College Station, TX). The primary cost analysis followed the intention-to-treat principle, including all patients based on the group to which they were randomly assigned, regardless of their participation in TC services. To account for the skewness and non-normality of cost outcome data, we estimated regression models using a generalized linear model (GLM) with log link, which provided inference on proportional differences between randomized treatment groups. After examining the relationship between the mean and variance of log-transformed cost data, and comparing observed cost data to predictions of models with different variance specifications, we selected the Poisson variance function in GLMs.21 After estimating final regression models, we calculated predictive margins using Stata’s “margins” command,22,23 which provided estimates of costs (in dollars) for each study group, adjusted across the sample’s covariate distribution. Regression models adjusted for age, sex, insurance (public, private, uninsured), race/ethnicity, homelessness, index visit type, and healthcare costs during the 90-day period preceding the index visit. After identifying deaths during study follow-up using National Death Index (NDI) records,24 regression models accounted for incomplete follow-up with an exposure term for days of follow-up while alive.
RESULTS
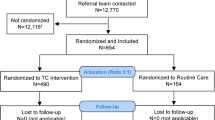
During the 6-month enrollment period between September 2015 and February 2016, 653 patients were identified as eligible and randomized (Fig. 1). Baseline characteristics of 489 patients randomized to TC and 164 patients randomized to RC are described in Table 1. The mean age of study participants was 44 years; 41% were women, 34% were uninsured, 55% were enrolled in a public insurance program, and the most common racial/ethnic group was Black/African-American (30.0%). Overall, 284 (43.5%) were discharged from an inpatient ward and 369 (56.5%) from the ED or an observation unit. As demonstrated previously,12 patients’ index visits were clinically heterogeneous; across 18 principal diagnosis categories for the index visit (e.g., cardiovascular, gastrointestinal, etc.), there were no significant differences between the two trial arms. Despite random allocation, patients assigned to RC were somewhat more likely to have their qualifying discharge after an inpatient rather than ED stay, and their mean total healthcare costs during the 90-day baseline period were higher: $12,874 (SD $20,693) for RC versus $10,956 (SD $20,209) for TC.
Trial flow diagram. *Patients in this group were not deemed by their care team to require coordinated follow-up care after discharge or were discharged after hours, when the discharge coordination team may have been unavailable. †Most patients who were assisted by the hospital discharge coordination team had an existing source of medical care follow-up and were not appropriate for randomization to TC follow-up care. A small number of patients who were eligible were not randomized because they had been referred to the TC practice by the inpatient care team for follow-up of a pending test result, such as a biopsy for a possible new cancer diagnosis. ‡Because assessment by the hospital discharge coordination team determined whether patients did or did not have access to a usual source of follow-up care, it is only possible to know the eligibility status of patients who were evaluated by this team. Some patients may have been eligible but not randomized if (A) the discharge team was not notified (e.g., a patient left against medical advice before a consult could be placed) or (B) the discharge team identified another existing source of follow-up care, such as a patient’s usual primary care provider.
Under the study’s randomized encouragement design, 186 (38.0%) of 489 patients randomized to TC actually attended ≥ 1 visit at the TC practice over 365 days of follow-up. In addition, 10 (5.4%) of 184 patients assigned to RC completed ≥ 1 TC practice visit. During follow-up, 25 patients randomized to TC (5.1%) died, and 10 patients randomized to RC (6.1%) died (p = 0.63). The average annual cost of offering TC services was estimated at $574 (95% CI $472–$675) per person randomized to TC (Table S1; Appendix). This cost ranged from $89 for each patient randomized but never seen (i.e., a portion of total annual facility costs and time spent by TC personnel to schedule and prepare for TC visits) to $10,484 for one patient with 40 completed visits to TC.
Comparisons of mean direct medical costs per person are presented in Table 2. There were no statistically significant differences in any of the four net cost outcome categories over the first 90 days of follow-up. However, over 180 days, the TC group had 41% lower ED/observation costs (adjusted cost ratio [aCR], 0.59; 95% confidence interval [CI], 0.36–0.97), 50% lower inpatient costs (aCR, 0.50; 95% CI, 0.27–0.95), and 41% lower total healthcare costs (aCR, 0.59; 95% CI, 0.36–0.99) than the RC group. Over 365 days, ED/observation costs in the TC group remained 40% lower (aCR, 0.60; 95% CI, 0.36–0.99), but other differences were no longer statistically significant at the p < 0.05 level.
