Abstract
Background
Guidelines suggest clinicians inform patients about their 10-year cardiovascular disease (CVD) risk; however, little is known about how the risk estimate influences patients’ preferences for statin therapy for primary prevention.
Objective
To define predictors of preference for statin therapy after participants were informed about their individualized benefits and harms.
Design
Cross-sectional survey in 2020.
Setting
Online US survey panel.
Participants
A national sample of 304 respondents aged 40 to 75 who had not previously taken a statin and who knew their cholesterol levels and blood pressure measurements.
Intervention
Participants entered their risk factors into a calculator which estimated their 10-year CVD risk. They were then provided with an estimate of their absolute risk reduction with a statin and the chance of side effects from meta-analyses.
Main Measurements
We used a hierarchical model to predict participants’ preferences for statin therapy according to their 10-year CVD risk, perceptions of the magnitude of statin benefit (large, medium, small, or almost no benefit), worry about side effects (very worried, somewhat worried, a little worried, not worried at all), and other variables.
Key Results
Participants had a mean age of 55 years (SD = 9.9); 50% were female, 44% were non-white, and 16% had a high school degree or less education. After reviewing their benefits and side effects, 45% of the participants reported they probably or definitely wanted to take a statin. In the full hierarchical model, only perceived benefits of taking a statin was a significant independent predictor of wanting a statin (OR 7.3, 95% CI 4.7, 12.2).
Limitations
Participants were from an internet survey panel and making hypothetical decisions.
Conclusions
Participants’ perceptions of their benefit from statin therapy predicted wanting to take a statin for primary prevention; neither estimated CVD risk nor worries about statin side effects were independent predictors.
Similar content being viewed by others
INTRODUCTION
US practice guidelines addressing statin therapy to reduce cardiovascular disease (CVD) risk recommend using the pooled cohort equations (PCEs) to estimate a patient’s 10-year risk of a CVD event.1,2,3 This risk estimate then drives guideline recommendations regarding prescription of a statin or having a discussion with the patient about their CVD risk and the potential benefits and harms of taking a statin.
We had previously reported an internet survey where we presented participants an estimate of their 10-year CVD risk as well as the absolute risk reduction they might expect from a statin, using icon arrays to facilitate understanding.4 We also presented estimates of the possible harms of statins. Participants were then asked whether they would want to take a statin (definitely or probably not take a statin, probably or definitely take a statin). In our previous paper, we presented the “preference distribution” of these informed participants wanting to take a statin across the spectrum of CVD risk and found this distribution to be relatively flat, suggesting a broad range of CVD risk for which discussions about statins should be indicated.4 In this paper, we use the same data to seek other potential predictors of informed people wanting to take statins, in addition to their 10-year CVD risk. These analyses are primarily inductive, designed to generate hypotheses about how people make statin decisions. We considered this research important to better understand reasons for statin nonadherence, as well as to help make statin guidelines more patient-centered.
METHODS
Survey Methods
The methods of this survey study have been described previously.4 Briefly, we conducted a Qualtrics survey (www.qualtrics.com) in the spring of 2020 with an online non-probability internet market research panel to achieve a national sample of 309 respondents. People in the Qualtrics internet panel who met the demographic criteria were notified by email about the ability to participate and were provided a link to the survey (Appendix). Participants opted in to complete the survey after reading a consent form, and they received compensation if they completed the survey. Eligible people were aged 40 to 75 who had not taken a statin or PCSK9 inhibitor in the past 3 years, and who knew the results of their total cholesterol (TC), high density lipoprotein cholesterol (HDL), and blood pressure (BP). Quotas were established to ensure diversity based on age, sex, race, ethnicity, and education. Participants were excluded if they were allergic to statins, or if they had a prior CVD event. Each question had a response option indicating they did not want to answer. Quality control checks included setting a minimum amount of time to complete the survey (6 min).
Estimation of CVD Risk
To calculate a personalized estimate of each respondent’s 10-year CVD risk, respondents were asked to enter their age, sex, TC, HDL, systolic BP, treatment for hypertension, whether they had diabetes, and smoking status into an online calculator which used the PCEs to estimate their 10-year CVD risk.5 Since the calculator was publicly available, respondents accessed it through an iframe built into the survey, so they did not leave the secure site. Once the 10-year CVD risk estimate was calculated, participants were instructed to enter the risk value from the calculator as a response in the survey.
Presentation of Statin Benefits and Risks
The risk participants entered was used to generate two icon arrays, one presenting an estimate of their 10-year absolute risk of a CVD event if they did not take a statin and the other an estimate of their absolute risk if they took a statin. Icon arrays were displayed using a denominator of 100. The absolute risk with statin therapy was estimated from a meta-analysis done supporting the US Preventive Services Task Force (USPSTF) 2016 recommendation.6 The point estimate of the relative risk for CVD events from that analysis was 0.72 (95% CI 0.63 to 0.81). We used a 25% risk reduction to simplify calculations and icon array presentations (rounding up to a higher risk estimate when necessary).
Participants were then presented the possible side effects of taking a statin based on meta-analyses of trials where participants took a statin or placebo.7 These harms included severe muscle injury, developing diabetes, hemorrhagic stroke, and other possible side effects. All side effects were displayed using a denominator of 1000. The presentation of harms was conservative, in that only side effects shown to occur more often with statins than placebo in trials were included.
Study Variables
After viewing the information about the benefits and harms, participants were asked about their preferences for taking a statin (definitely take a statin, probably take a statin, probably not take a statin, and definitely not take a statin). Participants were also asked if they had ever talked with a healthcare provider about statin treatment (yes or no) and, if so, what the provider recommended (take a statin, not take a statin, my healthcare provider did not make a recommendation).
Additional variables were collected based on the investigators’ judgments of what factors might influence people’s decisions about statins. To evaluate how informed participants were about taking a statin, they answered four knowledge questions considered by the authors to represent the key facts for an informed decision. Three of the knowledge questions reflected content presented in the survey. A fourth question asked about their personalized 10-year CVD risk without a statin. The correct response for this item was based on their personalized risk generated from the calculator, and response options were categorized as 0–4%, 5–9%, 10–15%, and > 15%; any response in the range including the estimate from the risk calculator was considered correct.
Participants completed a one-item literacy screener that asked how often someone helped them read instructions, pamphlets, or other written material from the doctor or pharmacy; the response options included never, rarely, sometimes, often, or always.8 Participants also completed the 8-item Subjective Numeracy Scale (SNS) to obtain a measure of their perceived ability to perform mathematical tasks. SNS scores range from 8 to 48; higher scores indicate higher perceived ability to perform various mathematical tasks. The scale has been found to be valid and reliable.9
Participants were also asked how big the benefit of taking a statin felt to them (large, medium, small, or almost no benefit), and how worried they were about the possible side effects of taking a statin (very worried, somewhat worried, a little worried, not worried at all). They also completed the single-item maximizer-minimizer scale, which measures the extent to which respondents are predisposed to seek health care (medical maximizers) or prefer to avoid medical intervention (medical minimizers). Scores range from 1 to 6, with higher scores indicating more maximizing tendencies.10 Finally, participants provided demographic information, including age, sex, race/ethnicity, and educational level.
The Mass General Brigham Human Research Committee Institutional Review Board approved this study as exempt.
Statistical Analysis
Descriptive statistics were used to characterize the study sample and their survey responses. Participants who stated they definitely or probably wanted to take a statin were considered as wanting a statin, and those who stated that they definitely or probably did not want to take a statin were considered as not wanting a statin. This binary statin preference variable was used for all analyses. We hypothesized that participants’ feelings about the magnitude of the benefit of statin therapy and worry about the risks would be important predictors of their willingness to take a statin, in addition to the calculated 10-year risk. We planned to correlate the 10-year risk (treated as an ordinal variable based on ordered categories) with participants’ feelings about the magnitude of the benefit using Spearman’s rho. Given prior work indicating a possible inverse relationship between perceptions of risks and benefits,11 we hypothesized that worry about side effects would be inversely related to participants’ feelings about the magnitude of the benefit, and we tested this hypothesis using Spearman’s rho.