DISCUSSION
This pragmatic trial finds that offering access to multidisciplinary TC services for adult patients with no usual source of follow-up care at the time of a hospital or ED discharge reduces net total healthcare expenditures, primarily as a result of lower inpatient and other acute care utilization that become statistically significant between 90 and 180 days after discharge with transitional care support. This finding is consistent with prior research demonstrating readmission reductions with TC interventions that begin prior to discharge and involve a multidisciplinary team designed to address the unique clinical, psychological, and social needs of each patient.9,10
The inherently temporary, high-intensity nature of transitional care services provides plausibility for our study findings. In our prior analysis of utilization outcomes,11 referral to TC reduced the hospital readmission rate by 37% over 90 days, but our current study found no significant difference in inpatient or total costs at 90 days. Costs of the TC practice (classified as ambulatory costs) largely accrue shortly after discharge, so any subsequent reduction in total costs resulting from fewer hospital readmissions would first need to offset those additional upfront costs before net savings are realized. Depending on the underlying rate of avoidable readmissions in the target population, an effective TC intervention may take many months to achieve “return on investment.” In this study, as differences in ED/observation and inpatient costs widened over 180 days, net total healthcare cost differences achieved statistical significance between 90 and 180 days. However, as most patients completed the transition to an alternative source for primary care between 180 and 365 days, total cost differences no longer remained statistically significant. This could mean that the effect of TC intervention services wanes as patients stop participating and begin to receive care in other settings that may place less focus on addressing social needs or coordinating behavioral health services. It is notable that the absolute differences in adjusted total costs between TC and RC were roughly similar at 180 days (i.e., $12,923 − $7665 = $5258) and 365 days (i.e., $18,148 − $12,749 = $5399), exhibiting that the offset in total costs that emerged by 180 days still persisted after 365 days.
Our study has limitations. First, the pragmatic randomized design is a strength over observational studies of delivery system innovations or randomized trials involving only select research volunteers. However, even with randomization, there were small baseline differences in prior healthcare utilization. Our analyses adjusted for these differences, but it is possible that differences in other unmeasured variables could have introduced residual confounding. Second, healthcare expenditures for high-utilizing patients are known to be highly variable,25,26 and intervention studies aiming to evaluate differences in those costs require large intervention effect sizes or very large sample sizes to achieve statistical significance. Cost was a secondary outcome in this study, so the sample size limits our ability to detect modest yet meaningful differences in healthcare expenditures. Third, our analysis of health system costs did not consider reimbursements received for some patients who were enrolled in some form of health insurance coverage. Such reimbursements could have either increased or decreased the differences we observed in net costs. Fourth, the study enrolled adults with multi-morbidity, including a high prevalence of behavioral health issues. Many were poor, racial/ethnic minorities, uninsured or enrolled in Medicaid, and living in urban communities heavily burdened by adverse structural determinants of health; many were homeless. Our findings may have less generalizability to other populations. Finally, the study population was identified at the time of discharge from a single hospital; it is possible that the net costs of implementing a TC practice approach may differ in other hospital settings that employ alternative approaches for discharge planning and hospital follow-up coordination.
Importantly, our study demonstrates that transitional care approaches for high-utilizing patient populations with multiple care needs can reduce readmissions and lead to meaningful reductions in healthcare expenditures. These findings raise additional questions that warrant further research, including whether biopsychosocial, team-based delivery system approaches targeting patients with both high clinical comorbidity and high social need can be sustained, or whether specific components of the multispecialty team approach studied here can be embedded in other medical home delivery models to enable durable health and economic benefits over the longer term. Future studies of transitional care interventions also should be designed to have sufficiently large sample size, and statistical power, to explicitly examine differences in healthcare cost outcomes.
References
Lee KK, Yang J, Hernandez AF, Steimle AE, Go AS. Post-discharge Follow-up Characteristics Associated With 30-Day Readmission After Heart Failure Hospitalization. Med Care. 2016;54(4):365-372.
Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003;51(4):549-555.
Burke RE, Guo R, Prochazka AV, Misky GJ. Identifying keys to success in reducing readmissions using the ideal transitions in care framework. BMC Health Serv Res. 2014;14:423.
Gold HT, Slover JD, Joo L, Bosco J, Iorio R, Oh C. Association of Depression With 90-Day Hospital Readmission After Total Joint Arthroplasty. J Arthroplasty. 2016;31(11):2385-2388.
Kangovi S, Barg FK, Carter T, et al. Challenges faced by patients with low socioeconomic status during the post-hospital transition. J Gen Intern Med. 2014;29(2):283-289.
Kangovi S, Levy K, Barg FK, Carter T, Long JA, Grande D. Perspectives of older adults of low socioeconomic status on the post-hospital transition. J Health Care Poor Underserved. 2014;25(2):746-756.
Englander H, Michaels L, Chan B, Kansagara D. The care transitions innovation (C-TraIn) for socioeconomically disadvantaged adults: results of a cluster randomized controlled trial. J Gen Intern Med. 2014;29(11):1460-1467.
Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The care span: The importance of transitional care in achieving health reform. Health Aff (Millwood). 2011;30(4):746-754.
Kansagara D, Chiovaro JC, Kagen D, et al. So many options, where do we start? An overview of the care transitions literature. J Hosp Med. 2016;11(3):221-230.
Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095-1107.
Liss DT, Ackermann RT, Cooper A, et al. Effects of a Transitional Care Practice for a Vulnerable Population: a Pragmatic, Randomized Comparative Effectiveness Trial. J Gen Intern Med. 2019;34(9):1758-1765.
Schaeffer C, Teter C, Finch EA, et al. A pragmatic randomized comparative effectiveness trial of transitional care for a socioeconomically diverse population: Design, rationale and baseline characteristics. Contemp Clin Trials. 2018;65:53-60.
Drummond M, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Fourth edition. ed. Oxford, United Kingdom: Oxford University Press; 2015.
Herman WH, Brandle M, Zhang P, et al. Costs associated with the primary prevention of type 2 diabetes mellitus in the diabetes prevention program. Diabetes Care. 2003;26(1):36-47.
Johns B, Baltussen R, Hutubessy R. Programme costs in the economic evaluation of health interventions. Cost Eff Resour Alloc. 2003;1(1):1.
BLS. National Employment and Wage Estimates, May 2017. US Bureau of Labor Statistics, Division of Occupational Employment Statistics. https://www.bls.gov/oes/current/oes_nat.htm#29-0000. Published 2017. Accessed September 23, 2019.
Visscher SL, Naessens JM, Yawn BP, Reinalda MS, Anderson SS, Borah BJ. Developing a standardized healthcare cost data warehouse. BMC Health Serv Res. 2017;17(1):396.
CMS. Physician Fee Schedule. Centers for Medicare and Medicaid Services. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched. Published 2020. Accessed May 29, 2020.
Tumeh JW, Moore SG, Shapiro R, Flowers CR. Practical approach for using Medicare data to estimate costs for cost-effectiveness analysis. Expert Rev Pharmacoecon Outcomes Res. 2005;5(2):153-162.
ResDAC. Introduction to Medicare Cost Reports. Research Data Assistance Center (ResDAC), University of Minnesota School of Public Health. https://resdac.org/sites/datadocumentation.resdac.org/files. Published 2020. Accessed June 14, 2020.
Buntin MB, Zaslavsky AM. Too much ado about two-part models and transformation? Comparing methods of modeling Medicare expenditures. J Health Econ. 2004;23(3):525-542.
Heslin KC, Elixhauser A, Steiner CA. Identifying in-patient costs attributable to the clinical sequelae and comorbidities of alcoholic liver disease in a national hospital database. Addiction. 2017;112(5):782-791.
Mitchell MN. Interpreting and visualizing regression models using Stata. Second. ed. College Station: Stata Press; 2020.
National Death Index. National Center for Health Statistics. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/ndi/index.htm. Published 2020. Accessed August 12, 2020.
Figueroa JF, Lyon Z, Zhou X, Grabowski DC, Jha AK. Persistence and Drivers of High-Cost Status Among Dual-Eligible Medicare and Medicaid Beneficiaries: An Observational Study. Ann Intern Med. 2018;169(8):528-534.
Figueroa JF, Zhou X, Jha AK. Characteristics And Spending Patterns Of Persistently High-Cost Medicare Patients. Health Aff (Millwood). 2019;38(1):107-114.
Acknowledgements
This study was made possible by funding from the J.B. & M.K. Pritzker Family Foundation, which reviewed and approved the research protocol but had no role in the study conduct or reporting. We thank the patients who participated in this study, along with care team members and staff at the Northwestern Medical Group Transitional Care Practice. We also thank the Chicago-area federally qualified health center partners that provided care to patients in both study arms. We also recognize the support and participation of Northwestern Memorial HealthCare and providers and staff at Northwestern Memorial Hospital.
Funding
This evaluation was supported by funding from the J.B. & M.K. Pritzker Family Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Ackermann, Dr. Liss, Dr. French, Mr. Cooper, and Ms. Aikman report no financial disclosures or conflicts of interest. Dr. Schaeffer, reports employment as a health care provider at the Northwestern Medical Group Transitional Care (TC) practice.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
Question: What are the health system costs of providing transitional care for patients with acute healthcare needs who do not have a usual source of primary care, and are those costs offset by lower costs for subsequent readmissions and other services?
Findings: In this pragmatic clinical trial, we found that offering multidisciplinary transitional care services to vulnerable adults without an existing source for follow-up care upon hospital discharge reduced net healthcare expenditures at 180 days.
Meaning: Transitional care interventions have the potential to improve patient care and reduce future healthcare expenditures for vulnerable adults who have no usual source of medical care.
Supplementary Information
ESM 1
(DOCX 98 kb)
Rights and permissions
About this article
Cite this article
Ackermann, R.T., Liss, D.T., French, D.D. et al. Randomized Trial Evaluating Health System Expenditures with Transitional Care Services for Adults with No Usual Source of Care at Discharge. J GEN INTERN MED 37, 3832–3838 (2022). https://doi.org/10.1007/s11606-022-07473-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07473-w