We then used a 3-stage hierarchical logistic regression to predict participants’ desire to take a statin as the dependent variable. This approach allows the analysts to add related groups of variables in sequence and compare the discriminatory power of the resultant models. The first stage used 10-year estimated CVD risk to predict wanting to take a statin; our second stage added participant feelings about the magnitude of the benefit and worry about the risks as independent variables. The third stage added other potential predictors with bivariate associations with statin choice (P < 0.10). We compared models using both their R2 statistics and their areas under the operating characteristic (AUC) curve to test their ability to discriminate between participants who did or did not want a statin. Statistical calculations were performed in R version 3.5.2.1.12
RESULTS
Data were collected on 309 participants who completed the survey, but three respondents who did not answer the question about their statin preference were excluded, leaving 306. The survey was completed in a median of 12.3 min (IQR 9.0–17.0). The two longest values (> 5 h) were considered outliers based on z-scores > 3 and were excluded as answering questions at the end of the survey required remembering facts from early in the survey, leaving 304 in the final sample. Given how the web-based market sample was derived, a response rate could not be calculated.
Characteristics of participants were described in detail in our previous report.4 Briefly, participants ranged in age from 40 to 74 with a mean of 55 years (SD = 9.9). Fifty percent were men and 50% were women. Fifty-seven percent self-identified as white, 23% as Asian, 11% as African American, 7% as Hispanic or Latino, and 4% as other or multiple races. Seventeen percent had a high school education or less, 34% had completed some college, and 49% had a college degree. Sixteen percent often or always needed help reading health information. Twenty-six percent of participants reported a prior discussion with a clinician about statin therapy, and in 75% of those discussions, the clinician recommended a statin. Based on self-reports, participants were drawn from 27 different US states.
The mean 10-year CVD risk, as well as median and interquartile range, is presented in Table 1. We also present the proportion of participants with risks in these ordered categories reflecting thresholds often appearing in practice guidelines: 0–5%, 5.1–7.4%, 7.5–10%, 10.1–15%, 15.1–20%, and > 20%. We provide the distribution of participants’ answers to the questions about the size of the benefit and degree of worry about statin risks in ordered categories. When asked their preference for taking a statin after reviewing their benefit and risk information, 45% of the participants reported they would definitely (9.5%) or probably (36.5%) want to take a statin. Total knowledge scores ranged 0–100 with a mean of 55.8 (SD 32.4). Maximizer-minimizer scale scores ranged from 1 to 6 with a mean of 4.02 (SD 1.50). In terms of participants’ perception of the magnitude of benefit from taking a statin, 33% thought there was almost no benefit, 23% a small benefit, 32% a medium benefit, and 12% a large benefit. In terms of worry about the possible side effects 15% were not worried at all, 28% were a little worried, 37% were somewhat worried, and 21% were very worried.
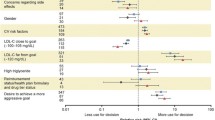
Figures 1a and b present crosstabulations of the ordered categories of estimated risk from the PCE and either perceived magnitude of benefit (Fig. 1a) or worry about risk (Fig. 1b). Participants’ estimated CVD risk categories were significantly correlated with their perceived benefits for taking a statin (rho = 0.29, P < .001), though not so highly to be concerned about multicollinearity in prediction models. We did not find that CVD risk categories were significantly correlated with level of worry about side effects (rho = 0.03, P = 0.59). However, there was a small but significant inverse correlation between participants’ perceived benefit and perceived worry (rho = − 0.22, P < 0.001). In examining Figure 1a regarding the relationship between predicted CVD risk from the PCE and participants’ perceptions of statin benefits, it is notable that for participants with a predicted risk of < 5%, about 33% still thought the benefit of statins was medium (30/118, 25.4%) or large (9/118, 7.6%). Conversely, for a risk > 20%, about 27% thought the benefit of a statin was almost none (9/77, 11.4%) or small (16/77, 16.9%).
a Crosstabulation of participants’ 10-year cardiovascular disease risk category from the pooled cohort equations and their perception of the magnitude of benefit from taking a statin (N = 287 participants with responses to both items). b Crosstabulation of participants’ 10-year cardiovascular disease risk category from the pooled cohort equations and their level of worry about side effects from taking a statin (N = 287 participants with responses to both items).
Bivariate models identified that CVD risk (ordinal categories), perception of benefits, perceptions of worry, discussing statins with a provider, knowledge, age, and literacy were predictive of statin preferences and were included in the hierarchical models (Appendix Table 3). Other examined variables, including gender, race/ethnicity (white, non-Hispanic vs. others), education level, maximizer-minimizer score, health literacy, and subjective numeracy were excluded because of lack of a sufficient bivariate relationship.
Table 2 presents the results of logistic models predicting whether participants would want statin therapy, based on potential predictors identified in the bivariate analyses. In stage 1, we see that CVD risk from the PCE is significantly predictive of statin preference with individuals that have higher risk being more likely to want a statin. However, the ability of the stage 1 model to discriminate between participants who do and do not want a statin is relatively poor (R2 = 0.12, AUC = 0.67). After adding participants’ perceptions of the benefits and worry about side effects of statin therapy in stage 2, we find that perceptions of the benefits of statin therapy were predictive of preference, indicating that those who perceive greater benefits were more likely to want statins, but worry about side effects was not a significant predictor. In stage 2, CVD risk from the PCE remains a significant, though weaker predictor of statin preference, and the discriminating ability of the model improves dramatically (R2 = 0.62, AUC = 0.91). In stage 3, we find adding knowledge, age, literacy, and discussing statins with a healthcare provider are not significant predictors of wanting a statin in the presence of estimated CVD risk, perceptions of benefits, and worry about harms. The discriminating ability of stage 3 (R2 = 0.62, AUC = 0.91) changed minimally from stage 2, and the estimated CVD risk was not a significant independent predictor of statin preference in stage 3. Comparisons of the three models indicate that the addition of perceptions of benefit and worry added in stage 2 resulted in a significant improvement of the model (χ2(2) = 150.2, P <. 001), but addition of the variables in stage 3 did not improve upon stage 2 (χ2(4) = 1.5, P = .83).
DISCUSSION
Practice guidelines routinely suggest clinicians estimate patients’ 10-year risk of a CVD event and then use that estimate to make decisions or have discussions with patients about statin therapy for primary prevention. However, when patients are involved in making decisions about statin therapy, little is known about how they process that risk information, along with information about potential side effects. Our data suggest that people’s qualitative impressions of the magnitude of benefit, rather than the quantitative risk estimates from the PCEs, drive statin decisions. In fact, these qualitative impressions and the quantitative risk estimates were only modestly correlated. In future research in clinical populations, exploration of the “disconnect” between people’s qualitative understanding of statin benefits and quantification of risk deserves further exploration. While many clinicians think patients put excessive weight on the possible harms of statin therapy in making decisions, we did not find worry about side effects was an independent predictor of wanting to take a statin.
Understanding how patients approach the statin decision for primary prevention is critical to addressing the problem of primary and secondary nonadherence to prescribed statins. Between 13 and 34% of patients prescribed a statin never fill it (primary nonadherence),13 while 25–50% of patients who initiate a statin discontinue it over the first year (secondary nonadherence).14 A number of qualitative studies addressing reasons for statin nonadherence identify a variety of factors, but patient doubts about the benefits of statins in the absence of manifest CVD is a common denominator.13,15
The broad distribution of informed patient preferences for statins across the spectrum of CVD risk4 suggests shared decision-making (SDM) between clinicians and patients may be a better approach than choosing arbitrary cut-points on the CVD risk distribution to recommend clinicians prescribe a statin in practice guidelines.16,17 Moreover, in other chronic conditions, such as prediabetes and asthma, shared decision-making around treatment has increased adherence.18,19 How the benefits of taking statins should be presented in an SDM discussion or any accompanying decision support tools to give patients as accurate as possible an impression of the CVD risk reduction possible need further research. Our results suggest presenting quantitative estimates of benefit alone, as we did in our study, may not be enough.
Our study has a number of limitations. First, while our sample of participants was relatively diverse, we do not know whether this internet sample of survey volunteers was representative of the broader patient population who might consider a statin. White and Hispanic or Latino people were underrepresented, while Asian people were overrepresented in our sample, compared to US Census figures.20 Second, our participants were making a hypothetical decision about taking a statin, albeit using their own personalized CVD risk estimate from the PCEs. We plan to replicate this work in a clinical population, ideally with participants who are in an actual “decision window” about taking a statin. Third, our study participants needed a relatively high level of “digital literacy” in order to participate, again raising concerns about generalizability despite the spectrum of health literacy and numeracy represented in our study population. Finally, our presentation of statin side effects was conservative, reflecting only the risks seen more commonly than placebo in trials. If we had instead presented the higher probabilities of potential side effects from observational studies,21 worry about side effects may have played a greater role in our models.
CONCLUSION
We conclude that in this study population, participants’ perceptions of their benefit from statin therapy predicted wanting to take a statin for primary prevention; neither estimated CVD risk nor worries about statin side effects were independent predictors. These findings, if replicated in a clinical population, have implications for addressing statin nonadherence, for shared decision-making about taking a statin for primary prevention, and the construction of practice guidelines taking patients’ preferences into account.
References
Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Statin Use for the Primary Prevention of Cardiovascular Disease in Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;316(19):1997-2007.
Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e596-e646.
O'Malley PG, Arnold MJ, Kelley C, et al. Management of Dyslipidemia for Cardiovascular Disease Risk Reduction: Synopsis of the 2020 Updated U.S. Department of Veterans Affairs and U.S. Department of Defense Clinical Practice Guideline. Ann Intern Med. 2020;173(10):822-829.
Brodney S, Valentine KD, Sepucha K, Fowler FJ Jr, Barry MJ. Patient Preference Distribution for Use of Statin Therapy. JAMA Netw Open. 2021 Mar 1;4(3):e210661. https://doi.org/10.1001/jamanetworkopen.2021.0661. PMID: 33720368; PMCID: PMC7961307.
Kane S. ASCVD Risk Calculator: 10-Year Risk of First Cardiovascular Event Using Pooled Cohort Equations. ClinCalc: https://clincalc.com/Cardiology/ASCVD/PooledCohort.aspx. Updated June 1, 2020. .
Chou R, Dana T, Blazina I, Daeges M, Jeanne TL. Statins for Prevention of Cardiovascular Disease in Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2016;316(19):2008-2024.
Collins R, Reith C, Emberson J, et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet. 2016;388(10059):2532-2561.
Morris NS, MacLean CD, Chew LD, Littenberg B. The Single Item Literacy Screener: evaluation of a brief instrument to identify limited reading ability. BMC Fam Pract. 2006;7:21.
Zikmund-Fisher BJ, Smith DM, Ubel PA, Fagerlin A. Validation of the Subjective Numeracy Scale: effects of low numeracy on comprehension of risk communications and utility elicitations. Med Decis Making. 2007;27(5):663-671.
Scherer, L.D. and Zikmund-Fisher, B.J., 2020. Eliciting medical maximizing-minimizing preferences with a single question: development and validation of the MM1. Medical Decision Making, 40(4), pp.545-550
Alhakami AS, Slovic P. A psychological study of the inverse relationship between perceived risk and perceived benefit. Risk analysis. 1994 Dec;14(6):1085-96.
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing Web site. https://www.R-project.org/. Published 2018.
Tarn DM, Barrientos M, Pletcher MJ, Cox K, Turner J, Fernandez A, Schwartz JB. Perceptions of Patients with Primary Nonadherence to Statin Medications. J Am Board Fam Med. 2021 Jan-Feb;34(1):123-131. doi: https://doi.org/10.3122/jabfm.2021.01.200262.
Ingersgaard MV, Helms Andersen T, Norgaard O, Grabowski D, Olesen K. Reasons for Nonadherence to Statins - A Systematic Review of Reviews. Patient Prefer Adherence. 2020 Apr 2;14:675-691. https://doi.org/10.2147/PPA.S245365. PMID: 32308373; PMCID: PMC7135196.
Ju A, Hanson CS, Banks E, Korda R, Craig JC, Usherwood T, MacDonald P, Tong A. Patient beliefs and attitudes to taking statins: systematic review of qualitative studies. Br J Gen Pract. 2018 Jun;68(671):e408-e419. https://doi.org/10.3399/bjgp18X696365. PMID: 29784867; PMCID: PMC6002012.
Barrett B, Ricco J, Wallace M, Kiefer D, Rakel D. Communicating statin evidence to support shared decision-making. BMC Fam Pract. 2016 Apr 6;17:41. doi: 10.1186/s12875-016-0436-9. PMID: 27048421; PMCID: PMC4822230.
Martinez KA, Rothberg MB. Soliciting Patients to Help Define Treatment Thresholds. JAMA Netw Open. 2021 Mar 1;4(3):e211181. https://doi.org/10.1001/jamanetworkopen.2021.1181.
Moin T, Duru OK, Turk N, Chon JS, Frosch DL, Martin JM, Jeffers KS, Castellon-Lopez Y, Tseng CH, Norris K, Mangione CM. Effectiveness of Shared Decision-making for Diabetes Prevention: 12-Month Results from the Prediabetes Informed Decision and Education (PRIDE) Trial. J Gen Intern Med. 2019 Nov;34(11):2652-2659. https://doi.org/10.1007/s11606-019-05238-6. Epub 2019 Aug 30. PMID: 31471729; PMCID: PMC6848409.
Wilson SR, Strub P, Buist AS, Knowles SB, Lavori PW, Lapidus J, Vollmer WM; Better Outcomes of Asthma Treatment (BOAT) Study Group. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med. 2010 Mar 15;181(6):566-77. https://doi.org/10.1164/rccm.200906-0907OC. Epub 2009 Dec 17. PMID: 20019345; PMCID: PMC2841026.
US Census Bureau. Quick Facts. https://www.census.gov/quickfacts/fact/table/US/PST045219. Accessed September 2, 2020.
Rosenson RS, Baker SK, Jacobson TA, Kopecky SL, Parker BA, The National Lipid Association's Muscle Safety Expert P. An assessment by the Statin Muscle Safety Task Force: 2014 update. J Clin Lipidol. 2014;8(3 Suppl):S58-71.
Acknowledgements
The authors would like to acknowledge the contributions of Floyd J. Fowler, Jr. for his early contributions to the design of the survey.
Disclaimer
Michael J. Barry, MD, is a member of the United States Preventive Services Task Force (USPSTF). This article does not necessarily represent the views and policies of the USPSTF.
Funding
Funded by a grant from Healthwise, a nonprofit patient education and decision support organization, through Massachusetts General Hospital to support the Informed Medical Decisions Program. Healthwise had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, and approval of the manuscript; or the decision to submit the manuscript for publication.
Drs. Barry and Brodney received salary support from this grant. KD Valentine and Karen Sepucha have no relevant disclosures.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior Presentations: None
Supplementary Information
ESM 1
(DOCX 40 kb)
Rights and permissions
About this article
Cite this article
Valentine, K., Brodney, S., Sepucha, K. et al. Predictors of Informed People’s Preferences for Statin Therapy to Reduce Cardiovascular Disease Risk: an Internet Survey Study. J GEN INTERN MED 38, 36–41 (2023). https://doi.org/10.1007/s11606-022-07440-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07440-5